- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Biohacker Bryan Johnson Swaps Out His Plasma To Reverse Aging; How Does It Work?

With new longevity science and health experiments, there is one individual at the forefront, Bryan Johnson, a tech billionaire-biohacker with a passion for reversing the clock. Renowned for spending more than $2 million a year on his own personal anti-aging routine, Johnson has pushed his crusade to new limits by having total plasma exchange (TPE)—a scientifically fascinating but highly controversial treatment that replaces the body's plasma with a substitute solution in an attempt to purify the body and, in Johnson's desire, reverse the clock.
Johnson, 47, was formerly in the headlines for injecting himself with his teenage son's plasma as part of what he called a "multi-generational plasma exchange." This was captured during the Netflix special Don't Die, which followed his extensive anti-aging trials, including plasma swapping with his father and son.
But as Johnson recently posted on social media, he has since switched from that headline-making habit. "I didn't give up because injecting your child's blood is creepy. I gave up because there's something that works better," Johnson tweeted.
That "something" is total plasma exchange (TPE)—a clinical-level process commonly compared to an "oil change" for the human body.
What Is Total Plasma Exchange?
Also referred to as therapeutic plasma exchange, or plasmapheresis, TPE is a procedure where the blood from a patient is taken out, broken down into its components (red cells, white cells, platelets, and plasma), and then the plasma is removed and replaced with a replacement fluid like albumin or donor plasma. The replacement fluid and the blood cells are then injected back into the body of the patient.
Having been used in hospitals for decades, TPE is already approved for conditions such as Guillain-Barré syndrome, myasthenia gravis, lupus, vasculitis, and even long COVID. New research now suggests that it has the potential to contribute to anti-aging, mental clarity, and immune system restoration—a path Bryan Johnson is heavily invested in.
What Happens When The Plasma Is Removed From Your Body?
Johnson's TPE treatment, as described by him, is to take out all his plasma and put in a 5% albumin solution and IVIG (intravenous immunoglobulin)—an extremely potent antibody-infused fluid usually reserved for bolstering or modulating immune function in immunocompromised individuals.
His treatment follows a bi-weekly routine involving two plasma exchange sessions, and then IVIG infusions that are four days apart. For each session, Johnson's team takes extensive baseline measurements, ranging from toxin concentrations to organ age to even microplastic levels.
In an interesting twist, Johnson asserts that his plasma was so exceptionally pure—presumably because of his stringent vegan diet, sleep habits, and supplement protocol—that the medical technician running the TPE machine "couldn't bring himself to throw it away."
What Is Albumin?
Albumin is the most prevalent protein found in human blood plasma. It has a primary function in tissue repair, transportation of nutrients, and fluid regulation. In TPE, it's the primary replacement fluid because it's compatible with human physiology and has a supporting role to preserve normal body functions after plasma removal.
Johnson feels that substituting his plasma with albumin provides a more efficient way of removing "unnatural pollutants" from the body—something that he believes is crucial in lowering biological age and avoiding age-related disease.
How Plasma Exchange Fights Aging?
The theoretical attraction of plasma exchange among longevity communities is that it has the ability to eliminate pro-inflammatory factors, toxic proteins, and defective antibodies that accrue over aging. Mice studies have established that the elimination of old plasma can trigger rejuvenation of organs and improved cognitive function—inspiring hopes for the same in humans.
According to proponents, removing plasma and replacing it can:
- Reduce systemic inflammation
- Enhance metabolic function
- Increase energy and mental acuity
- Boost immune system strength
While the area has not yet seen large-scale human studies, preliminary data and anecdotal results, like those of Johnson, are fueling increasing interest in TPE as a research anti-aging intervention.
TPE isn't for the faint of wallet. The cost of each session ranges from $5,000 to $10,000, and insurance usually doesn't cover the treatment unless it's for a condition approved by their organization. Johnson, who cashed out his payment firm Braintree to PayPal for $800 million, can finance his curiosity—and he's doing it on a very public platform.
Side Effects and Risks of Plasma Exchange
As with any surgical procedure, TPE has its own risks and side effects, which include:
- Fatigue and nausea
- Tingling of the hands, feet, or lips
- Risk of low blood pressure, low calcium, or anemia
- Occasional complications such as bleeding, infection, or syncope
Because it is a complex procedure, it needs experienced professionals and sterile equipment—the procedure is usually done in specialized hospitals or clinics.
How Does It Add To Longevity?
While Bryan Johnson’s approach might seem extreme to some, it’s pushing the boundaries of what modern medicine knows about aging and regeneration. Whether plasma exchange will emerge as a validated fountain of youth or remain a fringe biohacking trend remains to be seen.
Johnson, though, is convinced the proof is "emergent" and that his protocol could revolutionize our conception of aging. "I now have a birthday every 19 months," he asserts, quoting a deceleration of his biological aging rate to only 0.64, based on measurements taken by his team.
Johnson’s journey—from son-to-father blood swaps to high-tech plasma exchange—may seem eccentric, even controversial. But it shines a spotlight on a fundamental question facing medicine and humanity alike: What if aging isn’t inevitable?
His approach may not yet be mainstream or universally accepted, but it's certainly forcing a larger conversation about the future of personalized medicine, regenerative therapies, and how far we’re willing to go in pursuit of youth.
Is Hormone Replacement Therapy (HRT) A Boon To Women's Health During Menopause? | Women's Day Special

Credit: iStock
The 20th-century modernist writer Virginia Woolf, in her book 'Mrs Dalloway', published in 1925, described her 52-year-old protagonist Clarissa Dalloway feeling “shriveled, aged, breastless”, during menopause.
Even after decades, the experience continues to remain widely relatable for scores of women worldwide.
In January this year, author Twinkle Khanna compared menopause to “a phone with a faulty charger.” Several other celebrities, namely Naomi Watts, Oprah Winfrey, Gwyneth Paltrow, and Angelina Jolie, have voiced out their concerns and frustration that women face during the transition.
Menopause is a natural transition in a woman’s life, typically occurring between the ages of 45 and 55. But for millions of women around the globe, its symptoms, which range from hot flashes to night sweats to mood changes and sleep variations, can wreak havoc, affecting professional life, relationships, and physical and mental health.
Hormone replacement therapy (HRT) can be the answer to help ease the symptoms, which are often misunderstood, under-discussed, and sometimes unnecessarily feared.
“Hormone Replacement Therapy (HRT) is an evidence-based option that helps restore hormonal balance during this transition. It is highly effective in relieving menopausal symptoms, improving quality of life,” Dr. Parjeet Kaur, Associate Director, Endocrinology & Diabetes, Medanta, Gurugram, told HealthandMe.
What Is Menopause?
Menopause marks the end of reproductive years for a woman. It occurs when a woman permanently stops menstruating.
Clinically, menopause is diagnosed after 12 consecutive months without a menstrual period.
Most women experience menopause between the ages of 45 and 55, though the transition -- called perimenopause -- can begin several years earlier.
During this time, the ovaries gradually produce less estrogen and progesterone, the hormones that regulate the menstrual cycle. This hormonal decline leads to a range of symptoms, which vary widely among women.
“Menopause is a natural part of biological ageing. It can also be due to medical or surgical procedures. Most women go into menopause between 45 and 55 years,” Dr. Shilpa Agarwal, Consultant Gynecology and Obstetrics and Fetal Medicine Expert, Jaslok Hospital and Research Centre, Mumbai.
“Menopause is caused by the loss of ovarian follicular function and, consequently, a decline in the circulating blood estrogen levels. Natural menopause is deemed to have occurred after 12 consecutive months without menstruation for which there is no other obvious physiological or pathological cause and in the absence of clinical intervention,” she added.
Common symptoms include:
- Hot flashes and night sweats
- Sleep disturbances
- Mood changes and irritability
- Vaginal dryness
- Reduced libido
- Difficulty concentrating
- Weight gain or metabolic changes
While some women experience only mild symptoms, others find that menopause significantly affects their quality of life.
More than the uncomfortable symptoms, the drop in estrogen levels raises a slew of health issues, mainly osteoporosis, heart disease, and sometimes metabolic disorders.
Although regular health checkups, balanced nutrition, and physical activity during midlife are essential to sail through, HRT can play a huge role.
What Is Hormone Replacement Therapy? How Can It Help?
Hormone replacement therapy consists mainly of female hormones, typically estrogen alone or a combination of estrogen and progesterone.
Former First Lady of the US, Michelle Obama, in her podcast in 2020, spoke candidly about her experience of hot flashes.
She described it as a "furnace turning on in her core", and a host of other issues after which she resorted to HRT to maintain her health and lifestyle during that transition.
“Hormone replacement therapy replenishes women with ovarian hormones. HRT typically combines estrogen and progesterone therapy. Progesterone is required in women with an intact uterus to prevent endometrial hyperplasia,” Dr. Agarwal said.
The medications primarily help in
- Reducing hot flashes and night sweats
- Improving sleep and mood
- Treating vaginal dryness and discomfort
- Importantly, HRT helps prevent bone loss and fractures.
Dr. Kaur said that HRT is highly effective in relieving menopausal symptoms, improving quality of life, and supporting bone health by reducing the risk of osteoporosis.
Notably, it can be used in several forms, including pills, skin patches, gels, sprays, and vaginal creams or rings.
Dr. Agarwal recommended that women start HRT within 10 years of menopause or before the age of 60 years".
The experts also advised women to keep monitoring for side effects during HRT.
For many women with moderate to severe menopausal symptoms, HRT can be highly effective.
Studies show that beyond hot flashes, improving sleep, and restoring vaginal health, hormone therapy also
leads to:
- a 25 percent to 50 percent reduction in fatal cardiovascular events,
- a 50 percent to 60 percent reduction in bone fractures,
- a 64 percent reduction in cognitive decline.
Are There Any Risks Involved?
Despite its benefits, HRT has been the subject of debate for decades. Safety concerns intensified after a major US study in the early 2000s linked certain types of hormone therapy to increased risks of breast cancer, blood clots, and stroke.
However, in 2025, the US FDA removed all misleading warnings on the therapy.
Current medical guidelines generally suggest that HRT is safest for healthy women under age 60 or within 10 years of menopause, when used at the lowest effective dose for symptom relief.
“Modern HRT, when carefully selected and monitored, is considered safe for many women. The key is individualized care -- a thoughtful discussion with your doctor can help determine the most suitable approach based on your health profile, age, and personal preferences,” Dr. Kaur said.
Still, HRT may not be advisable for women with a history of:
- Breast or endometrial cancer
- Blood clotting disorders
- Stroke or heart disease
- Certain liver diseases
For these women, non-hormonal treatments -- such as certain antidepressants, lifestyle changes, and alternative medications -- may help manage symptoms.
Menopause is a new phase of life -- and with the right information and guidance, it can be navigated confidently and comfortably, Dr. Kaur said.
From First Period to Menopause: How Your Cycle Evolves Over the Years | Women's Day Special

Considered to be a key symbol of fertility and reproductive years, a woman's menstrual cycles are an integral and natural part of her life. However, they are more than just a monthly event, but instead a reflection of their hormonal, metabolic and even emotional health.
Due to genetics and other lifestyle factors, every woman experiences their cycle differently, which leaves many second-guessing about their hormonal balance, thyroid function, metabolic health, stress levels and even sleep quality.
Dr Archana Dhawan Bajaj, Gynaecologist and IVF Expert, Nurture exclusively tells Healthandme: "Knowing these patterns would guide people to understand when the changes are normal worry and when they are upheaval of a problem. Although the cycles vary among individuals, some features of such cycles are common between individuals, including the length of the cycle, flow, symptoms, as well as consistency, which are used to determine a normal state at various ages.
Here is what you should know and keep an eye out for during each phase:
The Early Years: Finding a Rhythm
Dr Maya PL Gade, Consultant, Gynaecology & Obstetrics at Kokilaben Hospital tells Healthandme: "In the first 2–3 years after menarche i.e. your first period, irregular cycles are common. Nearly 40–50 percent of adolescents do not ovulate consistently at first. The brain–ovarian hormonal axis is still maturing, so cycles may be longer than 35 days (than their typical 28 day monthly cycle) , bleeding may be heavy and cramps can feel intense.
Dr Rohan Palshetkar, Consultant IVF Specialist, Bloom IVF also warned that bleeding for more than 7–8 days continuously, soaking pads every 1–2 hours or going more than 90 days without a period may signal hormonal imbalance, clotting disorders, or conditions like PCOS.
He told Healthandme: "It is important to note that early teen cycles often happen without ovulation. For teenage girls, developing stable cycle will take some time due to ovaries adjusting to produce hormones. It is only in their late teens and early 20s that the girls will get the cycles more regular."
Normal Menstrual Cycle: According to Dr Bajaj, a normal cycle can be between 21 and 45 days. During bleeding, flow can be light, heavy, and cramps, mood swings, or even fatigue may accompany the adaptation of the organism to the hormonal changes.
Abnormal Menstrual Cycle: The expert explained: "Extensive bleeding, which needs the replacement of sanitary items every hour to two hours, long than seven or eight days, excruciating pain, or lack of periods in several months could be a sign of hormonal imbalance, thyroid complications, or polycystic ovarian syndrome."
20s and Early 30s: The Stable Phase
Talking about the post-teenager phase, Dr Gade said: "For many women, this is when cycles become more predictable, typically every 21–35 days, with 3–7 days of bleeding. Ovulation is more regular and PMS patterns are clearer. However, this is also the stage where lifestyle has a strong impact."
"Fertility is also at its peak in the 20s and early 30s, making it easy for women in this age group to become pregnant. With childbirth and breastfeeding, the chances of cycle alteration, its flow and length are high," Dr Palshetkar added.
Dr Gade also noted that high stress, poor sleep, intense exercise, crash dieting, thyroid disorders, or PCOS can disrupt ovulation and any sudden irregularity in this decade is often the body’s early warning system. A consistently painful period is also not “normal”, it may point to endometriosis or adenomyosis, both of which are frequently underdiagnosed,"
Keeping this in mind, it is essential for girls in their 20s and early 30s to track their period for regularity and flow, Dr Palshetkar advised.
Normal Menstrual Cycle: Dr Bajaj told this publication: "The average period to undergo a cycle is 21 to 35 days at an average of three to seven days with a moderate flow. The symptoms can be mild and include bloating, cramps or breast tenderness that can be easily treated."
Abnormal Menstrual Cycle: Talking about abnormal alterations, the gynaecologist said: "Excessive menstrual bleeding, cramps that impair normal life or inter-menstrual bleeding may be some of the early signs of endometriosis, fibroids, hormonal disruption or chronic stress."
Late 30s to 40s: The Hormonal Transition
Dr Gade explained: "Fertility begins to decline gradually after 35 due to reduced ovarian reserve. Cycles may shorten initially because ovulation happens slightly earlier. As women move into perimenopause, a transition that can last 4–8 years, hormone levels fluctuate unpredictably. Estrogen doesn’t simply drop; it rises and falls unevenly.
"This explains why many women notice heavier bleeding, clotting, worsening PMS, new-onset anxiety, sleep disturbances or cycles that skip months and then return. Studies suggest that up to 90 percent of women experience noticeable cycle changes during this phase.
"Importantly, very heavy bleeding at this stage should not be ignored. It can sometimes be linked to fibroids, endometrial thickening, or other structural changes in the uterus."
Moreover, Dr Palshetkar also warned: "For some, there is a noticeable and increasing gap between periods before menopause. Fertility decline is a reality in the age group, though it is not impossible to get pregnant.
Normal Menstrual Cycle: Dr Bajaj elaborated to Healthandme: "The hormonal shifts at this age may make the cycles a bit shorter or longer. Flow can either become thicker or thinner and premenstrual symptoms can be more pronounced as the body slowly transitions into perimenopause."
Abnormal Menstrual Cycle: Additionally, she said: "Very heavy bleeding, very prolonged intervals between the periods, bleeding following intercourse or sudden spotting between menstruation may be considered an issue, as these can be indicators of hormonal disorders, the presence of fibroids, or other gynecological problems."
Menopause: A New Baseline
Ultimately, Dr Gade detailed: "Menopause is diagnosed after 12 consecutive months without a period, with the average age globally around 50–51 years. Hormone levels stabilize at lower levels, and while periods stop, symptoms like hot flashes, vaginal dryness, bone density changes, and metabolic shifts may appear."
"Post-menopause, a woman’s reproductive health sees a significant decline of estrogen levels, fertility, and inability to produce any eggs. However, it still sees noticeable hormonal fluctuations and resultant health troubles.
"Facing PMS-like symptoms like mood swings and irritability is not uncommon. Medical attention is required when women notice severe pain or very heavy bleeding at
any age after menopause.
"The changes and evolution in the menstrual cycles are proof of her complete health during the course of the life she lives. And it impacts the way she lives or can live through her lifetime," Dr Palshetkar added.
Normal Menstrual Cycle: Lastly, Dr Bajaj said: "Prior to menopause, the cycles can become irregular since of the hormonal fluctuations and some symptoms like hot flushes, sleeping problems or mood swings can appear."
Abnormal Menstrual Cycle: While she noted that slight spotting is possible post-menopause due to fluctuations in estrogen and progesterone levels, the expert advised: "Post-menopausal vaginal bleeding is regarded as abnormal and needs to be medically examined because it may be due to underlying health conditions that must be addressed."
Hailey Bieber Revealed How A Mini Stroke At 25 Led To Her Discovering A Hole In Her Heart

(Credit - SHE MD Podcast/haileybieber/Instagram)
Hailey Bieber recently opened up about a mini stroke or Transient Ischemic Attack (TIA) she experienced when she was just 25. In an episode of the SHE MD podcast, hosted by Mary Alice Haney and Dr. Aliabadi, Hailey discussed how the mini stroke actually led her to find out an even bigger issue in her heart.
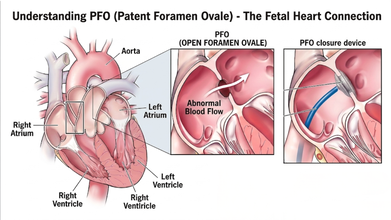
Dr. Aliabadi, a world-renowned OBGYN based in Los Angeles, who is also Hailey’s doctor, explained that this ordeal led Hailey’s medical team to discover a PFO, also known as a hole in her heart
In the interview, the founder of Rhode Beauty detailed how she had the classic stroke symptoms and said: “[My] whole right side of my arm went numb. I couldn't speak. Like my words were coming out all jumbled. The right side of my face was drooping. It was like a classic stroke symptom”
She explained that the reason why her team called it a mini stroke is because it ended within 31 minutes. By the time she reached the hospital, she didn’t need any clot busting medicine or procedure.

What Caused Hailey Bieber’s Mini Stroke?
Dr. Aliabadi explained that Patent Foramen Ovale (PFO) is extremely common phenomenon and a majority of people go through life never knowing they have it.
The Cleveland Clinic explains that the PFO is a small flap or opening between the upper chambers of your heart that everyone has. However, it usually closes up before the age of three. Most of the time, a PFO doesn’t cause symptoms and would not need treatment; however, in rare cases, it could lead to a stroke and or a TIA.
How Was Hailey’s Heart Condition Diagnosed
Hailey explained that her heart is slightly tilted in her chest and standard echocardiogram couldn't see the opening at first which led ER doctors to be unable to detect it.
As a result, she had to see a specialist for a Transcranial Doppler test. Doctors listened to the sound of blood "shunting" (moving the wrong way) through her heart to finally confirm the hole was there, which was much larger than they expected.
Also Read: Women Heart Symptoms Could Differ From Men, Explains Expert
What Is Transcranial Doppler Test?
According to the Cleveland Clinic, it is an ultrasound test that uses sound waves to detect conditions that affect blood flow to and within your brain. It can detect strokes caused by blood clots, narrowed sections of blood vessels, and numerous other heart-related issues.
How Did They Fix Hailey Bieber’s Heart?
Instead of an open-heart surgery, doctors performed a modern, minimally invasive procedure on Hailey's heart. She detailed the procedure where the doctors reached her heart through a vein in her groin. They threaded a tiny "button" made of metal and Teflon up to her heart and used it to securely plug the hole.
Hailey also learned she has some genetic factors that put her at a higher risk for blood clots and inflammation. Despite suffering a life-altering stroke, she views it as a "blessing in disguise" as it led her to find these issues early.
Now, she manages her health through a clean lifestyle, focusing on sleep, exercise and keeping her heart inflammation low.
© 2024 Bennett, Coleman & Company Limited

