- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Are You Able To Thrive On Just 4 Hours Of Sleep? This Rare Gene Mutation Might Be Why

Credits: Canva
I’ve never needed much sleep to feel refreshed. While most of my friends groan without their full 8 hours and reach for coffee before conversations, I’ve always felt perfectly fine—sometimes even better—after just four or five hours of shut-eye.
For years, I had thought that I was merely the "odd one out," a person with an offbeat sleeping pattern always harming my body maybe but now it appears, there could be a genetic explanation for why individuals like myself are programmed this way. Scientists found a rare gene mutation in a gene known as SIK3 that enables some of us to function just fine on less sleep. No drowsiness. No foggy brain. No side effects.
If you’ve ever wondered why some people seem superhuman on minimal sleep, or secretly hoped there was a way to train your body to do the same, this discovery might just hold the answers. Let’s explore what makes natural short sleepers tick—and whether this sleep “superpower” is something the rest of us can unlock too.
For years, sleep specialists have repeated the same mantra: adults require a minimum of 7 to 9 hours of quality sleep each night to maintain mental acuity, immune function, and cardiovascular health. Long-term sleep deprivation has long been associated with higher risks of obesity, Alzheimer's disease, high blood pressure, and even premature death. But what if some people are genetically predisposed to perform best on only four hours of sleep?
Recent scientific studies have put this astounding phenomenon under the limelight with a stunning finding: an exceptional gene mutation, SIK3-N783Y, that makes some individuals what scientists have coined as natural short sleepers.
Who Are These Super Sleepers?
A natural short sleeper (NSS) is one who sleeps four to six hours every night but wakes up feeling refreshed and ready to go—without the help of coffee or the typical symptoms of sleep deprivation. They are not sleep-deprived; their bodies simply need less sleep than others.
This fascinating sleep pattern has puzzled scientists for decades, but thanks to a recent study by researchers from the Chinese Academy of Sciences, the enigma is starting to lift. Their results, which were published in a peer-reviewed journal, indicate a rare gene mutation in the salt-induced kinase 3 (SIK3) gene.
Can You Really Survive—and Thrive on Just 4 Hours of Sleep?
The scientists discovered that the N783Y mutation in the SIK3 gene alters the SIK3 protein structure. This alteration affects the protein's function to transfer phosphate molecules, an essential component of the chemical signaling that governs our internal sleep-wake cycles.
In order to better analyze this effect, researchers created genetically modified mice that had the same mutation. Such mice slept around 30 minutes less per night than regular mice, and even less when deprived of sleep. Surprisingly, these differences weren't associated with the amount of proteins in the brain—but rather, with the way the proteins worked.
Furthermore, mutant mice had higher delta wave activity on EEG readings—a sign of deep, restorative sleep. This reinforces the theory that the mutation doesn't merely cut short sleep, it makes it more effective.
This is not the first time that scientists have associated genetics with sleep duration. Several years back, one mother and daughter who claimed to require just six hours of sleep at night without ever getting tired were discovered to carry a mutation in a gene linked with the circadian clock, our internal sleep- timing mechanism.
So far, scientists have discovered at least five mutations in four genes that affect sleep duration. But the newly found SIK3 mutation is particularly intriguing because it directly affects biochemical pathways that can now be targeted in the future development of drugs.
How Does this Gene Affect Sleep Medicine?
The applications of this research are vast. By knowing what enables natural short sleepers to feel rested on less time, researchers can start working on the development of treatments to improve sleep quality—not by lengthening time, but by increasing the efficacy of the hours we do spend sleeping.
"This discovery deepens our knowledge of the genetic basis of sleep," researchers said, highlighting the mutation's promise in leading to precision sleep medicine—focused treatments that modify sleep regulation systems at the molecular level.
Natural Short Sleep vs. Sleep Deprivation
Natural short sleep is a genetically controlled, rare condition in which people perform best with only 4–6 hours of sleep. In contrast to sleep-deprived individuals, they rise feeling rested, with no hint of exhaustion or mental slowness. This is not about "toughing it out" on fewer z's—it's simply the way their bodies are biologically programmed to require less. Sleep deprivation has an impact on mood, memory, immunity, and cardiovascular health. Long-term sleep deprivation has been known to increase disease risks like Alzheimer's or cardiovascular disease. Thus, when natural short sleepers are prospering, the rest of us should not try to replicate their sleep.
Why Most People Still Need 7 to 9 Hours of Sleep?
Most people still require 7 to 9 hours of sleep because it maintains critical functions such as memory consolidation, emotion regulation, immune function, and cell repair. Sleep removes toxins from the brain and re-sets the body's biological clocks for the day ahead. Sleeping less than required on a regular basis can hamper concentration, decision-making, and metabolism and result in long-term dangers including obesity, cardiovascular disease, and dementia. Although a small group of people have a genetic mutation that enables them to survive on less sleep, the rest of us are not so hardwired and require sufficient sleep to maintain physical, mental, and emotional health.
Why You Shouldn't Deprive Yourself of Sleep?
Before you begin reducing your sleep time, it's important to observe, natural short sleep is different from sleep deprivation. The majority of us cannot just train ourselves to be short sleepers. For most people, trying to sleep just four hours a night results in cognitive impairments, memory loss, compromised immunity, and long-term health problems.
Rather than copying the sleep habits of the genetically fortunate few, experts advise taking efforts at sleep hygiene:
- Stick to a regular sleep schedule, even on weekends.
- Avoid caffeine and heavy meals in the evening.
- Make the sleeping environment cool, dark, and quiet.
- Limit screen use before bedtime.
- Deal with stress through meditation or journaling.
While the discovery of the SIK3-N783Y mutation may not mean much for your sleep schedule today, it opens exciting doors for future treatments and a deeper understanding of how our bodies regulate rest. It also highlights the fascinating diversity of human biology—some people are literally wired to need less sleep, and now, we’re beginning to understand why.
So, if you wake up feeling great on only a few hours of sleep each night, science may one day validate that you're one of a select, genetically privileged few. In the meantime, shoot for that 7-9 hour mark your body and mind will appreciate it.
Norovirus 2025: Is There A Vaccine For The Stomach Bug Spreading This Year?

Credits: Canva
Dozens of norovirus outbreaks have been recorded nationwide over the past few weeks, and as people deal with intense vomiting, diarrhea, and other uncomfortable or even risky symptoms, a common question keeps coming up: why is there still no vaccine for such a widespread infection.
The Centers for Disease Control and Prevention (CDC) says norovirus cases are increasing toward the end of 2025, with higher activity reported in both the US and the UK. Health officials note that a new, highly infectious strain known as GII.17 is partly driving this rise. Because many people have little or no immunity to it, outbreaks are being seen more often in schools and shared public spaces. While overall case numbers remain within typical seasonal ranges, recent weeks have shown a clear upward trend.
What Is Norovirus?
Norovirus is an extremely contagious virus that leads to gastroenteritis. It commonly causes symptoms such as vomiting, diarrhea, nausea, and stomach cramps, and may also bring fever and body aches. It is often referred to as the ‘stomach flu,’ though it has no connection to influenza.
The virus spreads quickly through contaminated food or water, shared surfaces, or direct contact with an infected person’s vomit or stool. Crowded settings like cruise ships are especially vulnerable. Most people recover within one to three days with rest and enough fluids, according to the CDC.
Norovirus Symptoms 2025
Norovirus usually comes on suddenly, causing vomiting, watery diarrhea, nausea, and abdominal pain. Fever, headaches, and body aches are also common. Symptoms typically appear 12 to 48 hours after exposure and last for one to three days. Because it spreads so easily, infections can move fast through families and communities.
While most cases improve on their own, dehydration is a concern, so warning signs such as intense thirst or reduced urination should not be ignored, as noted by the Cleveland Clinic.
Do We Have A Norovirus Vaccine?
At present, there is no widely available vaccine for norovirus. That said, research has made meaningful strides. Experimental oral vaccines have shown encouraging results in clinical studies, suggesting they may offer protection against multiple fast-changing strains and help reduce how much virus an infected person sheds. Scientists are hopeful that an effective, broadly protective vaccine may become available in the coming years, according to the National Institutes of Health.
Why Don’t We Have a Norovirus Vaccine Yet?
Developing a vaccine for norovirus has proven especially difficult, largely because of how quickly the virus changes. “It really is evolving extremely rapidly, and that’s a big problem,” Patricia Foster, PhD, professor emerita of biology at Indiana University Bloomington, told Health.
Norovirus also exists in dozens of subtypes, with several dominant strains circulating at any given time. This is why people can catch norovirus more than once in their lives. Even if immunity develops against one strain, either after infection or through vaccination, another strain can still cause illness. Centers for Disease Control and Prevention. About norovirus.
Norovirus: Multiple Vaccines Are In The Works
Despite these obstacles, vaccine research is moving forward. Progress has accelerated in part because of newer technologies developed over the past decade. In 2016, Mary Estes, PhD, a researcher at Baylor College of Medicine, and her team found a way to grow norovirus outside the human body. This breakthrough made it possible to test vaccine approaches and treatments more effectively. This step was crucial because common lab animals like mice do not typically get sick from human norovirus.
Today, scientists are testing several experimental vaccines. One example is a 2023 vaccine developed at Washington University School of Medicine in St. Louis that combines protection against norovirus with an existing rotavirus vaccine. Several pharmaceutical companies are also developing candidates, many of which are now in clinical trials, said Amesh Adalja, MD, senior scholar at the Johns Hopkins Center for Health Security, in comments to *Health*.
HilleVax, a Boston-based company, has been testing a norovirus vaccine originally developed by Japan’s Takeda. However, that candidate did not succeed in a phase II trial in June 2024. Meanwhile, a tablet-style norovirus vaccine from San Francisco-based Vaxart has completed phase I testing. Among the most promising efforts is Moderna’s vaccine, which is currently being tested in human volunteers.
Preventing Norovirus, Even Without a Vaccine
Norovirus spreads so easily that stopping it once someone falls ill can be very challenging. This is linked to the virus’s structure. Norovirus is a nonenveloped virus, similar to polio and other stomach-related infections. Because of this, neither hand sanitizers nor soap and water actually destroy the virus, Foster explained. “Handwashing helps because you’re physically rinsing the virus away,” she said.
As a result, basic hygiene practices, especially thorough handwashing, remain some of the most effective ways to lower risk, said Ming Tan, PhD, an infectious disease researcher and associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center, speaking to *Health*.
If norovirus does strike, treatment options are limited. Staying hydrated is essential to avoid complications from fluid loss. Some people may also use medicines to control nausea or diarrhea, either over the counter or by prescription, such as Zofran. If severe symptoms develop, including confusion, high fever, or intense abdominal pain, medical care should be sought right away.
Mystery Disease Adenovirus: New Virus Said To Be Stronger Than Covid And Flu — All You Need To Know

Credits: Canva
Adenovirus: A newly emerging “untreatable” mystery virus that is being described as stronger than Covid is now spreading across several parts of the world, with experts warning that even common disinfectants may not be effective against it. Known as adenovirus, the infection causes symptoms similar to a severe bout of flu, such as shortness of breath, a runny nose, and a sore throat. What sets it apart, however, is the limited treatment available.
In most cases, people who contract the virus have no option but to manage symptoms and allow the illness to pass on its own. The good news is that adenovirus infections are usually mild. That said, much like Covid or seasonal flu, the risk rises for people with weakened immune systems, who may experience more serious complications, according to a report by The Mirror.
Jefferson Health’s medical director of infection prevention and control, Eric Sachinwalla, has cautioned that unlike more familiar viral infections, there is very little doctors can do to actively treat adenovirus.
What Is Adenovirus?
Adenoviruses belong to a broad family of common viruses that can affect multiple parts of the body, including the airways and lungs, eyes, digestive system, urinary tract, and even the nervous system. They are a frequent cause of fever, cough, sore throat, diarrhoea, and conjunctivitis. Most infections tend to be mild and clear up on their own within a few days. However, health experts are now noting a rapid rise in cases, with the virus spreading quickly and leaving large numbers of people unwell.
The virus is particularly contagious because it is tougher than many others. Routine cleaning with soap and water or standard disinfectants may not be enough to eliminate it, allowing it to survive longer in the environment. This is why outbreaks are often seen in places such as day-care centres and military barracks, where close contact is common. Adenovirus spreads through respiratory droplets, can be passed through stool, and can linger on contaminated surfaces for extended periods, as per Mirror.
Adenovirus Symptoms
Symptoms of adenovirus infection can vary widely. Common signs include shortness of breath, a runny nose, and a sore throat. Some people may also develop diarrhoea or pink eye. The wide range of symptoms is partly due to the fact that there are more than 60 known strains of the virus.
Adenovirus: How Is Adenovirus Different From Covid And Flu?
Adenoviruses, like coronaviruses, spread from person to person and can trigger similar respiratory symptoms. However, they belong to entirely different virus families and behave differently. One key difference is resistance. Coronaviruses are more easily destroyed by disinfectants, while adenoviruses are harder to kill, which allows them to spread more easily than Covid or flu.
For otherwise healthy individuals who feel unwell but do not have severe symptoms such as high fever or breathing difficulty, recovery usually happens at home with basic supportive care. Medical attention is more important for people with weakened immunity, parents of very young infants, or those with existing conditions like heart or lung disease. If symptoms appear, experts advise against walking straight into a clinic. Calling ahead is safer, as doctors may recommend a telehealth consultation if the illness seems highly contagious.
Adenovirus: Is Adenovirus Untreatable?
Most adenovirus infections are mild and resolve without medical treatment. However, if symptoms linger or worsen, there is often little doctors can do beyond monitoring and symptom relief, as the virus largely needs to run its course. Following basic hygiene measures, such as washing hands regularly and cleaning frequently touched surfaces, remains one of the most effective ways to reduce the risk of infection.
What Is The Experimental HIV Drug Charlie Sheen Says Suppressed The Virus In His Body?
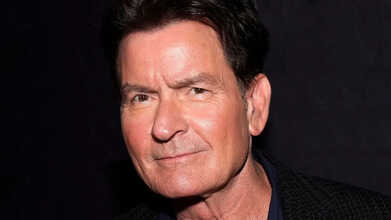
Credits: AP
Though Charlie Sheen’s HIV has been described as “completely manageable,” the actor recently shared that he once came across a treatment he believed worked far better than existing options, but it never reached the public. Speaking on the *Howie Mandel Does Stuff* podcast, the 60-year-old actor reflected on an experimental drug he used years ago and explained why it ultimately disappeared from view. “There was one that was really good that I was hoping would come to market one day, and it never did,” said Sheen, who publicly disclosed his HIV diagnosis in 2015. This has raised a key question: which experimental drug is Charlie Sheen referring to?
What Is HIV?
Human immunodeficiency virus, or HIV, is a virus that attacks the immune system. If left untreated, it can progress to acquired immunodeficiency syndrome, or AIDS, which represents the most advanced stage of infection. HIV primarily targets white blood cells, weakening the body’s natural defences. The virus spreads through unprotected sexual contact, sharing needles for drug use, exposure to infected blood, and from parent to child during pregnancy, delivery, or breastfeeding.
What Does HIV Do To A Person?
HIV infects CD4 cells, also known as helper T cells, which play a central role in immune response. As the virus destroys these cells, the white blood cell count drops, leaving the body vulnerable to infections it would normally fight off with ease.
Early on, HIV can cause flu-like symptoms. After that, it may remain hidden in the body for years without obvious signs, while continuing to damage the immune system. When CD4 levels fall very low, or when certain serious infections develop, HIV is considered to have progressed to AIDS.
At this stage, symptoms may include rapid weight loss, severe fatigue, sores in the mouth or genitals, recurring fevers, night sweats, and changes in skin colour.
Charlie Sheen Claims An Experimental Drug That Works Better For HIV
During the podcast conversation, Sheen named the drug he believes made a major difference. “That was a thing called PRO 140,” he said. He described it as a monoclonal antibody that produced faster and more consistent results, with fewer side effects than standard treatments. When asked why it never became widely available, Sheen suggested it may have posed a threat to existing therapies. “It works, better than what they have,” he said, adding that the company behind it ran into serious trouble. Mandel responded that someone should investigate further, a point Sheen agreed with.
What Is The Experimental Drug Charlie Sheen Is Talking About?
PRO 140 is a humanised monoclonal antibody designed to block CCR5, a receptor HIV commonly uses to enter human cells and replicate. Around 70 percent of people living with HIV in the United States, and as many as 90 percent of newly diagnosed patients, carry CCR5-tropic strains of the virus.
Earlier studies found that a single intravenous dose of PRO 140 sharply reduced HIV levels, while weekly injections under the skin lowered viral load much more effectively than a placebo. Research also suggested that the drug did not interfere with normal immune functions linked to CCR5.
According to Aidsmap, PRO 140 was generally considered safe and well tolerated. Although more than 90 percent of participants in extended studies reported side effects, there were no serious adverse reactions linked directly to the drug, and no one had to stop treatment because of it. The reported side effects were limited to injection-site reactions, which were usually mild to moderate.
Sheen has repeatedly spoken about his experience with the drug, maintaining that it delivered steadier results and caused fewer side effects than conventional HIV treatments.
© 2024 Bennett, Coleman & Company Limited

