- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
This New Blood Test Could Spot Leukemia Risk Without The Painful Bone Marrow Sampling
Credits: Health and me
Just days after their laboratories were devastated by an Iranian missile attack, Profs. Liran Shlush and Amos Tanay of the Weizmann Institute of Science have published a landmark study that could transform how we detect and predict leukemia and other blood disorders. Their research, released in Nature Medicine, introduces a revolutionary blood test that may one day replace the painful, invasive bone marrow biopsy—a procedure dreaded by patients and clinicians alike.
Developed by Professors Liran Shlush and Amos Tanay, this innovation replaces the traditionally painful and invasive bone marrow biopsy with a cutting-edge, non-invasive blood test.
This development is poised to revolutionize diagnostics in hematology and could dramatically reduce global dependence on bone marrow sampling — a procedure that over a million people endure each year globally.
Why Bone Marrow Biopsies Have Been the Gold Standard?
For decades, diagnosing blood cancers such as leukemia has relied on extracting bone marrow—a process that involves drilling into the bone, typically under local anesthesia or sedation. The procedure is not only uncomfortable and anxiety-inducing but also costly, technically demanding, and sometimes inconclusive. Even when a sample is obtained, pathologists may disagree on whether the cells are healthy or diseased, leaving patients and their families in limbo.
The study found a way to detect and analyze rare blood-forming stem cells that occasionally escape the bone marrow and enter the bloodstream. These elusive cells, though few — often just one in a million — carry a wealth of diagnostic information.
“As we age, our blood stem cells accumulate mutations,” explains Prof. Shlush. “These mutated cells eventually dominate the blood system, failing to produce healthy blood cells and laying the groundwork for conditions like myelodysplastic syndrome (MDS) and leukemia.”
Traditionally, these defective cells are hidden within the bone marrow, undetectable by standard blood tests. Bone marrow biopsies, while effective, are painful, costly, and often inconclusive. But this new method captures and analyzes the rare migratory stem cells through a simple blood draw, combined with advanced single-cell genetic sequencing.
How a Simple Blood Test Changes Cancer Diagnosis?
The breakthrough came when Dr. Nili Furer, Nimrod Rappoport, and Oren Milman, collaborating with researchers in Israel and the U.S., discovered that rare blood stem cells occasionally escape the bone marrow and circulate in the bloodstream. These migrating cells, though extremely scarce—sometimes just a handful in a milliliter of blood—carry crucial diagnostic information.
By applying advanced single-cell genetic sequencing, the researchers were able to isolate and analyze these rare cells, identifying early signs of MDS and assessing an individual’s risk of developing blood cancer. This approach allows for the detection of disease processes long before symptoms arise, offering a window of opportunity for early intervention.
Focus on Myelodysplastic Syndrome
The study centers on myelodysplastic syndrome (MDS) — an age-related condition where stem cells fail to mature properly, leading to ineffective blood production and a heightened risk of progressing to acute myeloid leukemia (AML), a particularly aggressive form of cancer.
Previously, diagnosing MDS required extracting marrow with a needle — an uncomfortable procedure that many patients dreaded. Now, thanks to this innovation, the same diagnosis can be made using peripheral blood samples. Dr. Nili Furer, along with collaborators Nimrod Rappoport and Oren Milman, played a critical role in demonstrating that these rare stem cells in blood are sufficient for detecting MDS and its progression risk.
Why Men Age Faster — At Least in Their Blood?
One of the study’s more striking revelations involves gender differences in blood aging. The researchers observed that stem cell aging occurs faster in men than in women, which may explain why blood cancers are more prevalent in males.
“Men’s stem cells begin to exhibit cancer-prone mutations earlier than women’s,” notes Prof. Shlush. “This gender-based variance in blood aging is an eye-opener and may inform future prevention strategies.”
The test not only identifies disease but also acts as a biological clock, providing new insights into how blood ages — revealing patterns that even bone marrow biopsies have failed to detect.
Capturing and characterizing these rare cells required a blend of cutting-edge laboratory techniques and sophisticated data analysis. Each cell yielded tens of thousands of data points, and the team analyzed millions of cells from participants ranging in age from young adults to 95-year-olds. Prof. Tanay’s expertise in computational biology was instrumental in making sense of this vast dataset, enabling the team to distinguish healthy cells from those showing early signs of disease.
Implications of The New Blood Test On Treatment
The implications of this discovery are profound. Clinical trials based on the new blood test are already underway at multiple medical centers worldwide. The researchers believe that, in time, this test could be used not only for MDS and leukemia but also for a broad spectrum of blood-related disorders. By providing a non-invasive, highly sensitive diagnostic tool, the test has the potential to spare millions of patients from the ordeal of bone marrow biopsies each year.
“As part of the aging process, stem cells—the ones capable of generating all blood cells—undergo genetic changes and mutations,” explains Prof. Shlush. “With time, these cells accumulate mutations and begin to dominate the blood system. They stop differentiating properly, produce only themselves, and suppress the production of healthy cells. Eventually, this can lead to deadly diseases like blood cancers.”
The research itself is as resilient as its scientists. Just days before the study’s release, the labs of Profs. Shlush and Tanay at the Weizmann Institute were severely damaged in an Iranian missile attack. Despite the destruction, the team pushed forward, ensuring the findings reached the scientific community on time.
The study reflects the combined efforts of a global team of physicians, biologists, and data scientists across Israel and the United States, proving that science endures even in the face of adversity.
The prospect of replacing an invasive, expensive, and often ambiguous diagnostic procedure with a quick, precise, and painless blood test is a major leap forward. For millions worldwide, this means earlier detection, better prognosis, and more effective treatment strategies — all from a single vial of blood.
Michael Clarke Reveals Skin Cancer Surgery, Sparking Urgent Reminder: How To Spot The Signs Early?

Credits: Instagram/Michael Clarke
Former Australian cricket captain Michael Clarke has once again faced a health struggle that affects millions around the globe, skin cancer. Clarke, 44, posted on social media that he recently had surgery to have a suspicious growth removed from his nose. His post was not just about healing, but also an appeal: get your skin checked.
This reminder from a sports legend underscores a pressing global health issue. Skin cancer is the most common cancer diagnosed in the United States, Australia, and many other parts of the world. The good news is that when detected early, most cases are highly treatable but that early detection depends on awareness knowing what skin cancer looks like and when to seek medical help.
Clarke's recent diagnosis is not his initial experience with skin cancer. In 2006, doctors operated on him to remove suspicious marks on his face and chest. They removed them surgically before they were able to do further damage. Again in 2019, he had surgery to have cancerous tumors removed from his forehead.
Now, in 2025, his post-surgery update again emphasizes how skin cancer can be a recurring aspect for those at risk. Clarke had penned, "Skin cancer is real! Particularly in Australia. Another one removed from my nose today. A friendly reminder to have your skin checked. Prevention is better than the cure but in my case, regular check-ups and early detection is the key."

Australia has some of the highest rates of skin cancer on the planet because of high levels of UV radiation. However, Clarke's experience sounds off far beyond his native soil. In the United States alone, more than 5 million instances of skin cancer are treated annually, the American Cancer Society says.

What Is Skin Cancer?
Skin cancer occurs when skin cells grow out of control, penetrating surrounding tissue and occasionally spreading to other organs. The sun's ultraviolet (UV) light is the primary cause, though indoor tanning is also a culprit. There are three types of skin cancer with varying risks and appearances:
Basal Cell Carcinoma (BCC): The most frequent one. BCC typically appears as a flesh-colored bump, pearl-like growth, or pinkish lesion. It usually develops on sun-exposed sites such as the face, neck, and arms. Although it does not spread much, if left untreated, it can produce extensive local destruction.

Squamous Cell Carcinoma (SCC): The second most frequent type. SCC can be a hard red bump, scaly area, or sore that closes up and reopens. It often occurs on sun-exposed areas like the ears, lips, and face. If left alone, SCC can grow and invade deeper tissues.

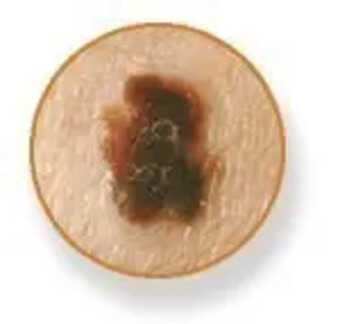
Melanoma: The most life-threatening form. Melanoma can develop in a pre-existing mole or as a new dark spot that appears different from surrounding markings. It grows more quickly than other skin cancers, so catching it early is paramount.
SCC can develop from a precancerous skin growth: Actinic keratoses are primarily caused by cumulative sun exposure and tend to develop on areas of the body that get the most sunlight, including the face, scalp, neck, hands, and forearms. People with fair skin are more likely to develop these patches, but they can occur in anyone with a history of significant sun exposure.

What Does Skin Cancer Look Like?
One of the difficulties with skin cancer is that its early signs are simple to overlook or assume to be harmless. However, being in a position to recognize these alterations can be the difference between life and death. General warning signals are:
- A new growth that looks like a mole, bump, or scab.
- An open sore that does not heal.
- A patch of skin that is rough or scaly.
- Alterations in a mole getting larger, darker, or becoming irregular in shape.
- Persistent itching or pain around a skin spot.
Doctors recommend following the ABCDE rule for melanoma:
Asymmetry: One half doesn’t match the other.
Border: Edges are irregular or blurred.
Color: Uneven colors—brown, black, red, or white patches.
Diameter: Larger than 6mm (about the size of a pencil eraser).
Evolving: Any mole or spot that changes in shape, size, or symptoms.
Where Skin Cancer Can Appear?
Most individuals think that skin cancer only occurs on sun-exposed skin. Although it is correct that the scalp, face, neck, arms, and hands are the most susceptible, cancers can occur on less visible locations:
- Under the toenail or fingernail.
- On the palms or soles of the feet.
- Around the genitals.
- On the back, which individuals might seldom examine themselves.
This is particularly the case for individuals with darker skin. In these individuals, melanoma and other types tend to appear on less sun-exposed areas, i.e., under nails or on the feet.
Who Is at Greatest Risk?
Anyone may get skin cancer, but certain individuals have a higher risk based on specific characteristics. People with fair skin, light hair, and light eyes are at greater risk, as are those with past histories of severe sunburns, particularly blistering. Frequent sun exposure with poor protection and tanning bed use also increase the risk of skin cancer. An inheritance pattern of the illness or compromised immune system further increases the risk. Michael Clarke's years of cricket playing in the strong Australian sunlight emphasize how long-term exposure to the sun can dramatically raise the risk of skin cancer.
Is Skin Cancer Preventable?
While you cannot alter your genes or your skin type, you can lower your risk considerably:
- Use sunscreen daily with SPF 30 or better. Apply every two hours when you're outside.
- Wear protective gear, wide-brimmed hats, sunglasses, and long sleeves.
- Seek shade between 10 a.m. and 4 p.m. when the sun's rays are strongest.
- Steer clear of tanning beds, which release cancer-causing UV radiation.
- Have your skin checked regularly, both at home and by a dermatologist.
Clarke's focus on early diagnosis is echoed in medical guidance: the sooner you detect changes, the greater the potential for effective treatment.
Why Regular Checkups Are So Important?
Skin cancer often develops silently. A small bump today may not cause pain but could evolve into something dangerous over time. Clarke’s case illustrates why vigilance is critical even after previous treatments. Recurrence is possible, and only regular screenings can catch issues before they progress.
The American Academy of Dermatology recommends annual full-body skin checks for most adults, and more frequent exams for those with higher risk factors.
Michael Clarke's candor regarding his diagnosis puts a spotlight on a public health problem that affects the entire world. His tale is not merely that of an athlete undergoing another surgery it is a reminder to all, wherever they may be in the world, that skin cancer exists, is prevalent, and is frequently preventable.
Legionnaires’ Outbreak Canada: 94 Sick So Far, Ontario Food Manufacturer's Cooling Tower Could Be Source Of The Deadly Disease

Credits: Canva
Legionnaires Outbreak: Public health officials in London, Ontario, have redeclared a Legionnaires’ disease outbreak after 25 new cases emerged, weeks after declaring the situation under control. The Middlesex-London Health Unit (MLHU) confirmed Tuesday that testing has identified a likely source: cooling towers at Sofina Foods Inc., a large meat-processing facility on Trafalgar Street.
Outbreak Declared Over, Then Returned
The outbreak was first detected in early July and by early August had led to 70 confirmed cases and three deaths. After three weeks without new infections, the MLHU declared the outbreak over on August 6. But within days, new patients began appearing.
As of this week, the caseload has climbed to 94, including 86 hospitalizations and four deaths. Six patients remain in hospital. Officials say the resurgence highlights how the bacteria can persist in contaminated environments despite earlier cleaning efforts.
“For several weeks, no additional illnesses were reported, and we were optimistic that remediation efforts had eliminated the bacteria. However, 25 more people have now become ill,” said Dr. Joanne Kearon, associate medical officer of health. “Fortunately, a likely source has now been identified.”
Read: Legionnaires Outbreak in New York: All That You Need To Know About The Disease
Cooling Towers Traced as the Source
Extensive environmental testing linked the outbreak strain of Legionella bacteria to Sofina Foods’ cooling towers. Samples taken in recent weeks matched the same bacterial subtype found in patient cases.
While nine different cooling towers across the city initially tested positive for live bacteria, the Sofina plant produced a definitive genetic match. Earlier testing at the site in 2024 and early 2025 had shown no match, but officials said the bacteria can survive in cooling towers and regrow under hot, humid conditions.
The health unit emphasized that food products from Sofina remain safe to consume, since Legionnaires’ disease spreads only through inhaling contaminated water droplets, not through eating or drinking.
Sofina Foods Responds
Sofina Foods, which employs hundreds of workers in London’s east end, said the new findings were “unexpected” given the company’s daily sanitation protocols and previous negative test results.
“We are deeply concerned with this new information and are continuing to investigate fully,” said Sharon Begley, Sofina’s chief safety officer. “Over and above our regular processes, we conducted further deep cleaning and disinfecting processes recommended by MLHU. The cooling tower is offline and will remain offline until these additional steps are completed.”
The company stressed its commitment to employee and community safety, noting it has been cooperating closely with public health authorities since the outbreak began.
How Legionnaires’ Spreads
Legionnaires’ disease is a severe form of pneumonia caused by Legionella bacteria. It is not transmitted from person to person. Instead, people get sick when they inhale mist or small droplets of water containing the bacteria, which can be carried by wind from sources such as cooling towers, hot tubs, and water systems.
Symptoms typically appear within 2 to 10 days of exposure and may include fever, chills, cough, muscle aches, and shortness of breath. Most exposed individuals do not get sick, but older adults, smokers, and people with weakened immune systems face greater risk of serious illness.
The current outbreak has been concentrated in a six-kilometre radius in London, with cases ranging from young adults to seniors. No children have been affected to date.
Also Read: Legionnaires' Outbreak Update: It Is No Longer 'Only A New York Problem'
More Cases Possible
Dr. Kearon warned that more cases could surface due to the bacteria’s incubation period. “Legionella has an incubation period of two to 10 days ... there may still be further cases in the next two weeks,” she said.
This year’s outbreak is already the largest in London’s recent history, surpassing a 2024 outbreak that caused 30 cases and two deaths. Officials say they are working with Sofina Foods and other operators to ensure thorough remediation and prevent further spread.
“The decision to reopen the outbreak reflects a rise in cases after several weeks without new cases, suggesting that the Legionella bacteria has re-emerged in the environment despite earlier remediation efforts,” MLHU said in a statement.
Eli Lilly Sends Weight-Loss Pill For Approval: Is Oral GLP-1 As Effective As The Injections?

Credits: Canva
Eli Lilly has taken a major step in the fight against obesity and diabetes. The company announced that its oral GLP-1 drug, orforglipron, successfully met the “primary and all key secondary endpoints” in a large clinical trial, paving the way for global regulatory submissions.
“With these positive data in hand, we are moving with urgency toward global regulatory submissions to potentially meet the needs of patients who are waiting,” said Kenneth Custer, Eli Lilly’s executive vice president and president of cardiometabolic health.
“If approved, we are ready to offer a convenient, once-daily pill that can be scaled globally, removing barriers and redefining how obesity is treated around the world.”
What Is Orforglipron?
Orforglipron is an investigational, non-peptide, once-daily small molecule GLP-1 receptor agonist. Unlike some oral medications that come with strict food or water restrictions, it can be taken at any time of day without such limitations.
Originally discovered by Japan’s Chugai Pharmaceutical and later licensed to Eli Lilly in 2018, orforglipron is now in Phase 3 trials. The company is testing it not just for weight management and type 2 diabetes but also for conditions linked to obesity, including obstructive sleep apnea and hypertension.
The ATTAIN-2 Trial Results
The company’s latest clinical trial, called ATTAIN-2, produced results that have drawn significant attention. At the highest dose: 36 mg daily for 72 weeks, participants saw an average weight loss of 22.9 pounds (10.5%), compared to just 5.1 pounds (2.2%) among those given a placebo.
The drug also delivered strong results for people with type 2 diabetes. Across doses, orforglipron reduced A1C levels by 1.3% to 1.8% from a baseline of 8.1%. Notably, 75% of participants who took the highest dose achieved an A1C of 6.5% or below, aligning with the American Diabetes Association’s definition of diabetes remission.
Beyond weight and blood sugar, orforglipron showed broader health benefits. The trial reported improvements in cardiovascular risk factors such as non-HDL cholesterol, systolic blood pressure, and triglyceride levels. In an exploratory analysis, the drug also cut high-sensitivity C-reactive protein, a key marker of inflammation, by about 50%.
Why An Oral Option Matters
Injectable GLP-1 receptor agonists like semaglutide and tirzepatide have already transformed obesity and diabetes care, but accessibility remains a hurdle. For many patients, injections are intimidating, inconvenient, or simply not practical in daily life.
That’s where an oral pill could be a game-changer. A once-daily tablet could remove psychological and logistical barriers, making it easier for patients to stay on treatment. And given the rising global burden of obesity, which significantly raises the risk of cardiovascular disease, stroke, and some cancers, the demand for more convenient treatment options has never been greater.
Pills vs. Injections: Which Works Better?
The big question now is whether oral GLP-1 drugs are as effective as their injectable counterparts.
A 2021 research review published in Springer Nature, offers some clues. After examining multiple studies, researchers concluded that oral semaglutide, a similar class of drug, provided “similar or better efficacy and similar tolerability” compared to injectable GLP-1 receptor agonists.
Also Read: How To Identify A Counterfeit Ozempic? Look For These Signs
In some cases, oral versions were found to be just as effective for weight loss and lowering A1C levels in people with type 2 diabetes. However, the review focused on patients already using insulin, which may have influenced outcomes. Experts emphasize that while results are encouraging, more research is still needed to directly compare oral and injectable versions in broader populations.
For now, injections remain the gold standard in clinical practice. Drugs like Wegovy and Mounjaro (both injectables) have shown weight reductions of 15% to 20% or more in major trials, higher than the 10.5% seen with orforglipron in ATTAIN-2. That said, the convenience of a pill could tip the balance for many patients, especially those reluctant to use injections long-term.
Eli Lilly’s oral GLP-1 drug is not yet approved, but the latest results highlight its potential to reshape treatment strategies for obesity.
© 2024 Bennett, Coleman & Company Limited

