- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
WHO Warns Of Rising Mpox Cases As New ‘Clade Ib’ Strain Spreads Globally—See The List Of Affected Countries
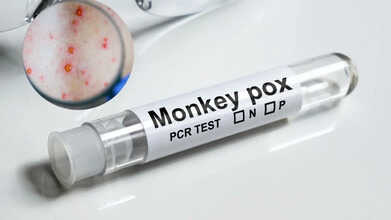
Credits: CANVA
The World Health Organization (WHO) has raised concern over the continued spread of Mpox (formerly known as monkeypox) across Africa and other regions. In the past six weeks alone, 17 African nations have reported active transmission. Between September 14 and October 19, there were 2,862 confirmed infections and 17 related deaths, according to WHO’s 59th multi-country situation report released on October 30.
The Democratic Republic of Congo, Liberia, Kenya, and Ghana have reported the highest number of cases. Infections have increased notably in Kenya and Liberia, while the Democratic Republic of Congo has seen a slight decline and Ghana is beginning to show early signs of improvement.
What Is Mpox and How Does It Spread?
Mpox, previously known as monkeypox, is a viral infection caused by the monkeypox virus, which belongs to the Orthopoxvirus genus. The World Health Organization (WHO) identifies two main clades of the virus, Clade I (subdivided into Ia and Ib) and Clade II (IIa and IIb). The widespread outbreak seen during 2022–2023 was primarily linked to Clade IIb.
Typical symptoms include skin rashes or lesions that last two to four weeks, along with fever, body aches, swollen lymph nodes, fatigue, and headaches.
The infection spreads through close physical contact with an infected person, contaminated objects, or animals carrying the virus. Transmission from a pregnant woman to her baby can also occur.
How Serious Is the Global Mpox Situation Now?
According to the World Health Organization (WHO), a total of 42 countries reported 3,135 confirmed Mpox infections and 12 related deaths in September, with more than four-fifths of all cases recorded in Africa. While most regions have seen infection rates ease, the European and South-East Asian regions are now showing a slight increase.
The WHO stated that all variants, or clades, of the monkeypox virus (MPXV) remain in circulation worldwide. Experts caution that if emerging outbreaks are not swiftly controlled, ongoing community transmission may occur.
It is worth noting that in the same month, the WHO ended Mpox’s designation as a Public Health Emergency of International Concern (PHEIC) after observing a consistent decline in new infections, particularly in heavily affected African countries.
Where Has the New Clade Ib Variant Been Found?
The Clade Ib form of the Mpox virus has been newly detected in Malaysia, Namibia, the Netherlands, Portugal, and Spain. Additional imported cases linked to international travellers carrying the same strain have appeared in Belgium, Canada, Germany, Italy, Qatar, and Spain.
Evidence of local transmission—cases without any recent travel exposure, has been confirmed in six countries outside Africa: Italy, Malaysia, the Netherlands, Portugal, Spain, and the United States. In the U.S., three patients hospitalised in California tested positive for the new variant despite no travel history, according to The Guardian, prompting concern among health authorities.
Following these developments, WHO has officially classified these countries as experiencing community-level spread of the Clade Ib MPXV strain.
How Are Countries Responding to the Renewed Spread of Mpox?
WHO continues to assess the global Mpox threat as moderate among men who have sex with men (MSM) and low for the general population. The agency is encouraging governments to sustain surveillance systems, improve testing capabilities, and maintain access to vaccines and treatment options to prevent wider community outbreaks.
Flu Cases In US Reach 5 Million Mark, Reveals CDC Data

Credits: iStock
Flu cases in the US has touched almost the 5 million mark, as per the latest data from the Centers for Disease Control and Prevention (CDC). New York City has seen the highest levels of flu-like activity, revealed the data. Among the other states are Alabama, Colorado, Connecticut, Hawaii, Louisiana, Maryland, Minnesota, New Hampshire, New Jersey, Ohio, Rhode Island, and Texas. All these states noted a "moderate" level of flu-like or respiratory illnesses, while rest of the states remain in "low" or "very low" levels of flu-like activities.
What Does The CDC Data Reveal In Flu Cases?
As per the CDC data, there have been at least 4.6 million illnesses, with 49,000 hospitalization, and 1,900 deaths so far by flu in this season. These cases of flu are linked with the new variant known as the subclade K. CDC notes that among the samples sent to it, of the over 900 of them, 0-% were A(H3N2), of those that had further testing, nearly 90% of them were subclade K.
The CDC also notes that this mutant is a mismatch from the season's flu vaccine composition, however, according to experts the vaccine is still useful as the first line of defense against flu, including to avoid any severe illness, hospitalization, and or death.
John Brownstein, an epidemiologist told the ABC News, "Even with this new variant and some mismatch with the vaccine, getting a flu shot is still absolutely worth it. The vaccine continues to provide strong protection against severe outcomes like hospitalization and death, and that’s especially important as flu activity ramps up."
Flu Deaths In Children
Two pediatric flu deaths were reported this week, which brought the total number three to this season. Last season, there were 288, the same as the number in 2009 during the H1N1 pandemic, It is the highest levels since 2004. It was in that year when flu child deaths became mandatory for states to report to CDC.
The CDC found that about 90% of children who died from flu last season were not vaccination. The CDC study found that flu vaccination among kids have dropped 10% points lower than the pre-pandemic levels, with about only 40% of children getting the flu shot this season.
As of now, around 140 million doses of flu have been distributed, whereas last year, it was 128 million. The CDC also notes that anyone over the age of 6 months must get their annual flu shot. It is never too late to get the vaccine, note the experts.
Brownstein also notes: "This is the time of year when flu typically starts to take off, and we expect activity to continue increasing in the weeks ahead. As people gather indoors and travel more around the holidays, those conditions can accelerate spread."
H3N2 Symptoms
- High fever (often above 101°F)
- Severe body aches and muscle pain
- Extreme tiredness that lasts longer
- Dry cough that can be persistent
- Headache
- Sore throat
- Runny or stuffy nose
- Loss of appetite
- Nausea (especially in children)
The recovery time of any influenza could last up to 5 to 14 days, the key is to monitor breathing patterns and avoid over medication.
Could Donald Trump Have Tertiary Stage Syphilis? Here’s Why This Doctor Believes It’s Possible

Credits: AP
Donald Trump’s health has long been under scrutiny, and a recent Instagram post by a physical therapist, @epistemiccrisis, who holds a doctorate and has 14 years of experience treating dementia patients, has stirred fresh speculation. The doctor discussed how tertiary stage syphilis, also known as neurosyphilis, can closely mimic the symptoms of behavioural variant frontotemporal dementia.
What Is Tertiary Stage Syphilis?
Tertiary syphilis is the late stage of a syphilis infection, and it is relatively uncommon, usually appearing years or even decades after the initial infection. Its manifestations can vary, but the most common forms include cardiovascular syphilis, central nervous system involvement—classically presenting as tabes dorsalis or general paresis—and gummatous syphilis, which most often affects the liver. In the United States, syphilis is considered a reportable illness, meaning cases must be reported to public health authorities.
Tertiary Stage Syphilis And The Brain
Tertiary stage syphilis occurs when the infection remains untreated for years, potentially causing serious neurological complications. Before antibiotics were widely available, neurosyphilis accounted for roughly 15% of psychiatric inpatients, as per the doctor. The disease can damage the frontal and temporal lobes, producing behavioural changes strikingly similar to dementia.
Case Study Explains The Symptom Overlap
The doctor referenced a PubMed case study of a 47-year-old male whose behaviour drastically changed, leading to psychiatric admission. The patient showed extreme disorientation and poor hygiene, including rubbing his own faeces in his hair. After receiving antibiotics, his symptoms resolved, and brain scans later revealed improved blood flow to the frontal lobe.
Could Donald Trump Have Tertiary Stage Syphilis?
Red marks on Trump’s hands have sparked discussion about possible tertiary stage syphilis. However, the doctor noted that untreated syphilis in someone of Trump’s age would generally produce more severe complications, making the likelihood low. Additional health factors, including possible history of stroke, heart issues, and kidney disease, further complicate speculation.
Are Frontotemporal Dementia and Tertiary Syphilis Related?
Donald Trump has been speculated to show signs of frontotemporal dementia, a condition affecting behavior, personality, and decision-making. Interestingly, tertiary stage syphilis, specifically neurosyphilis, can cause similar symptoms by damaging the frontal and temporal lobes. Both conditions may lead to changes in social behavior, judgment, and cognitive function, making it challenging to differentiate without proper medical evaluation. Unlike frontotemporal dementia, which is progressive and currently incurable, tertiary syphilis is treatable with antibiotics, underscoring the need for accurate diagnosis.
Is Tertiary Stage Syphilis Treatable?
Neurosyphilis is treatable with antibiotics, and early detection is critical. The case study highlights how the condition can mimic dementia, emphasizing the need for careful evaluation—even for high-profile figures like Donald Trump.
Disclaimer: The claims discussed in this article are being made by the Instagram user @epistemiccrisis. Health & Me does not verify or endorse these claims, and this content is intended for informational purposes only, not as a medical diagnosis or advice.
Ayush Mark Explained: What Is This New Global Standard Label For Traditional Medicine?

Credits: Canva
Prime Minister Narendra Modi unveiled the Ayush Mark at the Second WHO Global Summit on Traditional Medicine on Friday. The Ayush Mark is envisioned as a global standard for quality Ayush products and services. The WHO Global Summit on Traditional Medicine was held at Bharat Mandapam from December 17 to December 19, 2025, with this year’s theme, “Restoring balance: The science and practice of health and well-being.” Speaking at the closing ceremony, PM Modi highlighted India’s rising leadership in promoting traditional medicine as an evidence-based, integrated, and people-focused part of global health systems.
Alongside the Ayush Mark, PM Modi also introduced the My Ayush Integrated Services Portal (MAISP), the central digital platform of the Ayush Grid, released a commemorative Ashwagandha postal stamp, the WHO technical report on Yoga training, and the book “From Roots to Global Reach: 11 Years of Transformation in Ayush.” He also presented the Prime Minister’s Awards for Outstanding Contribution to the Promotion and Development of Yoga, recognizing both national and international individuals and organizations for their exceptional service.
Speaking at the event, he said, “Over the past three days, experts from across the world in traditional medicine have held meaningful discussions here. I am glad India is providing a strong platform for this, and the WHO has actively participated. It is our good fortune and a matter of pride that the WHO Global Centre for Traditional Medicine has been established in Jamnagar, India. The world entrusted us with this responsibility with great confidence at the first Traditional Medicine Summit.”
What Is The Ayush Mark?
The Ayush Mark is a label issued by the Ministry of Ayush for Ayurveda, Yoga and Naturopathy, Siddha, Unani, and Homoeopathy products and services. The Ayush Mark Certification Scheme has been run by the Quality Council of India (QCI) since 2009.
Products and services carrying the Ayush Mark follow quality manufacturing practices, use standard raw materials, and undergo safety testing. The Ayush Mark and its two previous certification levels have existed for several years. The new label builds on them and aims to set a global benchmark for traditional medicine products and services. Earlier certifications included the Ayush Standard Mark and the Ayush Premium Mark.
The Ayush Standard Mark follows Good Manufacturing Practices (GMP) for Ayurvedic, Siddha, and Unani medicines under Schedule T of the Drugs and Cosmetic Rules, 1945. The Ayush Premium Mark is aligned with WHO GMP guidelines for herbal medicines.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, also attended the WHO Global Summit on Traditional Medicine. He praised PM Modi for elevating traditional medicine to a global platform. Dr Tedros commended India for turning vision into action, calling the country a global leader in transforming traditional medicine from heritage to evidence-informed practice. He highlighted landmark initiatives like the establishment of the Ministry of Ayush and the WHO Global Centre for Traditional Medicine in Jamnagar, noting these efforts have strengthened the integration of traditional medicine into health systems, research, and policy, supporting universal health coverage and sustainable development worldwide.
Global Recognition and Impact of Ayush Mark
The Ayush Mark is not just a certification but a step toward placing Indian traditional medicine on the world stage. By setting internationally recognized quality benchmarks, it aims to boost confidence among global consumers and practitioners, encouraging the adoption of Ayurveda, Yoga, Naturopathy, Siddha, Unani, and Homoeopathy products and services worldwide. This initiative reinforces India’s role in shaping evidence-based, safe, and sustainable traditional medicine practices across borders.
© 2024 Bennett, Coleman & Company Limited

