- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Researchers Discover Mifepristone Alternative Amid Legal Battle On Abortion Pills

Abortion Pills (Credit: Canva)
US Supreme Court overturned the landmark Roe v. Wade decision in 2022, removing federal protection for abortion rights and allowing individual states to determine their abortion laws. This allowed many states to make medical termination of pregnancy completely illegal. Complicating things further, many states put a near ban on abortion pills, including Mifepristone (14 total states). Just recently, multiple states appealed in the country's top court for a complete ban on these pills. However, the justices ruled that the plaintiffs—a group of anti-abortion doctors and activists—did not have the legal standing to sue. Regardless, it left an opening for three states—Missouri, Kansas, and Idaho—to potentially revive their legal challenges on a total ban on Mifepristone pills.
But Why Mifepristone?
Mifepristone is a drug that blocks progesterone, a hormone essential for pregnancy to continue. When used in combination with another medicine, misoprostol, can terminate an intrauterine pregnancy within 10 weeks of gestation (70 days or less from the first day of the last menstrual period).
A New Alternative
As the legal battle continues, a recent study has identified an alternative to mifepristone, offering new hope to women. The research suggests that ulipristal acetate, the active ingredient in emergency contraception pills like ellaOne, could be used as a substitute for Mifepristone.In the study, 133 women up to nine weeks pregnant were given a 60-milligram dose of ulipristal acetate followed by misoprostol 24 hours later. For 97% of participants, this combination successfully induced abortion—a rate comparable to the effectiveness of the mifepristone-misoprostol regimen. Four participants required additional procedures or medications to complete the abortion.
The 60-milligram dose of ulipristal used in the study is double the standard dose found in ellaOne, which is commonly used for emergency contraception. According to the manufacturer of ellaOne, the drug is designed to prevent pregnancy and does not terminate an existing one. When used as emergency contraception, ellaOne is effective up to five days after unprotected sex. While further research is needed to concretize the discovery, if it works, then ulipristal acetate could become a magic pill for women with unwanted pregnancies.
How Do Abortion Pills Work?
Abortion pills are a combination of two medications- mifepristone and misoprostol, which are consumed in two separate doses. The person may experience cramping and bleeding within a few hours of taking the second medication. This is an indicator that it has worked. The combination of pills is a safe and reliable way to end a pregnancy up to about 12 weeks after the first day of your period. This process can take somewhere between 2 to 3 days to complete, however, symptoms can last for a few weeks. Passing large blood clots may indicate that the embryonic or fetal tissue is exiting your body. Cramping occurs so your uterus can shrink back to its original size. This procedure could be carried out at home. However, a follow-up appointment is suggested to get reassurance.
If you are not aborting at home with the help of the pill, an ultrasound is likely to be performed and you will be given a dissolving tablet that is placed in your vagina, under your tongue or between your cheek and teeth. This will lead to bleeding within 4 hours.
Superbug Alert: Drug-Resistant Typhoid Fever Returns as a Growing Global Threat
Credits: iStock
Typhoid fever, to many sound like it now belongs to history books, but a new strain that can resist strongest of antibiotics have emerged in South Asia. This has raised the concerns over the potential spread of drug-resistant infections.
A gene, which is capable of breaking down carbapenems, which is a powerful antibiotics was seen as a drug of last resort, is discovered among 32 samples collected from hospitals, across western and southern India. This gene is known as blaNDM-5, which can move between different types of bacteria, raising fears that resistance could in fact grow quickly.
Recent outbreaks of extensively drug-resistant (XDR) typhoid across South Asia have raised serious concerns, as these strains no longer respond to most commonly used antibiotics. Since 2016, Pakistan alone has reported over 15,000 XDR typhoid cases, while resistance to azithromycin has been detected in Bangladesh, India, Nepal and other neighboring regions.
Speaking to the Telegraph, Dr Malick Gibani, Clinical Lecturer in Infectious Diseases at Imperial College London, said, “We all hear that antimicrobial resistance is a problem, but typhoid really exemplifies it – how resistance seems to emerge relentlessly, moving from one class of antibiotics to the next."
“It’s not yet untreatable, but the treatments we do have are much more limited and significantly more challenging to deliver.”
What Is Typhoid?
Typhoid is caused by the bacteria Salmonella Typhi. It usually spreads through contaminated food or water and can lead to high fever, stomach pain and serious complications if not treated on time.
Antibiotics are the first line of treatment. These range from commonly used medicines such as amoxicillin and co-trimoxazole to stronger, hospital-only drugs for resistant infections, including carbapenems. Without timely treatment, typhoid can turn life-threatening and, in some cases, prove fatal. What has alarmed researchers is the emergence of typhoid strains that can resist even carbapenems.
“Although the number of cases described is still relatively small, this feels very much like a warning sign,” said Dr Gibani. “This was always expected and reflects the steady evolution of antimicrobial resistance in typhoid. These infections are not untreatable yet, but they are becoming increasingly difficult to manage.”
Experts point out that typhoid is often difficult to diagnose. This uncertainty can lead to the widespread and sometimes unnecessary use of antibiotics, which further fuels resistance. There are also concerns that extensively drug-resistant typhoid may be more widespread than current data suggests, especially in low-income countries where surveillance and reporting are limited.
“The risk is highest in places with poor water quality, uncontrolled antibiotic use and weak healthcare systems,” said Prof Calman A. MacLennan from the University of Oxford. He noted that while current typhoid mortality is under one percent, the disease was far deadlier before antibiotics were available. “In the pre-antibiotic era, death rates were as high as 10 to 20 percent, and during some wars, more people died of typhoid than from combat.”
Best Line Of Defense Against Typhoid
Vaccination, experts say, could be key to preventing a resurgence. The Typhoid Conjugate Vaccine, or TCV, has shown strong effectiveness by triggering the body’s immune response rather than targeting the bacteria directly with antibiotics. “That makes it much harder for the pathogen to escape,” Prof MacLennan explained.
The vaccine has already been introduced into national immunization programmes in 11 countries. However, reaching the poorest regions, where typhoid is most common, remains a challenge. Rolling out a new vaccine requires significant planning and resources, even with international support.
Dr Gibani warned that although South Asia has been hit hardest so far, drug-resistant typhoid can spread globally through travel. Imported cases have already been reported in Europe, North America and Australia. Experts stress that surveillance, vaccination and better sanitation are critical to stopping these dangerous strains from taking hold elsewhere.
Children Getting Fewer Vaccine May Be A 'Better Thing', Says RFK Jr, As US Struggles With Rise In Flu Activity
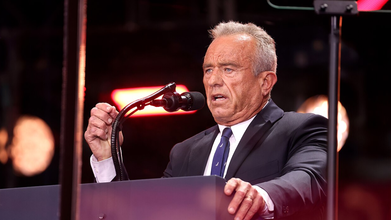
Credits: Wikimedia Commons
"May be it is a better thing that fewer children are receiving the flu vaccine," said Robert F Kennedy Jr, the Health and Human Services Secretary of the United States as the country fights with a surge in flu cases. RFK Jr said this in a response to a CBS News journalists' concern over rising flu cases and the drop in the number of flu vaccines.
This week, the Centers for Disease Control and Prevention (CDC) announced vaccines to fight respiratory syncytial virus or RSV, meningococcal disease, flu, and COVID are the only recommended jabs for children at high risk of serious illness or must be administered after being consulted with doctors and parents. This is part of the CDC and Trump administration's effort to scale back the childhood vaccine scheme.
In an interview with the CBS News, RFK Jr. said, "We are not taking vaccines away from anybody. If you want to get the vaccine, you can get it. It is going to be fully covered by insurance, just like it was before." However, now, there is an added step. Vaccines that were compulsory before now requires a consultation with the physician first. "You have to, yeah, you need to do shared decision making with your physician, which is how it ought to be," he said.
Fewer Flu Vaccine Could Be A Better Thing: TFK Jr, Is There Evidence?
The CBS News reporter asked if there is any evidence that fewer kids getting the vaccine is actually a "better thing" The reporter also pointed out that many kids died of flu last year and that no evidence shows that the kids who died were vaccinated. In fact, a roughly 90% of kids who died from the flu in 2024 were not vaccinated, showed the CDC data.
To this, Kennedy quoted a Cochrane Collaboration study. It is a UK-based health care research nonprofit, which he called, "one of the ultimate arbiters of vaccine safety and clinical data". As per him, the study is an extensive meta review of the flu vaccine. Kennedy said that the study found "there is no evidence that the flu vaccine prevents serious disease or that it prevents hospitalizations or death in children.
However, the medical community does not respect this. In fact, the CDC itself has cited from various studies, including a 2020 and 2017 study from Pediatrics journal, and a 2022 and 2014 study from the journal of Clinical Infectious Diseases, which is an official publication of Infectious Diseases Society of America, and found that vaccines in fact prevented severe and life-threatening complications in children from the flu.
The CDC notes: "ACIP recommends any licensed, age-appropriate flu vaccine for children without preference for any one flu vaccine over another. In several studies, flu vaccine effectiveness was higher among children who received two doses of flu vaccine the first season that they were vaccinated (as recommended) compared to "partially vaccinated" children who only received a single dose of flu vaccine."
However, Kennedy is fixed at his opinion that "here is no scientific evidence that the flu vaccine prevents serious illness, hospitalizations, or death in children."
Becky Quick Speaks About Her Daughter’s Genetic Disorder —What The Diagnosis Is About

Credits: AP
Becky Quick recently spoke about her 9-year-old daughter Kaylie’s private struggle with a rare genetic disorder. In an interview with People, published Thursday, January 8, the 53-year-old co-anchor of CNBC’s Squawk Box revealed that Kaylie has SYNGAP1. According to the Child Neurology Foundation, SYNGAP1 is a genetic condition that can cause seizures and developmental challenges. Quick recalled that she first noticed something was off “probably around 8 months,” when Kaylie wasn’t reaching her developmental milestones.
“Sometimes her eyes would cross. You just know as a mom that something isn’t right,” Quick told People, adding that after observing her daughter and reviewing developmental studies, it became clear that Kaylie wasn’t meeting expected benchmarks. “We immediately began working with therapists. They supported Kaylie in rolling over, achieving fluid movements, eventually walking, and so many other skills. But we also noticed additional concerns developing.”
Becky Quick Daughter Battles SYNGAP1
For nearly a decade, Quick has kept her daughter Kaylie’s SYNGAP1 diagnosis private. The condition, as defined by the Children’s Hospital of Philadelphia, is a rare genetic disorder that can lead to a variety of neurodevelopmental challenges. It currently has no cure and often requires round-the-clock care.
The journalist took Kaylie to her pediatrician, who recommended a study with a developmental specialist. The results confirmed Quick’s fears: her daughter was not reaching key milestones.
“We started working with therapists immediately,” Quick said. “[They] helped Kaylie develop rolling, fluid movement, eventually walking, and many other skills. But we also observed additional issues.”
A neurologist then performed an EEG study, which revealed that Kaylie was experiencing subclinical seizures — subtle seizures that aren’t visibly noticeable. A subsequent genetic test confirmed that Kaylie had SYNGAP1.
What Is SYNGAP1?
SYNGAP1 (SRD) refers both to a gene and the rare neurological disorder it causes. The condition is marked by intellectual disability, epilepsy, and autism spectrum traits, arising from a mutation that reduces the SynGAP protein, which is essential for proper synaptic function in the brain, according to MedlinePlus. Without adequate SYNGAP1 protein, synapses become overly excitable, impairing communication between neurons and leading to the neurological difficulties observed in SYNGAP1 patients, as per National Institute of Health.
Becky Quick Daughter: What Are The Symptoms Of SRD?
SYNGAP1 is considered a spectrum disorder, meaning patients experience symptoms differently and with varying severity. The exact factors influencing symptom expression or intensity remain unclear. The most commonly observed signs include, as per NIH:
- Intellectual Disability (mild to severe)
- Hypotonia (low muscle tone)
- Global Developmental Delay
- Epilepsy (including subtle eyelid flutters, brief jerks, staring spells, and drop seizures)
- Sensory Processing Disorder
- Delays in Gross and Fine Motor Skills
- Dyspraxia (coordination difficulties)
- Speech Delay/Apraxia (mild to severe)
- Autism Spectrum Disorder
- Sleep and Behavior Disorders
- Visual Abnormalities
- Not every patient will exhibit all of these symptoms.
Becky Quick Daughter: What Causes SRD?
SYNGAP1-related disorders arise from a variant on the SYNGAP1 gene (6p.21.32). Each human cell contains 23 pairs of chromosomes, totaling 46, with thousands of genes on each chromosome. Most genes come in pairs, one inherited from each parent, and their primary role is to produce proteins that regulate tissues and organs.
When a gene experiences a variant, sometimes called a mutation or alteration — it can stop functioning properly. Variants occur naturally, similar to a typo when DNA is copied from cell to cell, or they may result from environmental factors.
A de novo variant is a genetic change that appears for the first time in a family, occurring early in reproductive development. Most SYNGAP1 patients carry de novo variants. For families with a genetic report, understanding the variant can help clarify the diagnosis and guide next steps.
© 2024 Bennett, Coleman & Company Limited

