- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Becoming Forgetful With Age? Signs That Tell It's 'More Serious' Than Just Aging
Credits: Canva
Who hasn't ever forgotten a friend's name, lost their glasses, or had trouble remembering a word that was just "on the tip of the tongue"? These little memory blips are normal, particularly with age. But with increasing awareness about dementia and cognitive decline, even occasional forgetfulness can raise alarm. Is it just aging or something worse?
Though periodic memory loss is a natural aspect of aging, distinguishing it from the onset of dementia is important to ensure early intervention. Here's a closer examination of when forgetfulness is harmless—and when it might require medical attention.
What are Normal Age-Related Memory Changes?
Aging brings natural changes to our bodies and brains. Known as age-associated memory impairment, these changes are mild and don’t interfere with day-to-day function. According to the World Health Organization (WHO), healthy aging is about maintaining functional ability and well-being even as biological changes occur.
With normal aging:
- You may occasionally forget names or appointments, but remember them later.
- Multitasking becomes harder, and it may take longer to learn new things.
- Concentration can decline, particularly in distracting settings.
These changes are generally more irritating than distressing. Most importantly, most elderly persons maintain independence, functional memory, and the capacity for engaging in meaningful activities.
What are Dementia-Related Memory Changes?
Dementia is not a normal aspect of aging. It is a medical illness that includes a gradual loss of memory, thinking, behavior, and the capacity to carry out daily activities. Alzheimer's disease is the most prevalent type, but there are numerous others—such as vascular dementia, Lewy body dementia, and frontotemporal disorders.
The main differences between aging and dementia:
- In typical aging, you might forget some aspect of an experience. With dementia, whole experiences are forgotten.
- Dementia entails persistent, deteriorating problems with communication, decision-making, orientation, and even personality.
- Healthy older adults are usually conscious of their forgetfulness, but individuals with dementia may not have insight into their own deterioration.
Signs Your Forgetfulness May Be More Than Aging
Some indicators transcend normal memory slips and might signal an underlying cognitive disorder. Let's examine the most revealing differences:
1. Memory Changes
Normal: Occasionally forget names or appointments.
Concerning: Forget recent things, repeat oneself, or get lost in familiar settings.
2. Language Challenges
Normal: Struggle briefly to name something.
Concerning: Often lose train of thought, use wrong words, or have trouble keeping up.
3. Problem Solving & Decision Making
Normal: Need more time to make decisions.
Concerning: Struggle to manage finances, prepare meals, or organize activities previously done easily.
4. Decline in Independence
Normal: Continue with home maintenance and personal care.
Concerning: Need assistance with dressing, bathing, medication, or bill payment.
5. Disorientation
Normal: Remember occasionally where you placed something or the date.
Concerning: Disoriented about place, time of day, or season.
6. Personality & Mood Changes
Normal: Minimal mood shifts in reaction to life events.
Concerning: Unusual irritability, paranoia, or avoiding social activities.
7. Social Withdrawal
Normal: Prefer solitude at times.
Concerning: Refuse interaction because you are confused or cannot keep up with conversation.
8. Lack of Awareness
Normal: Acknowledge your forgetfulness and learn how to make up for it.
Concerning: Deny or are unaware of decline even when pointed out by others.
9. Progressive Pattern
Normal: Changes are not frequent and don't progress quickly.
Concerning: Symptoms become worse—from intermittent lapses to persistent confusion and dysfunction.
Other Causes of Memory Loss You Ought Not to Ignore
All memory issues aren't due to dementia. Some reversible or treatable conditions cause similar symptoms:
- Nutritional deficiencies (e.g., vitamin B12)
- Thyroid or liver dysfunction
- Side effects of medications
- Chronic depression, anxiety, or stress
- Untreated sleep apnea or insomnia
- Head injury or concussion
- Alcohol or drug abuse
- Infections or tumors of the brain
A full assessment by a medical provider is necessary to ascertain the cause.
What Is Mild Cognitive Impairment (MCI)?
Mild Cognitive Impairment occupies the place between normal aging and dementia. People with MCI have observable memory or thought problems that surpass typical age-related decline—but are still capable of independent living. MCI will either stay the same, or in some cases, will worsen to Alzheimer's disease.
Things You Can Do to Help Brain Health
If you or the person you care about is undergoing cognitive changes, these measures will assist in sustaining function and quality of life:
Maintain routines: Regular daily routines aid in memory and minimizing confusion.
Organize yourself: Use notes, calendars, or cell phone reminders.
Challenge your mind: Read, play puzzles, or take up a new hobby.
Stay connected socially: Social isolation may worsen cognitive decline.
Physical exercise: Regular exercise increases blood flow to the brain.
Prioritize nutrition: Consume a well-balanced diet that includes plenty of vegetables, omega-3s, and antioxidants.
Get quality sleep: 7–9 hours at night.
Manage chronic conditions: Maintain diabetes, hypertension, and cholesterol control.
When to See a Doctor?
If memory issues begin affecting your or a loved one's day-to-day activities, it's time to seek help. Signs include:
- Getting lost in familiar areas
- Having trouble with personal care
- Repeating stories or asking the same questions
- Having trouble managing money or medications
Don't jump to conclusions but don't wait. A timely diagnosis provides for more effective planning, care, and in some instances, treatment which can halt progression.
Aging has its own unique changes, yet not all forgetfulness indicates an urgent issue. Nevertheless, knowledge and initiative make a world of difference. Educate yourself about the signs, pay attention to your body and never be afraid to consult professionals. Caught early, most factors behind memory problems can be solved, allowing you or your loved one the utmost opportunity for a healthy, well-lived life.
1 In Every 8 School-going Children Is Obese In Kolkata: Study

Credits: LinkedIn; Canva
1 in every 8 child in Kolkata school between the age of 12 to 16 is obese. A new study conducted in Kolkata schools by a global obesity awareness organization revealed this data. Wednesday, the same day as Holi in India, was also the World Obesity Day. In Kolkata, the issue is concerning, especially when children are at the center of it. The Howrah bridge also lit with blue and yellow lights, the colors to symbolize obesity awareness.
What Did The Study Reveal About Obese Children?
An initiative by METTA Dana Foundation, a global academic outreach organization with its focus on childhood obesity revealed the rising case of childhood obesity in Kolkata. "Childhood obesity is rising rapidly, with the prevalence among school-aged children increasing from 4% in 1975 to almost 20% in 2022," said Debashis Basu, endocrinologist and chairman of METTA Dana Foundation. This is seen as a five-fold increase over five decades.
Basu further said, "The rise is sharpest in low-and-middle-income countries like India and Bangladesh. Childhood obesity often continues into adulthood, increasing the risk of serious non-communicable diseases, such as diabetes, heart disease and certain cancers." Basu also said that 13 per cent of such cancers are related to childhood obesity.
He said that early signs of chronic diseases are already appearing in children. He also noted that around "a fourth of Kolkata's children are diabetic or are in a pre-diabetic stage".
Obesity In Young People
Globally, as per a Lancet study, more than half of all adults and a third of children and adolescents will become overweight by 2050. The study also notes that obesity is becoming a bigger concern and it could impact around 21.8 crore men and 23.1 crore women in India.
In fact, India is projected to have world's second highest number of obese kids and adolescents, aged between five and 14 years. This means around 16 million boys and 14 million girls could be overweight.
One of the biggest challenges of being overweight is diabetes, as Basu also noted. In a previous conversation with Health and Me Dr Mayank Lodha Seth, chief pathologist at Redcliffe Labs, noted that diabetes is no longer a disease of aging, young people, including teenagers too are affected.
Also Read: Diabetes No Longer A Disease Of Aging; Four Things Youth Should Know About It, According To Doctor
"We took this initiative to revive it [World Obesity Day] this year with support from National Institute of Nutrition. India is beginning to face the triple burden of malnutrition, stunting and wasting, micronutrient deficiencies, and obesity- often coexisting in the same family or the same person in various stages," said Basu.
Why Is India Facing A Crisis In Youth Obesity?
According to UNICEF’s Child Nutrition Global Report 2025, obesity, for the first time, surpassed underweight globally as the most common form of malnutrition among school-aged children and adolescents.
According to the National Family Health Survey (NFHS) data, India is witnessing a rapid surge in overweight and obesity among under-five children under five, with prevalence rising by 127 per cent (from 1.5 per cent to 3.4 per cent between NFHS 3 (2005-06) and NFHS 5 (2019-21). Similarly, adolescent girls and boys have seen an increase in overweight and obesity of 125 per cent (from 2.4 per cent to 5.4 per cent) and 288 per cent (from 1.7 per cent to 6.6 per cent) respectively.
A recent child nutrition report points to a worrying shift in the way young people in India eat. Fast foods, ultra-processed snacks, and sugary drinks that are high in fat, salt, and sugar are steadily replacing fruits, vegetables, and traditional home-cooked meals. These choices are not always driven by taste alone. Easy availability and aggressive marketing campaigns aimed at children and teenagers are increasingly shaping what they want to eat.
Early-life factors are also playing a role in the rising numbers. Poor maternal nutrition during pregnancy, inadequate infant feeding practices, and low rates of exclusive breastfeeding can influence a child’s long-term health and metabolism. Social and gender norms add another layer to the problem. In many households, adolescent girls and women still eat last and often the least, which can affect nutritional balance early in life and contribute to unhealthy patterns later.
At the same time, lifestyles among young people are rapidly changing. The growing consumption of ultra-processed foods and sugar-sweetened beverages is being combined with lower levels of physical activity. Children and teenagers today spend more time on screens, whether for schoolwork, entertainment, or social media, leaving less time for outdoor play and movement. This shift towards sedentary routines is one of the key reasons obesity is increasing among the younger population.
The environment around food is also changing. Urban areas and even smaller towns are now saturated with packaged and processed food options that are quick, cheap, and heavily promoted. When healthier choices are less visible or less accessible, children and adolescents are more likely to gravitate toward convenient, calorie-dense products.
Data from UNICEF’s U-Report poll, which surveyed adolescents and young adults aged 13 to 24 across 171 countries, highlights the scale of marketing exposure. More than two-thirds of young people said they regularly encounter food advertisements. In the week before the poll, 75 per cent reported seeing ads for sugary drinks, fast food, or packaged snacks. Social media was the biggest source of exposure at 52 per cent, followed by the internet at 46 per cent and television at 43 per cent. Not surprisingly, three in five respondents admitted that these advertisements made them want to try the products they saw.
Experts say this constant exposure is shaping dietary habits from an early age. When young people repeatedly see unhealthy foods promoted as fun, trendy, or aspirational, it normalizes those choices.
Selena Gomez Was 'Misdiagnosed' Before Her Bipolar Disorder Diagnosis

Credits: Instagram
Selena Gomez recently opened up about being wrongly diagnosed for her mental health issues. The 33-year-old singer said that she was "misdiagnosed" before she ultimately received her bipolar disorder diagnosis.
She, along with her husband appeared on the podcast Friends Keep Secret, and said that she knew something was wrong with her. "I knew something was wrong, but I think I was misdiagnosed," Gomez said. "People were just assuming, and I would try multiple therapists. And that’s why it’s hard. It’s actually really hard when we’re talking about these things. And for me to go get a therapist, all of it is so f***ing complicated."
Going on to explain that finding the right diagnosis and treatments took going through "multiple different people," Gomez emphasized how important it was to remember that "you can’t just give up." Gomez also said she underwent therapies at four different rehabs, which helped her understand her diagnosis - a chronic mental health condition characterized by severe mood swings, alternating between extreme emotional highs and lows.
Therapy Should Not Be Shamed, Says Gomez
Gomez also slammed people who shame the idea of therapy. She said those people are hypocrites. "That's the problem with misconceptions," she said. "The whole hypocrisy of shaming people for therapy or people not understanding it is that it’s just not for you. That’s completely fine, but for me, it finally allowed me to go, ‘Oh, that’s why I handled things the way I handled them. That’s why all the other people were able to get over things so quickly, and I wasn’t.'”
“I would act out of fear, I would act out of love, I would act out of passion,” she added.
What Is Bipolar Disorder?
As per the American Psychiatric Association (APA), bipolar disorders are mental health conditions characterized by periodic, intense emotional states affecting a person's mood, energy and ability to function. APA notes that these periods, lasting from days to weeks, are called mood episodes.
Mood episodes are categorized as manic/hypomanic episodes when the predominant mood is intensely happy or irritable, or depressive episodes, when there is an intensely sad mood or the ability to experience joy or pleasure disappears. People with bipolar disorder generally have periods of neutral mood as well. When treated, people with bipolar disorder can lead full and productive lives.
But Don't Mood Fluctuations Happen To People Without The Disorder?
APA notes that while people without bipolar disorder could also experiences mood fluctuations, they are part of commonly lived experience and typically last hours rather than days. These mood fluctuations are also not accompanied by extreme changes in behavior or changes in functioning, such as difficulties with daily routines and social interactions. Bipolar disorder could also disrupt a person's relationships with loved ones and cause difficulty in working or going to school.
What Causes Bipolar Disorder?
Bipolar disorder usually runs in families, as 80 to 90 per cent of cases come from a relative with bipolar disorder or depression.
Environmental factors such as stress, sleep disruption, and drugs and alcohol may trigger mood episodes in vulnerable people. Though the specific causes of bipolar disorder are unclear, there are both biological factors, including a family history of mood disorders, psychotic disorders, and substance misuse, and environmental factors that increase the risk for bipolar disorder. The average age of onset is in the mid-20s.
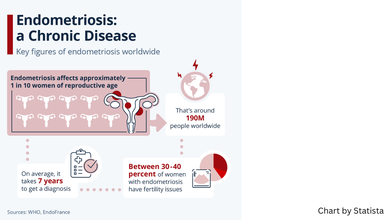
This Is Endometriosis, A Short Film On Debilitating Health Condition Wins BAFTA Award 2026, Know More

Credits: Instagram/ IMDb
This Is Endometriosis, a 2024 intimate, expressive film by Georgie Wileman and Matt Houghton won a BAFTA Award 2026 for Best British Short Film. This 19.27 minute long film shows how Georgie was robbed of her time due to endometriosis. The film sets in present-day narrative with memories from her past.
Endometriosis is a condition, that Georgie notes is often dismissed by many doctors as just "painful periods". However, her film portrays how truly disabling this medical condition. It is a condition in which cell similar to the lining of the uterus or the endometrium, grow outside the uterus. It affects 1 in 10 born with a uterus and could cause pain, often "worse than the last stages of child labour", notes thisiseno.com, the official website of the short film. Around 190 million people worldwide are impacted by the condition, however, what the film points out is how "dangerously underfunded, under researched and misinformed" doctors continue to remain despite the condition being so widespread.
Read: A Woman Lost Her Ovary To Endometriosis Surgery After Receiving An Ultimatum From Gynecologist
A Film That Documents Personal Struggle

Georgie, while accepting the award wore a symbolic blood-red gown. She said, "It was surreal and beautiful. Knowing how much this win would mean to the [endometriosis] community made it an emotional moment."
She points out that it is more than just a "painful period" and that "It is a full body disease. It important for people to understand the severity of the pain – it’s widely considered to be worse than childbirth." What is shocking is that it takes an average of eight to 10 years to be diagnosed.
She shares being "bed-bound for three months" when she was only 13. She said it first got "really bad" and she was not believed for long time. "It took me a long time to even believe myself. I was just so angry at my body for not working."
While she had been in and out of wheelchair, she was not formally diagnosed with endometriosis until she was 26, and then at 29, she was diagnosed with its 'sister disease' adenomyosis. She has undergone seven surgeries for her endometriosis and a hysterectomy for adenomyosis.
Read: Keltie Knight Was Gaslit By Doctors For Years Before Getting A Hysterectomy
In 2020, after years of feeling dismissed by doctors and watching her condition be misunderstood in the media, she decided she had had enough. That frustration pushed her to tell the story herself.
“It began as a photography project,” Wileman says. “And it meant a lot to people because, for the first time, they felt their experiences were being shown truthfully.”
But she soon realized that still images could only go so far. “There’s only so much a photograph can capture,” she adds.
Why Does It Take So Long For An Endometriosis Diagnosis?
A study published in Obstetrics and Gynecology journal looks at the factors of what leads to such a delay in endometriosis diagnosis. Researchers identified that factors include normalization of menstrual pain, the diversity of symptoms, and a lack of training and prompt referrals among healthcare professionals lead to this delay.
At an individual level, the researchers found that many women struggled to tell the difference between “normal” period pain and something more serious. A common belief was that painful periods were simply part of being a woman and had to be endured. As a result, many relied on self-care measures and delayed seeking medical help, which likely pushed back the timeline for an endometriosis diagnosis.
On an interpersonal level, stigma played a powerful role. Menstrual problems were often seen as too private or embarrassing to talk about. At the same time, society’s tendency to normalize period pain meant that symptoms were minimized, both by those experiencing them and by people around them. This silence and normalization further contributed to delayed diagnoses.
Barriers also existed within the healthcare system itself. Some participants said their general practitioners dismissed their concerns or appeared unfamiliar with endometriosis. Healthcare professionals involved in the study acknowledged gaps in their own training and pointed out the lack of clear clinical guidelines for diagnosing the condition.
Doctors also noted that endometriosis symptoms can overlap with other disorders, making it harder to identify. Diagnosis is particularly challenging because there is no simple, noninvasive test that can confirm the condition with certainty. Delays in referrals were common. One contributing factor was the widespread belief that laparoscopic surgery is the only definitive way to diagnose endometriosis. Some healthcare providers also questioned how useful a formal diagnosis would be, which further slowed the process.
Dr Sophie Davenport, a doctor in England who conducted the research as part of her Master of Public Health dissertation, emphasized that the problem is layered and requires solutions at multiple levels.
“The key highlights of the data are that delays to diagnosis exist throughout the journey,” she explained. “We need to address these at different levels — from society understanding what ‘normal’ menstruation looks like and being open about menstrual problems, to clinicians being well educated, up to date on how endometriosis presents and diagnosed, and truly listening when patients say their periods aren’t normal.”
© 2024 Bennett, Coleman & Company Limited

