- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
'Repeated' Medical Imaging Test Could Be Exposing Millions To Radiation-Linked Tumors
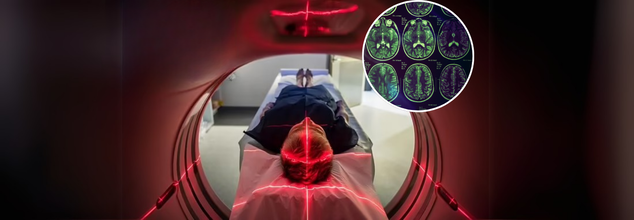
What if the very test meant to save your life could be subtly increasing your risk of cancer? That’s the alarming question emerging from new research on the widespread use of CT (computed tomography) scans—advanced imaging tools that use X-rays to generate cross-sectional views of the body. Often hailed for their ability to catch internal injuries, tumors, and other critical conditions early, CT scans have become a routine part of modern diagnostics. Yet as their use skyrockets globally, so do concerns over the health consequences of repeated and, at times, unnecessary exposure to high doses of radiation.
There’s no denying the clinical value of CT scans. They help detect life-threatening bleeding, guide surgeons during complex procedures, and monitor the progression of diseases like cancer. In the U.S. alone, over 93 million CT scans are performed each year—a number that continues to grow, according to medical market research firm IMV.
But what often goes unnoticed is the invisible cost: radiation exposure.
Unlike conventional x-rays, which emit lower doses, CT scans deliver substantially higher radiation levels. A chest x-ray, for instance, exposes a patient to 0.1 millisieverts (mSv), whereas a chest CT scan delivers around 7 mSv—that’s 70 times more. These numbers are not trivial, especially when stacked up over multiple scans throughout a person’s life.
One of the most concerning revelations from a study led by Dr. Rebecca Smith-Bindman, professor at the University of California, San Francisco, is the staggering inconsistency in radiation doses across CT machines. The dose for the same scan type can vary by a factor of 10 to 15 times, even when used for identical clinical reasons.
“In some cases, one machine could be exposing patients to tenfold more radiation than another,” Dr. Smith-Bindman told NBC News. This lack of regulation means patients could be unknowingly absorbing dangerous levels of radiation, increasing their long-term cancer risk.
Her 2009 study, which analyzed the 11 most common CT scan types in over 1,000 patients, found that radiation doses for an abdominal and pelvic scan could range up to 31 mSv—comparable to about 163 chest x-rays or 160 roundtrip flights between New York and Tokyo.
The link between medical radiation and cancer is not new, but its scale is only now becoming clear. According to findings published in The New England Journal of Medicine, CT-related radiation could be responsible for up to 2% of all cancers—translating to tens of thousands of cases annually.
Dr. Smith-Bindman’s team estimated that one in 270 women and one in 600 men who undergo certain types of CT scans at age 40 may develop cancer as a direct result of the scan. For younger patients in their 20s, the risk doubles.
Radiation has long been associated with cancers such as leukemia, breast, colon, ovarian, bladder, stomach, and lung cancers. With rising CT scan usage and no uniform standard for radiation dosing, experts warn we could be looking at a silent, radiation-fueled cancer epidemic in the coming decades.
Are CT Scans Overprescribed?
Part of the answer lies in defensive medicine—doctors fearing lawsuits may order extra tests “just to be safe.” Financial incentives also play a role; CT scans are among the most expensive diagnostic tools, and hospitals benefit when more of them are used. This creates a dangerous mix of overdiagnosis and overexposure.
A separate long-term study from Brigham and Women’s Hospital in Boston analyzed over 31,000 patients and found that 33% had received more than five CT scans, and 1% had more than 38. In such cases, the cancer risk spiked to over 12% above the national average.
Recognizing the growing threat, the U.S. government is beginning to take action. New Medicare regulations, introduced during the final weeks of the Biden administration, require hospitals and imaging centers to record and share radiation dosage data from CT scanners. These rules will be phased in over three years and could include fines for non-compliance by 2027.
Whether these policies survive under subsequent administrations remains to be seen, but experts agree that standardization of CT scanning practices is urgently needed.
What Patients Can Do Protect Themselves?
While some CT scans are medically necessary and lifesaving, patients can—and should—take steps to minimize unnecessary exposure:
Ask questions: Before undergoing a CT scan, ask your doctor how the results will influence your care. Could a lower-dose scan like an MRI or ultrasound provide the same insight?
Track your imaging history: Keep a personal record of all diagnostic scans you've had. It helps doctors make better-informed decisions and avoid redundant testing.
Consider spacing out scans: If you're undergoing routine imaging for a chronic condition, discuss with your provider whether extending the interval between scans is possible.
Avoid "just in case" scans: CT scans should not be used as reassurance tools in asymptomatic individuals, as they can lead to incidental findings, triggering a cycle of further tests and radiation exposure.
CT scans have revolutionized medical diagnostics and undoubtedly saved countless lives. But with great power comes great responsibility. The lack of regulation, wide dose variation, and rising use of these high-radiation scans call for a reevaluation of when and how they are used.
As science continues to uncover the long-term impact of medical imaging, one thing is clear: it’s time for the medical community—and patients themselves—to weigh not just the benefits, but the hidden risks, of overexposure to radiation.
Pancreatic Cancer: New Study Warns How Your Alcohol Habit Could Be A Date With One Of The World’s Deadliest Cancers

A new study from scientists in Miami has raised a big red flag saying that heavy alcohol consumption does not just damage your liver; it could also be quietly harming your pancreas and paving the way to one of the most lethal cancers in the world. While nobody talks much about this organ, it keeps your show running. Sitting behind the stomach, the pancreas organ produces the digestive enzymes that help you break down food, as well as the hormones that regulate your blood sugar.
The fresh study, published in Cellular and Molecular Gastroenterology and Hepatology, sheds new light on how alcohol-induced inflammation accelerates the development of the deadly disease.
The Miami researchers discovered that alcohol, in high quantities, can damage the very pancreatic cells that make those enzymes. This injury sparks inflammation that can smoulder away until it creates precancerous lesions. Left unchecked, these can evolve into pancreatic cancer, a disease with a grim reputation.
A gene that could save the day
Not everyone who enjoys a tipple is destined for cancer. For the disease to develop, researchers found that a mutation in a gene called Ras, which controls cell growth, must also be present. But when alcohol was paired with a pro-inflammatory molecule in experiments, the effects mimicked alcohol-induced pancreatitis, complete with inflammation, lesions, and cancer.
The breakthrough? By disabling a gene called CREB, the scientists stopped both precancerous and cancerous lesions from forming. In other words, CREB seems to hold the keys to either the safe or self-destruct modes for your pancreas.
Why this matters more now
Pancreatic cancer kills over 9,000 people in the UK and more than 52,000 in the US every year. The five-year survival rate? About 10 to 12 per cent, among the lowest of any cancer. To make matters worse, cases are rising among younger people, though deaths have not yet spiked.
What makes this cancer so deadly is its silence. Symptoms rarely appear until it has already spread, and by then, treatment options are limited.
The stealthy symptoms you should not ignore
- Belly pain that radiates to your back
- Unexplained weight loss and loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Pale or floating stools, dark urine, and itching
- New or worsening diabetes
- Fatigue or weakness
By the time these appear, the disease is often in an advanced stage, which is why prevention is key.
Defining ‘heavy drinking’
The study defined heavy alcohol use as eight or more drinks per week for women and 15 or more for men. Over months and years, that adds up to a consistent assault on your pancreas.
Complications that make life harder
Pancreatic cancer isn’t just fatal; it can also cause a series of painful, exhausting complications:
- Weight loss as the body struggles to absorb nutrients
- Blocked bile ducts leading to jaundice
- Abdominal pain from tumors pressing on nerves
- Bowel obstructions
- Painful swelling in the limbs due to blood clots
Reportedly, managing these often requires procedures like stent placements or even nerve-block injections, adding more physical and emotional strain to an already heavy burden.
How to reduce the risk
- Cut back on alcohol: You do not need to go teetotal overnight, but trimming down your weekly intake could protect your pancreas.
- Quit smoking: Tobacco and alcohol together are really bad.
- Maintain a healthy weight: Extra body fat increases inflammation and strains your pancreas.
- Eat for your pancreas: Load your plate with vegetables, fruit, and whole grains, and keep processed foods to a minimum.
- Stay active: Exercise helps manage weight and lowers inflammation.
Experts Warn Against The Unique Symptoms Of 'Stratus' Covid Strain That Has Infected A Large UK Population; Can It Evade Antibodies?

Credits: Canva
The UKHSA has noted that a new strain of COVID-19 virus, called Stratus, with two variants, XFG and XFG.3, has accounted for a high proportion cases in England, reports the Independent. Among these two variants, XFG.3 has accounted for 30% of cases in the country.
However, experts have suggested to not panic on the arrival of this new strain. Dr Alex Allen, consultant epidemiologist of UKHSA said, "It is normal for viruses to mutate and change over time," as reported by the Independent. However, the UKHSA has also confirmed that it continues to monitor all strains of COVID in the UK. For now, experts are not concerned over the spread.
What Is Stratus XFG and XFG.3?
As per the World Health Organization (WHO), XFG is a "variant under monitoring" and that any health risk posed by this variant remain low at the global level.
As of now, globally, XFG has the highest relative growth when compared to the other variants that are currently active and circulating, including "Nimbus" NB.1.8.1.
Also Read: World Organ Donation Day 2025: Theme, History, And Importance
The WHO also confirmed that current data does not indicate that this variant leads to more severe illness or deaths than the other currently active variants in circulation.
Unique Symptoms Of Stratus COVID Strain
While the strain is said to be not a cause of concern, the symptoms may be unique from what we traditionally know COVID symptoms to be.
The WHO however, time and again has said that there is no increase in severity. It said, "While there are reported increases in cases and hospitalisations in some of the [South-east Asia Region] countries, which has the highest proportion of XFG, there are no reports to suggest that the associated disease severity is higher as compared to other circulating variants."
Dr Allen also seconded the opinion and said, "Based on the available information so far, there is no evidence to suggest that the XFG and XFG.3 variants cause more severe disease than previous variants, or that the vaccines in current use will be less effective against them.”
The unique symptoms of Stratus COVID strain includes:
- Sore throat or hoarseness, as experts have also claimed that Stratus can give patients a "hoarse voice".
- Headaches that can last several days
- Nasal congestion and mild fever
- Fatigue that lingers beyond acute phase
Other than these unique symptoms, the common COVID symptoms like change in smell or taste, shortness of breath and chest discomfort remain, however, it may be uncommon in vaccinated individuals.
Are There Any Risks Around The New Stratus Strain?
XFG is growing rapidly compared to co-circulating variants globally. However, XFG exhibits only marginal additional immune evasion over [other varient] LP.8.1. While there are reported increases in cases and hospitalizations in some of the [South-east Asia Region] countries, which has the highest proportion of XFG, there are no reports to suggest that the associated disease severity is higher as compared to other circulating variants. The available evidence on XFG does not suggest additional public health risks relative to the other currently circulating Omicron descendant lineages," said WHO.
Do We Need New Vaccines For The New Strain?
The WHO said that as per the current available data, the currently approved COVID-19 vaccines are expected to remain effective against symptomatic and severe diseases, including caused by the new strain.
However, Dr Kaywaan Khan, Harley Street GP and founder of Hannah London Clinic told Cosmopolitan UK that due to certain mutations in the spike protein in Stratus strain, it could evade antibodies "developed from prior infections or vaccinations".
While WHO noted that the risk of vaccine evasion is low, it also noted that more studies must be added to assess the risk of antibody escape.
World Organ Donation Day 2025: Theme, History, And Importance
Credits: Canva
Every year, on August 13, World Organ Donation Day is observed, globally, to spread awareness about the importance of organ donation and to make people aware about the misconceptions that surround organ donation.
World Organ Donation Day 2025 Theme And Significance
This year's theme for World Organ Donation Day is 'Answering the Call'. This theme highlights the important function played by the professionals in the organ donation community. What it means is to encourage more to strengthen their dedication to save as many lives as possible through organ donation and transplantation.
The Pace Hospital notes that as of 2021, globally, 1,44,302 organ transplantations had occurred, of which, 26.44% were of deceased organ donation. India performed a total of 12,259 transplantation, contributing to 8% in global transplantations. In India, the most transplants that took place were for kidneys at 74.27%, liver at 23.33%, heart at 1.23%, lung at 1.08%, pancreas at 0.15%, and small intestine at 0.03%.
The overall number of deceased donors transplantation in India was 4.5%. While the deceased donors transplantation in India was reported 759 for kidney, 279 for liver and 99 for heart, the Indian Ministry of Health's estimated that it needs 175,000 kidneys, 50,000 livers, hearts, and lungs and 2,500 pancreas to meet the demand.
The Indian Ministry of Road and Transport and Highway's 2021 report notes that more than 1.5 lakh were reported as accident-related mortalities, however, only 552 deceased brain deaths organ transplantations took place in 2021. This is why it is more so important to raise awareness about organ donation to help those in requirement and reducing the number of patients on the waiting list.
History Of Organ Donation
It was in 1954, when the first successful organ transplant was performed. It was a kidney transplant by Dr Joseph Murray and his team at Peter Bent Brigham Hospital in Boston, Massachusetts.
The donor was Ronald Lee Herrick, who donated his organ to his twin brother Richard Herrick. Later in 1990, the doctor was honored with Nobel Prize in Physiology and Medicine for bringing advances in organ transplantation.
Th United Network for Organ Sharing (UNOS) highlights the timeline of the first donations and transplants performed of different organs.
- 1996: First simultaneous kidney and pancreas transplant performed.
- 1967: First successful liver transplant performed.
- 1968: The Southeast Organ Procurement Foundation implemented the first computer-based organ matching system, which was dubbed as UNOS. It successfully performed the first isolated pancreas transplant and heart transplant.
- 1981: First successful heart-lung transplant performed.
- 1983: First successful single-lung transplant performed. Cyclosporine, the first of a number of drugs that effectively treat organ rejection by suppressing the human immune system, introduced.
- 1984: National Organ Transplant Act (NOTA) was passed.
- 1986: First successful double-lung transplant performed.
- 1987: First successful intestinal transplant performed.
- 1988: First split-liver transplant performed.
- 1989: First successful living donor liver transplant performed.
- 1990: First successful living donor lung transplant performed.
- 1992: UNOS helped found Donate Life America to build public support for organ donation.
- 1998: First successful adult-to-adult living donor liver transplant performed.
How Organ Donation Can Change A Life?
In March 2024, a dedicated Delhi-based teacher, Meena Mehta was declared brain dead and her organs were donated to many, including her hands, shared her nephew Jawed Mehta. A 45-year-old Delhi-based painter had lost both his hands in a 2020 train accident, who received hand transplant. The hands were of Meena Mehta. After a 12-hour long surgery, the painter was able to paint again. Meena Mehta also donated her kidney, liver, and corneas, which has changed lives of three more people.
© 2024 Bennett, Coleman & Company Limited

