- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
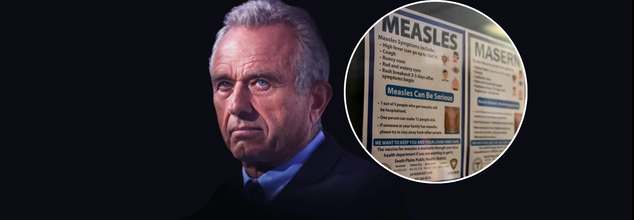
RFK Jr. Urges People To Get Measles Vaccination, 'Didn’t Know’ The Impact Of His Research Cuts
Once considered nearly eradicated in the United States, measles is making a troubling comeback. As of early April, nearly 600 confirmed cases have been reported across multiple states, with Texas emerging as the outbreak’s epicenter. The resurgence of this highly contagious, vaccine-preventable disease is being linked to declining immunization rates, misinformation surrounding vaccines, and weakened public health infrastructure following recent federal budget cuts.
Experts warn that unless aggressive intervention strategies are employed—including increasing vaccination coverage and restoring epidemiological support—the current outbreak could not only persist for months but also jeopardize the U.S.'s measles elimination status achieved in 2000.
In a candid and critical moment of reflection, U.S. Health Secretary Robert F. Kennedy Jr. urged Americans to get vaccinated against measles, even as he admitted on national television that he was unaware of the full impact of significant public health funding cuts enacted during his early tenure. The statement comes amid one of the largest measles outbreaks in recent U.S. history—now spanning multiple states and threatening to reverse decades of progress in infectious disease control.
As of this week, over 595 cases of measles have been confirmed across Texas, New Mexico, Oklahoma, and Kansas. Texas has borne the brunt of the outbreak with 505 cases reported in 21 counties, including urban spillovers that concern local officials. New Mexico has reported 56 cases, Oklahoma 10 (with two still under investigation), and Kansas 24, some of which are believed to be linked to the same source.
The outbreak’s epicenter is Gaines County, Texas—a rural region with low vaccination coverage and limited public health infrastructure. Public health authorities are scrambling to contain the virus, which is known for being highly contagious—transmissible to 90% of unvaccinated individuals in proximity to an infected person.
In his first network television interview since joining President Donald Trump’s cabinet, RFK Jr. sat down with CBS News’ Dr. Jon LaPook for a revealing conversation that quickly became the focus of nationwide scrutiny.
LaPook confronted Kennedy with the administration’s decision to implement $11 billion in cuts to programs targeting infectious diseases, childhood vaccinations, mental health, and addiction support.
“You proposed more than $11 billion in cuts... Did you personally approve those cuts?” asked LaPook.
Kennedy replied, “I’m not familiar with those cuts… Those were mainly DEI cuts, which the president ordered.”
LaPook countered with a specific example, “About $750,000 of a University of Michigan grant into adolescent diabetes was cut. Did you know that?”
“I didn’t know that, and that’s something that we’ll look at,” Kennedy responded, acknowledging that while some reinstatements had occurred, important studies may have been unintentionally defunded due to the sweeping nature of the restructuring.
The CDC’s local partnerships and lab capacities have been severely strained by the budget reductions. Several local health departments, particularly in Texas and New Mexico, have stated that their ability to track, test, and isolate measles cases has been weakened due to the loss of funding and trained personnel.
These challenges are compounded by HHS restructuring, which has resulted in the layoff of more than 10,000 employees under a new directive led by Kennedy in collaboration with the Musk-supported Department of Government Efficiency (DOGE).
“HHS’s job is to make America healthy. We’re spending $1.9 trillion a year and people are not getting healthy,” Kennedy said during the interview. “When you do a disruption of this scale… you may make mistakes in 20% of cases, and then you go back and fix them.”
Yet critics argue that the stakes are too high to risk such large-scale experimental reforms, especially in areas concerning communicable diseases.
Despite his controversial past as a prominent vaccine skeptic, Kennedy used the same interview platform to strongly endorse measles vaccination—a surprising but much-needed pivot.
“We are urging all families in outbreak areas to ensure their children are vaccinated with the MMR vaccine,” Kennedy said, echoing guidance issued by the CDC earlier this week.
The Texas Department of Health Services is now encouraging parents in outbreak zones to get the second MMR dose for children aged 1–4 as soon as possible. Infants between 6–11 months are also eligible for an early dose, with two more to follow on the standard schedule.
The CDC emphasized that 12% of all measles cases this year have required hospitalization, making the situation even more urgent. Experts warn that if the outbreak continues for over 12 months, it could jeopardize the measles elimination status the U.S. achieved in 2000.
The outbreak has cast a spotlight on the fragile state of public health infrastructure, and Kennedy’s remarks have amplified the debate around how to fund and manage it effectively. Though he has promised to revisit specific defunded studies, public health experts remain cautious.
“What we need now is a full restoration of support—not just funds, but trust,” said Dr. Erin Thomas, an infectious disease specialist based in Houston. “These cuts sent a message that infectious disease prevention was no longer a national priority. This outbreak is the direct consequence.”
The statement by the Department of Health and Human Services last week, calling COVID-19 a “non-existent pandemic” and labeling response efforts as wasteful spending, further illustrates the administration’s departure from traditional public health principles.
India’s Antacid Habit Is Putting Hearts, Kidneys, Guts, and Bones at Risk

Credits: iStock
Indians are popping antacids like candies, and they are putting their hearts, kidneys and gut health at risk. Doctors from time and again have cautioned patients to not take such pills without prescriptions.
Antacids are prescribed proton pump inhibitors or PPIs, used commonly to reduce the amount of acid in the stomach and helps to treat and prevent various acid related conditions. However, in India, acidity is not treat as a symptom, but a lifestyle condition, which has made these pills so common. These over the counter access also created medical complacency, this means the availability has blurred the line between short term relief and long term therapy.
How does antacid impact your kidney health?
Repeated use is increasingly associated with acute interstitial nephritis and chronic kidney disease. What makes this dangerous is that kidney damage often develops silently, discovered only when kidney function has already deteriorated significantly.
How does antacid impact your gut health?
It also impact the gut microbiome, and causes chronic digestive problems. Stomach acid regulates gut bacteria. Suppressing it allows harmful bacteria to flourish, leading to bloating, infections, diarrhea, and conditions like small intestinal bacterial overgrowth (SIBO).
How does antacid impact your bone health?
Furthermore, regular usage of antacids could make your bones weak too. As per a 2023 study published in the journal BioMed Research International, pantoprazole cause bone loss, which could be prevented by adding octreotide.
The study analyzed the serum levels of calcium, phosphorus, and ALP before starting the treatment, and at the end of 12 weeks of treatment on pantoprazole, significant decline in calcium levels were noticed, as compared with other groups. The study also found that octreotide significantly prevented the effect of pantoprazole on the serum levels of calcium and ALP.
The study also found that pantoprazole decreased femoral bone density and femoral BMAD. Besides this, another decrease was found in the femoral bone weight and volume as well as the trabecular volume.
How does antacid impact your heart health?
Frequent heartburn is also a symptom of gastroesophageal reflux disease or GERD. This is a condition in which the valve between the stomach and the lower esophagus malfunctions and allows stomach acid to bubble up into the esophagus. This is often treated with antacid, which may mask the real problem.
Over time, untreated GERD can injure the lining of the esophagus and increase the risk of serious complications, including Barrett’s esophagus, a condition that can raise cancer risk. Also, symptoms often blamed on heartburn, such as chest pain or burning, can sometimes signal a heart attack. That’s why experts stress getting a proper medical evaluation before self-treating with antacids.
The safer alternatives are:
Famotidine (Pepcid, Calmicid, Fluxid, Mylanta AR) is a potent H2 blocker used to manage acidity and heartburn. Studies show that famotidine is not thought to raise the risk of osteoporosis.
Other options: Ranitidine (Zantac - where available, as it was withdrawn in some markets due to safety concerns) and Nizatidine are other H2 blockers.
Note: Health & Me do not encourage discontinuance of any prescribed medicine by a doctor. Before making any change in your medicine schedule, please speak to your doctor/GP.
Nasal Spray Warning Over 'Rebound Congestion'; Experts Say It Should Not Be Used For More Than 7 Days

Credits: iStock
Nasal spray warnings are given by doctors and experts as the long use of it could lead to worsening of condition. The Royal Pharmaceutical Society (RPS) advised the public to not use nasal decongestant for more than seven days, as it contains xylometazoline or oxymetazoline. Its prolonged use can cause 'rebound congestion' or increased dependency on these sprays to breathe easily.
A recent poll, reports the Independent found out that almost six in 10 pharmacists report patients were unaware of the dangers of its extended use. Due to the increased number of flu activity, symptoms like blocked nose has increased, which has lead to a high usage of nasal spray.
Is Rebound Congestion Preventable?
It is a preventable condition, and is scientifically known as rhinitis medicamentosa, which causes the symptoms to worsen. Patients become depended on the sprays to breathe more easily.
RPS survey of 300 pharmacists found that 59% think the public is not aware of the risks, while 75% said packaging should be clearer about the seven-day limit. 63% said they had intervened in cases of suspected overuse.
Professor Amira Guirguis, chief scientist at RPS told the ITV News, "Nasal decongestant sprays can be helpful for short-term relief, but using them for longer than seven days can make your congestion significantly worse. Our research shows that many people are unaware of this risk, which means they may continue using these sprays without realizing they could be prolonging their symptoms. We'd like to see clearer warnings on the packaging which you can't miss and greater awareness of the seven-day limit. If your congestion lasts more than a week, speak to your pharmacist. There are safe and effective alternative options to help you manage your symptoms."
Another survey by ITV News suggests that more than a fifth of adults have used the products for longer than seven days. This means 5.5 million people in the UK may have risked developing a dependency.
Read: Bristol Hospitals Under Severe Strain as Flu and Cold Weather Hit the Region
As ITV News reported, Charlotte Johnstone, who is 30, had been using nasal spray multiple times a day since she was seven years old. She realized that the impact of this so-called addiction has caused her anxiety and left her "dreaming about not being able to breathe". She told ITV News, “I can’t sleep without having it, I wake up and the first thing I do is have my nasal spray. I don’t like eating if I’ve got a blocked up nose, it just makes me feel claustrophobic. I wouldn’t put myself in a situation where I don’t have it. “I go through stages of losing my sense of smell. I know it’s doing something but I don’t know what. But for the sake of having a clear nose, I’ll just take it,” she said.
A spokesperson from PAGB, the consumer healthcare association representing the manufacturers of these products, said: “The patient information leaflet which accompanies all nasal decongestant sprays, includes these instructions and outlines the risks of taking the medication for longer than its indicated use. As explained on the information supplied with the nasal decongestant sprays, OTC medicines manufacturers provide comprehensive accessible information to support people to make responsible informed decisions about the right product to self-care for their self-treatable condition," reported ITV News.
ChatGPT Health Explained: Will This New OpenAI Feature Replace Doctors?

Credits: iStock
Open AI launched a new ChatGPT feature in the US, called the ChatGPT Health. As of now, this is launched only in the United States, which can analyze people's medical records and give them better answers. However, it has also drawn attention of critics, who raise concerns regarding the privacy, as well as safety of diagnosis and treatment.
What Is ChatGPT Health?
As per the Open AI website, "Health is a dedicated space in ChatGPT where you can ask health and wellness questions and choose to connect your health data (like medical records and wellness apps) so responses can be grounded in that context. It is designed to support, not replace, medical care."
One can access Health from the sidebar and can ask health-related questions in a main chat. OpenAI has said that the conversations in ChatGPT Health would be stored separately to other chats and would not be used to train its AI tools. The feature will also not be used for "diagnosis or treatment".
However, Andrew Crawford, of US non-profit the Center for Democracy and Technology, as reported in the BBC said, it was "crucial" to maintain "airtight" safeguards around users' health information. "New AI health tools offer the promise of empowering patients and promoting better health outcomes, but health data is some of the most sensitive information people can share and it must be protected," Crawford said.
Why Is This Feature Being Introduced?
OpenAI notes that more than 230 million people ask its chatbot questions related to health and wellbeing, at least every week. Thus the feature is being launched, while ChatGPT Health will have "enhanced privacy to protect sensitive data".
Open AI also noted that users can connect it with third party wellness apps to get the data, for instance Apple Health, Peloton, and MyFitnessPal. These apps can provide the medical records to OpenAI's new feature to generate relevant responses.
In a blogpost, Open AI noted: "You can securely connect medical records and wellness apps to ground conversations in your own health information, so responses are more relevant and useful to you. Designed in close collaboration with physicians, ChatGPT Health helps people take a more active role in understanding and managing their health and wellness—while supporting, not replacing, care from clinicians."
Will This Feature Replace Doctors?
OpenAI claims that ChatGPT Health is not launched to replace medical care, rather to help one navigate everyday questions and understand patterns over time. OpenAI claims that the tool was developed in close collaboration with physicians.
In the last two years, OpenAI said that it was able to work with more than 260 physicians across 60 countries and dozens of specialities, who have provided feedback on model outputs more than 600,000 times.
While the feature is only launched in the United States, however, the company said that it plans to make Health available to all users on web and IOS "in the coming weeks" as the experience is refined.
© 2024 Bennett, Coleman & Company Limited

