- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Scientists Develop Device That Helps Humans 'See In Dark'—Even With Eyes Closed

Credits: Canva
In a scientific breakthrough that blurs the line between fiction and medicine, Chinese scientists have developed soft, invisible contact lenses that allow humans to see near-infrared light—a hitherto invisible spectrum to the naked eye. This innovation is not only non-surgical but also effective in complete darkness, even with the eyes closed. The results from the study, which were released in the high-profile journal Cell, represent a major advance in wearable "super-vision" technology that can potentially revolutionize medical imaging, search and rescue, and vision aid for the blind.
Human eyes are biologically restricted to detecting only wavelengths of light between 400 and 700 nanometers—a slim range that accounts for only a part of the electromagnetic spectrum. Yet, near-infrared light, from 700 to 2,500 nanometers, penetrates more deeply and harmlessly through biological tissues, holding immense promise in the fields of early disease detection and non-invasive imaging.
Directed by University of Science and Technology of China neuroscientist Dr. Tian Xue, the scientists aimed to design a lens that would be able to overcome such natural restrictions. The solution lies in rare earth nanoparticles—tiny particles with the ability to absorb invisible infrared light and re-transmit it as visible red, green, or blue light. These nanoparticles, namely sodium gadolinium fluoride doped with ytterbium, erbium, and gold, were designed to operate safely and effectively within soft contact lenses.
How These Lenses Work?
This is not the first time the research group has made infrared vision more than just a fantasy. Previously, in previous experiments, they directly injected infrared-sensitive nanomaterials into the retinas of test animals, offering them night vision for a limited time. But because retinal injections were so invasive, attention soon turned to a less invasive approach: contact lenses.
By dispersing the nanoparticles of rare earth into polymer solutions that are biocompatible with human eyes, the researchers were able to create ultra-thin, see-through lenses. The lenses were tried out in mice and then in human volunteers. Tests proved that the wearers could identify flickering infrared radiation, recognize infrared patterns, and even decipher temporal codes—even though the light itself was completely undetectable by the human eye when it is not covered by lenses.
One surprising development? Human subjects showed even stronger definition in picking up infrared light when their eyes were shut. In the opinion of Dr. Xue, "Near-infrared light penetrates eyelids more efficiently than visible light, allowing for improved signal detection with eyes shut—free from visible light interference."
Seeing What the Naked Eye Misses?
Older night-vision goggles, introduced during World War II, use electronic image intensifiers and need lots of power to run. These goggles are big, give off greenish images, and usually have difficulty identifying finer details at longer wavelengths of infrared. The newly created lenses, however, work without the need for an external power source and provide a more natural visual output. They are so light and transparent that they are potential rivals for real-life, everyday use in troublesome visual conditions such as fog, dust, or nighttime.
Can These Lenses Assist the Color Blind to See Better?
Although currently in the proof-of-concept phase, this technology's applicability is vast and extensive. The following are some of the possible uses:
Medical imaging: Increased visibility of tissues during surgery or scans
Vision enhancement: Aiding people with visual deficiencies or color blindness
Security & surveillance: Infrared pattern recognition for clandestine communication
Search and rescue: Locating persons or objects under low-visibility conditions
Anti-counterfeiting: Decoding flickering infrared security codes that cannot be seen with the human eye
For colorblind people, the group even prototyped a model of the lenses that converted components of the visible red spectrum to green or blue light, possibly allowing users to differentiate colors previously invisible to them. "This could make the invisible visible," said Dr. Xue, as he points out its possibility of improving daily life for millions.
Although its potential is great, the technology has challenges to overcome before it can be sold commercially. As of now, the lenses can pick up only intense infrared signals from LED light sources. Increasing their sensitivity to ambient or low-intensity light is a key next step. Additionally, since contact lenses are near the retina, their potential to read fine details in an image is low.
To overcome this, the scientists are developing a wearable glass system using the same nanotechnology but with greater field of vision and better image quality. The aim is to develop a hybrid wearable that offers the convenience of lenses coupled with clarity and detail for complex tasks.
This revolutionary technology is a paradigm shift in the way that humans may engage with their environment. By literally broadening the visible spectrum, the innovation provides new modes for perceiving, reacting to, and comprehending our world—particularly in situations where sight has historically been impaired.
Whether wielded by surgeons, search and rescue crews, or people moving through a blacked-out terrain, the possibilities of night-vision contact lenses are staggering. As Dr. Xue summed up, "Our research opens up the potential for non-invasive wearable devices to give people super-vision."
Non-Communicable Diseases Driving More Deaths in India With Women Facing Highest Risk, Says Lancet Report

Credits: iStock
While most of the world is experiencing fewer deaths from chronic disease, India is heading in the opposite direction. The Lancet's latest analysis reveals non-communicable disease such as diabetes, cancer, and heart disease are shortening more lives—particularly among women. The statistics don't simply provide data, they tell a tale of lifestyle changes, unequal healthcare access, and who bears the largest burden.
A recent paper in The Lancet has shed new light on a disconcerting Indian trend: deaths due to non-communicable diseases (NCDs) are increasing, even as the remainder of the globe experiences improvement. These results indicate a pressing public health threat, with women shouldering the highest burden.
During 2010-2019, the majority of the globe experienced a decline in deaths due to long-term conditions like heart disease, diabetes, and some cancers. Indeed, about 80 percent of nations witnessed a fall, enhancing survival for millions. But India defied this. The research monitored 185 nations and determined that deaths from NCDs went down globally, but India saw a dramatic rise.
For men, the probability of dying from an NCD between birth and age 80 rose from 56 percent in 2001 to nearly 58 percent in 2019. For women, the picture was starker. After a modest decline between 2001 and 2010, mortality rates surged in the following decade. By 2019, the likelihood of an Indian woman dying from an NCD before turning 80 was 48.7 percent, compared to 46.7 percent in 2001.
Why Women Are at Higher Risk?
Whereas men gained advantages in the case of some disease categories like chronic obstructive pulmonary disease (COPD), heart disease, and cirrhosis of the liver, women did not experience gains in most of these categories. Apart from marginal increases in COPD, cirrhosis, and remaining NCD categories, women's mortality risks deteriorated across the board. This indicates increasing gender inequality in access to healthcare, screening, and treatment.
What Are Non-Communicable Diseases?
NCDs, also referred to as chronic diseases, are chronic conditions that unfold gradually. They consist of cardiovascular diseases (heart disease and strokes), cancers, chronic lung diseases such as COPD and asthma, diabetes, and neuropsychiatric diseases. NCDs, as reported by the World Health Organization (WHO), are responsible for 71 percent of total deaths globally. Remarkably, almost three-quarters of premature NCD deaths—deaths that occur before the age of 70—occur in low- and middle-income nations such as India.
The Alarming Case of Lung Cancer in India
A specific trend in lung cancer was emphasized by the Lancet report. Worldwide, lung cancer death decreased among men in 92 percent of nations. But India, Armenia, Iran, Egypt, and Papua New Guinea followed the opposite trend. This highlights India's peculiar susceptibility to lifestyle influences like excess tobacco use, air pollution, and late diagnosis.
Globally, lower deaths due to cardiovascular diseases and certain cancers led to most of the reduction in NCD mortality. However, this achievement was countered by increasing deaths from dementia, liver and pancreatic cancers, and alcohol use disorders. According to the study, although clinical advances such as improved diabetes and hypertension medication, cancer screening, and better emergency treatment of heart attack saved many countries, not all populations were equally exposed.
Why India Is Trailing Behind from the World?
Various structural issues seem to account for India's deteriorating performance. The report cited that the health data quality from India is "very low," which made it more difficult to monitor, prevent, and treat NCDs properly. Meanwhile, disparities in access to medicines, screenings, and preventive care continue to be widespread.
This was also fueled by the 2008 global recession. Its long shadow cut short health budgets and global health aid. Growing poverty, employment insecurity, and inadequate access to healthy foods also intensified inequalities in health. The poor, as well as vulnerable populations—usually women, the old, and poorer communities—were disproportionately hit.
Risk Factors Fueling NCDs
NCDs are highly interrelated with environmental and lifestyle determinants. They are largely driven by tobacco smoking, alcohol consumption, unhealthy diet, and physical inactivity. In India, these are added to by urbanization, air pollution, and unequal access to health care. Social determinants of health, where individuals are born, live, and work, further determine their exposure to the risk factors.
Experts say that it will take systemic transformation to turn around India's NCD burden. Majid Ezzati, lead author of the study and professor at Imperial College London, urged huge investments in healthcare infrastructure, along with tobacco and alcohol control campaigns. These interventions, already proved effective elsewhere in the world, could save millions of lives if successfully adopted in India.
The Lancet report gives a straightforward message: while large parts of the world are set to limit premature deaths from non-communicable diseases, India is in danger of being left behind. Women are especially hit with overly high risks that reflect underlying social and health inequalities.
It will take a two-pronged response—better short-term access to NCD treatments and addressing upstream determinants such as tobacco smoking, unhealthy diets, and air pollution. It also calls for improved monitoring and improved healthcare systems to ensure all groups of people enjoy the benefits.
Scientists Behind Life-Changing Cystic Fibrosis Treatment That Extends Life By Decades Win Medical ‘Nobel’ Prize
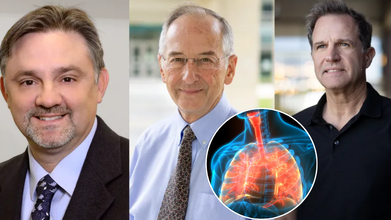
Three scientists whose groundbreaking work redefined the future of cystic fibrosis (CF) care have been awarded one of the world’s most prestigious honors in medicine: the Lasker-DeBakey Clinical Medical Research Award. Often referred to as the “American Nobel,” the award recognizes contributions that radically improve human health. This year, it went to Dr. Michael Welsh of the University of Iowa, Paul Negulescu of Vertex Pharmaceuticals, and Jesús (Tito) González, now of Integro Theranostics.
Together, their decades of research led to the creation of Trikafta, a therapy that has extended the lifespan of cystic fibrosis patients by decades and fundamentally reshaped what it means to live with the disease.
When cystic fibrosis was first described in the 1930s, it was considered a fatal childhood condition. Patients rarely survived past elementary school. Even as late as the 2010s, before Trikafta’s approval in 2019, half of patients with CF died before the age of 40.
Today, the outlook is dramatically different. Children born with CF between 2020 and 2024 who have access to Trikafta now face a median survival age of 65 years — nearly indistinguishable from the general population.
As Dr. Eric Sorscher of Emory University explained in The New England Journal of Medicine, “Available projections suggest that health and longevity may increase further as modulators begin to be administered at younger ages.”
This shift marks one of the most profound turnarounds in modern medicine.
The Role of the CFTR Gene
Cystic fibrosis is caused by mutations in a single gene: CFTR (cystic fibrosis transmembrane conductance regulator). The gene is critical for regulating the movement of ions across cell membranes, which in turn ensures proper water balance in tissues.
In healthy cells, CFTR forms channels that allow ions to flow freely. But in CF, the mutated gene produces faulty channels. The result is thick, sticky mucus that clogs the lungs and digestive system, fuels recurrent infections, and damages organs over time.
Dr. Michael Welsh, a pulmonologist and molecular biologist, helped illuminate the exact ways the most common CF mutation, delta-F508, disrupts cell function. He discovered two problems: the defective protein often gets “trapped” inside cells before reaching the surface, and even when it does reach the surface, it underperforms.
In a pivotal experiment, Welsh showed that simply lowering the temperature of cells allowed the trapped protein to move correctly. “That meant it was not totally broken,” he later recalled — a crucial realization that opened the door to correcting the defect.
Meanwhile, as a postdoctoral researcher in Nobel laureate Roger Tsien’s lab, Jesús (Tito) González developed a real-time system to track ion movement across membranes. Initially designed to study neurons, this tool proved invaluable for testing whether new drugs could restore CFTR function.
Negulescu and the Push to Find a Therapy
At Vertex Pharmaceuticals, Paul Negulescu helped drive the systematic search for compounds that could repair CFTR defects. Guided by Welsh’s molecular insights and González’s imaging system, the team screened thousands of molecules. The result was Trikafta, a triple-drug therapy that addressed the underlying cause of CF for most patients.
'Trikafta' Of Game-Changer in CF Treatment
Approved by the FDA in 2019, Trikafta combines three drugs — elexacaftor, tezacaftor, and ivacaftor — that work synergistically to help defective CFTR proteins fold correctly, reach the cell surface, and function effectively. The impact has been extraordinary. Since its introduction:
- Hospitalizations for lung infections have plummeted.
- The need for lung transplants has declined.
- Patients report stronger lung function, weight gain, and dramatically improved quality of life.
- For many families, the treatment has meant that milestones once unimaginable — graduating college, starting families, living into retirement — are now within reach.
Recognition at the “American Nobels”
The Lasker Awards, founded in 1945, celebrate biomedical achievements that shape the future of health. They are considered one of the highest honors in science, often predicting future Nobel Prizes.
The recognition of Welsh, González, and Negulescu underscores the profound impact of their work. The $250,000 prize, while symbolic compared to the billions Trikafta has generated, highlights the ethical and humanitarian dimension of their achievement: turning a once uniformly fatal disease into a chronic, manageable condition.
What CF Treatment Means for Medicine?
The CF breakthrough is not just about one disease. It represents a paradigm shift in genetic medicine. By targeting the root molecular defect rather than simply managing symptoms, Trikafta has become a model for other genetic conditions, from sickle cell disease to rare metabolic disorders.
It also illustrates the power of partnerships between academic researchers, biotech innovators, and patient foundations. The Cystic Fibrosis Foundation’s early investments in research were critical to advancing the work that ultimately led to Trikafta’s approval.
While Trikafta has transformed care in wealthy countries, challenges remain. The therapy is expensive — with an annual price tag of over $300,000 in the U.S. — putting it out of reach for many patients globally.
Furthermore, a subset of CF patients with rare genetic mutations still do not benefit from the drug, leaving an urgent need for alternative therapies. And as with all long-term treatments, researchers must continue monitoring for side effects and resistance.
Roughly 100,000 people worldwide live with cystic fibrosis. For decades, their lives were defined by daily medical regimens, frequent hospitalizations, and shortened lifespans. Today, thanks to the pioneering work of Welsh, González, and Negulescu, those same patients are looking toward futures filled with possibility.
FDA Approves Inlexzo For Bladder Cancer: Could This End Organ Removal Surgery?

Credits: iStock
The US Food and Drug Administration (FDA) has granted approval to Inlexzo (gemcitabine intravesical system) for the treatment of certain types of bladder cancer. This decision marks a milestone for patients with Bacillus Calmette-Guérin (BCG)-unresponsive, non-muscle-invasive bladder cancer (NMIBC), particularly those living with carcinoma in situ (CIS), with or without papillary tumors.
Unlike systemic therapies, Inlexzo works through a novel drug-releasing intravesical system designed for extended local delivery of gemcitabine into the bladder. For patients who wish to preserve their bladder and avoid radical surgery, the approval opens a long-awaited alternative.
Bladder cancer is the sixth most common cancer in the United States, disproportionately affecting older adults. Patients with NMIBC often start with BCG immunotherapy, the gold standard treatment. While many respond well initially, a significant proportion develop resistance or fail to sustain remission.
For these patients, the only widely recommended option has been radical cystectomy—a surgery to remove the bladder. Though effective, the procedure carries high risks, including a 3–8 percent post-surgical mortality rate, long recovery periods, and significant impact on quality of life. Many older patients are either unfit or unwilling to undergo the operation.
What this really means is that patients who have exhausted BCG therapy have been left with limited, often life-altering choices. Inlexzo offers a chance to delay or avoid bladder removal while still pursuing effective treatment.
The FDA’s approval was based on results from the SunRISe-1 phase 2b trial, a single-arm, open-label study. Findings showed:
- 82 percent of patients achieved a complete response following treatment.
- 51 percent of those maintained their response for at least a year.
Dr. Sia Daneshmand, principal investigator of SunRISe-1 and a urologic oncologist at the University of Southern California, emphasized the significance of these results, “I see many patients that ultimately become BCG-unresponsive and often face life-altering bladder removal. In my experience, Inlexzo is well tolerated and delivers clinically meaningful results. This will change the way we treat appropriate patients that haven’t responded to traditional therapy.”
Such durability of response signals a meaningful step forward in NMIBC care, particularly for patients for whom cystectomy is not feasible.
What Is Non-Muscle-Invasive Bladder Cancer (NMIBC)?
NMIBC represents a subset of bladder cancers confined to the inner lining of the bladder wall. It is categorized as low, intermediate, or high risk, depending on tumor size, multiplicity, and the presence of CIS. Approximately 10 percent of NMIBC patients are diagnosed with CIS, a flat but aggressive form of cancer that requires close management.
The reliance on BCG has long been the standard of care, but when patients become unresponsive, treatment options have been scarce. Radical cystectomy has remained the fallback. The approval of Inlexzo helps close a treatment gap that has persisted for decades.
How Inlexzo Works?
Inlexzo is not a traditional infusion or oral drug. It uses a drug-eluting intravesical system, placed inside the bladder during a short, office-based procedure. It does not require general anesthesia and begins releasing gemcitabine immediately, maintaining extended exposure directly to the bladder tissue. This approach is significant for two reasons:
- It keeps the chemotherapy localized, limiting systemic exposure.
- It allows for continuous therapeutic action without repeated, invasive interventions.
- For many patients, this translates into a treatment that is not only effective but also easier to tolerate and less disruptive to daily life.
Risks, Safety, and Limitations
While Inlexzo is a major advancement, it is not without risks. The FDA has issued clear precautions:
- Patients with bladder perforations or compromised bladder lining should not receive Inlexzo, as systemic exposure to gemcitabine may cause severe reactions.
- Delaying cystectomy in patients with persistent CIS could increase the risk of progression to muscle-invasive or metastatic bladder cancer, which is often lethal.
- MRI safety is limited to specific conditions, requiring close adherence to guidelines.
Reproductive risks include embryo-fetal toxicity and potential male infertility, based on animal studies. Women are advised to avoid pregnancy during treatment and for at least a week after device removal.
The most common side effects include urinary frequency, infections, bladder irritation, and blood in the urine. Serious adverse events occurred in 24 percent of patients, with 1.2 percent experiencing fatal outcomes, though these were rare.
Is This System A Patient-Centered Shift in Bladder Cancer Care?
Bladder cancer disproportionately impacts older adults—72 percent of patients in the SunRISe-1 study were over 65 years old. For this group, surgery carries heightened risks. Inlexzo’s approval gives clinicians a new tool to help manage NMIBC without immediately resorting to bladder removal.
As Dr. Daneshmand noted, this drug-delivery innovation may change the treatment landscape by filling a crucial gap in care. For patients who have exhausted BCG and face limited choices, Inlexzo offers hope for improved survival and quality of life.
Inlexzo’s approval is a win not only for patients but also for the field of urologic oncology. The drug’s placement under Johnson & Johnson’s portfolio signals strong industry investment in localized, bladder-preserving therapies.
Experts caution, however, that long-term follow-up studies will be essential to fully understand Inlexzo’s durability, risks, and potential role in combination with other therapies. For now, the FDA’s decision gives patients an urgently needed option that bridges the gap between immunotherapy failure and radical surgery.
© 2024 Bennett, Coleman & Company Limited

