- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Bjorn Borg Opens Up On His Struggle With Drug Overdose
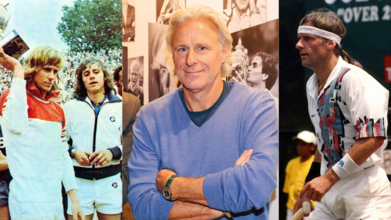
Credits: Wikimedia Commons
In his new autobiography Heartbeats, Björn Borg strips away the icy façade that once defined him on court. The book, set for U.S. release on 23 September by Diversion Books, begins with a raw account of his 1990s hospitalization after overdosing on “alcohol, drugs, pills, my preferred ways of self-medication.” It ends with a prostate cancer diagnosis, which he now faces in remission.
“It’s good,” the 69-year-old told The Associated Press in a recent video interview from his Stockholm home, “to have a good beginning and a good ending.” The 292-page memoir is a departure from the silence he cultivated during and after his playing days, offering stories of love, regret, excess and survival.
Walking away from tennis at 25
Borg retired shockingly early, at just 25, after losing both the Wimbledon and U.S. Open finals in 1981 to his rival John McEnroe. While others saw a glittering career still ahead, Borg knew otherwise.
“My head was spinning,” he said. “And I knew I’m going to step away from tennis.”
That decision, he explains, left him unmoored. He returned briefly to the professional circuit in the early 1990s but never again at Grand Slam level. What followed was a long descent into substance abuse.
On court, Borg was famously known as “Ice-Borg”, a man of composure who never flinched. But he reveals that this restraint was a learned skill, born from shame as a 12-year-old banned by his local club for bad behavior.
Off court, that discipline dissolved. By his own account, panic attacks and depression pushed him into cocaine use starting in 1982. “The first time I tried cocaine,” Borg writes, “I got the same kind of rush I used to get from tennis.”
The rush quickly became reliance. “It really destroys you,” Borg said of drugs. “I was happy to get away from tennis, to get away from that life. But I had no plan what to do. I had no people behind me to guide me in the right direction.”
Also Read: “Day by day, year by year,” Is How Bjorn Borg Takes Life After His Prostate Cancer Diagnosis
Overdoses and shame
Borg details two overdoses that landed him in hospital, one in Holland in the early 1990s, and another in 1989 in Milan, which he insists was an accident rather than a suicide attempt. The darkest moment, he admits, came when he awoke in a hospital bed to see his father looking down at him.
“That was the worst shame of all,” he writes.
These incidents, combined with spiraling personal struggles, forced Borg to confront how far he had fallen from the grace of his early sporting stardom.
Name: drops and surreal encounters
Heartbeats is not a typical sports autobiography. Alongside harrowing stories of addiction and recovery, Borg mixes in extraordinary encounters: a water-skiing shoulder injury before the 1977 U.S. Open, receiving death threats during the 1981 U.S. Open, being robbed at gunpoint after accepting payment in cash, and facing coin-throwing spectators in Rome.
The book name-drops Donald Trump, Nelson Mandela, Tina Turner, Andy Warhol, Yasser Arafat, and even “my old friend Hugh Hefner.” These anecdotes place Borg not only in tennis history but within a swirl of 20th-century celebrity and politics.
“People will be very surprised what really happened,” Borg said. “For me to come out after all these years, all I went through, I went through some difficult times, it’s a relief for me to do this book. I feel so much better. No secrets anymore.”
A candid look at survival
The memoir also traces his strained relationships, with parents, with his children, and with his own sense of identity after leaving professional sport. By his account, retirement robbed him of purpose, and drugs filled the void.
Borg acknowledges that his descent was partly a reaction to the structure of his tennis life: “I was happy to get away from tennis … but I had no plan what to do.” Without the rhythm of tournaments and training, he spiraled.
Yet he insists he has rebuilt his life. Now, after cancer treatment, he says he is proud of where he stands: sober, reflective, and still connected to the sport he once dominated.
Looking ahead, without secrets
For Borg, writing Heartbeats is as much about catharsis as it is about record-keeping. He admits that his privacy once shielded him from scrutiny but also kept him trapped in silence about his struggles. Now, at 69, he frames his story differently: beginning with a near-death overdose, ending with cancer remission, and filling the middle with unvarnished honesty.
“I went through some difficult times,” he said, “but now I feel so much better.”
Björn Borg’s memoir offers not just the tale of a tennis great, but a portrait of a man forced to confront addiction, shame, and mortality, and who, at last, seems at peace.
Health Warning For Vitamin D Users: These 4 Symptoms Are A Red Flag

Credits: AI Generated
The NHS is urging millions of people across the UK to take vitamin D to support overall health, but experts say certain symptoms should not be ignored. In a post shared on X, an NHS spokesperson said: “From October to March we can’t make enough vitamin D from sunlight, so to keep bones and muscles healthy, it’s best to take a daily 10 microgram supplement of vitamin D. You can get vitamin D from most pharmacies and retailers.”
While health professionals agree that vitamin D supplementation is important for many people, especially during the colder months, they stress that it should be taken carefully.
Why Does Sunlight Matter For Vitamin D Production?
Sunlight plays a crucial role in how the body makes vitamin D. UVB rays trigger a reaction in the skin that converts a compound called 7-dehydrocholesterol into vitamin D3. This form of vitamin D is essential for absorbing calcium, maintaining strong bones, and supporting the immune system.
As sunlight in the UK is not strong enough between autumn and early spring, the government advises everyone to consider taking a daily supplement of 10 micrograms, or 400 IU. Relying on food alone is often not enough to meet daily needs during this period.
Expert Warns Too Much Vitamin D Can Backfire
Biomedical scientist Tobias Mapulanga, who co-founded Repose Healthcare, has warned that some people may be taking more vitamin D than their bodies can handle. He explained that as winter advice circulates, many people add tablets, sprays, or gummies without realising they are doubling up.
He said that symptoms such as constant thirst, needing the toilet more often, nausea, stomach discomfort or constipation, headaches, mental fog, and new aches or cramps can appear soon after increasing vitamin D intake. These signs are often mistaken for winter illnesses, when they may actually point to excess supplementation.
“The message is simple,” he added. “The right dose helps, but taking too much can leave you feeling worse, not better.”
High-Dose Supplements Raise Safety Concerns
Research shows that 42% of UK adults reported taking vitamin D supplements in the past year. However, an investigation by Which? found some vitamin D products on sale contained doses as high as 12.5 times the recommended safe upper limit.
NHS England also logged 42 incidents over a two-year period where high-strength vitamin D was given more often than intended. Some of these cases led to hospital treatment for hypercalcaemia, a condition caused by too much calcium in the blood, according to reports from Bristol Live.
Stop Taking Vitamin D If You Notice These Warning Signs
1. Ongoing thirst and frequent trips to the toilet
If you suddenly feel unusually thirsty or find yourself urinating more often after starting vitamin D, it may be a sign you’re overdoing it. Cut back to a single 10 microgram tablet and stop using any additional vitamin D products if this happens.
Too much vitamin D can disrupt fluid and salt balance in the body, leaving you dehydrated and running to the bathroom. Check labels carefully and remove multivitamins, sprays, gummies, and fortified foods or drinks that also contain vitamin D.
Keep water close by and sip regularly while your body settles. Stay well below the upper limit of 100 micrograms, keep just one product visible, and put the rest out of sight to avoid accidental doubling.
2. Nausea, excessive burping, or stomach discomfort
Feeling sick, bloated, or dealing with an upset stomach after taking vitamin D suggests it isn’t agreeing with you. Try taking your supplement with a full meal and switch from sprays or gummies to a plain D3 tablet if symptoms persist.
Food helps protect the stomach lining, while sprays and gummies often contain sweeteners or flavourings that can irritate digestion. Choose a simple cholecalciferol tablet with minimal ingredients and reduce the dose to 10 micrograms.
Avoid fortified shakes or energy drinks until your stomach feels normal again.
3. New muscle cramps or bone aches
If you notice more aches in your bones or frequent muscle cramps after starting vitamin D, take it as a signal to reassess. Lower your dose and focus on staying well hydrated while eating mineral-rich foods.
Excess vitamin D can interfere with mineral balance, which muscles rely on, and dehydration can make cramping worse. Drink water with meals and include yoghurt, leafy greens, beans, and bananas in your diet.
Gentle stretching and short walks can ease stiffness. Stick to one 10 microgram supplement and avoid adding anything else until symptoms improve.
4. Brain fog or headaches
Trouble concentrating or recurring headaches can be signs that your vitamin D intake is too high. Replace multivitamins or high-strength products with a single 10 microgram D3 tablet.
High doses can raise calcium levels, and extra additives found in combined supplements may affect clarity of thought. Choose a product that contains only cholecalciferol and basic fillers.
Take it with food at the same time each day for consistency and better digestion. Avoid combined vitamin A and D products and focus on one simple supplement.
To prevent accidental overuse, review everything you take that contains vitamin D. Spread out all tablets, sprays, gummies, and fortified foods, and read each label carefully. Convert IU to micrograms by dividing by 40 to make totals easier to track.
Discard any extras and stick to one daily 10 microgram source. Keep a note of symptoms such as thirst, frequent urination, stomach upset, cramps, or mental fog to see how they relate to your intake.
If You Take Omeprazole Or Metformin, This Common Deficiency Could Be Affecting You

Credits: Canva
A pharmacist has warned that people taking certain long-term medications should stay alert to subtle symptoms such as numbness, tingling, and an unusually red or sore tongue. According to Superdrug Pharmacy Superintendent Niamh McMillan, as per Mirror, the signs are often easy to dismiss and may quietly develop over time in people with low vitamin B12 levels.
Pharmacist Warns Certain Medicines May Trigger Overlooked Vitamin B12 Symptoms
McMillan explained that vitamin B12 plays a vital role in keeping nerves and blood cells healthy. A shortage can build up slowly, which means early symptoms are often brushed aside or mistaken for everyday fatigue.
She said common warning signs include persistent tiredness or weakness, breathlessness, headaches, dizziness, pale skin, and a sore or red tongue. Some people may also notice pins and needles or numbness in their hands or feet, memory lapses, trouble focusing, or changes in mood such as feeling low or unusually irritable.
Who Is Most At Risk Of Low B12 Levels?
Vitamin B12 deficiency occurs when the body either does not get enough of the vitamin from food or struggles to absorb it properly. McMillan noted that people following vegetarian or vegan diets are at higher risk, as B12 is naturally found mainly in animal products.
Older adults are also more vulnerable, as are people with digestive conditions such as coeliac disease or Crohn’s disease. In addition, those taking certain medications may be affected, particularly long-term acid-reducing drugs such as proton pump inhibitors or diabetes medication like metformin.
Dietary Sources That Help Maintain B12 Levels
To reduce the risk of deficiency, McMillan advised including reliable dietary sources of vitamin B12 wherever possible. Foods naturally rich in the vitamin include meat, fish, eggs, milk, cheese, and yoghurt.
For people who avoid animal products, fortified foods such as some breakfast cereals and plant-based milks can help support intake. In some cases, supplements may also be useful, especially when diet alone is not enough or absorption is impaired.
When To Seek Medical Advice?
McMillan stressed that anyone experiencing symptoms or falling into a higher-risk group should speak to a healthcare professional. A simple blood test can measure B12 levels, and early treatment can help prevent lasting nerve damage or other complications.
She added that Superdrug Health Clinics offer a Vitamin B12 Injection Service at selected UK locations, following clinical assessment or confirmation of deficiency.
How Medications Can Interfere With Vitamin B12?
Several commonly prescribed medications can affect how the body absorbs or uses vitamin B12. This often happens because the drugs alter conditions in the stomach or gut, making it harder for B12 to be released from food or absorbed into the bloodstream.
Medications Linked to Vitamin B12 Deficiency
The most frequently associated medications include:
- Proton Pump Inhibitors (PPIs): such as omeprazole, esomeprazole, and lansoprazole
- H2 Blockers: including famotidine and cimetidine
- Metformin
- Oral contraceptives, although experts continue to debate whether these cause a true deficiency
- Colchicine, used to treat gout and known to damage the intestinal lining
- Anticonvulsants, including drugs like phenytoin and phenobarbital, which can affect B-vitamin metabolism
- Nitrous oxide, commonly known as laughing gas, which can rapidly inactivate existing B12 in the body
- Antibiotics, particularly long-term use of chloramphenicol or neomycin, which can disrupt gut bacteria involved in B12 processing
What To Do If You Take These Medications Long Term?
Experts advise people on these medicines not to stop treatment without medical guidance. Instead, they recommend staying alert for symptoms such as fatigue, tingling or numbness in the hands or feet, brain fog, or a sore, red tongue.
Getting tested is also key. A straightforward blood test can confirm B12 levels, and many doctors now suggest regular screening for patients who take metformin or proton pump inhibitors over extended periods.
Ending Alzheimer’s Could Start With Fruit Flies, UK Scientists Suggest

Credits: Canva
UK researchers say fruit flies could help unlock why devastating brain and nerve conditions such as Alzheimer’s, Parkinson’s and motor neurone disease develop, despite decades of medical research. Scientists have known for years that many neurodegenerative disorders are linked to genetic mutations. What has remained unclear is how those mutations actually trigger disease inside the nervous system.
According to the Mirror, new findings published in the journal Current Biology suggest a breakthrough may lie in studying fruit flies, insects whose genes behave in strikingly similar ways to those in humans.
UK Scientists Say Fruit Flies May Hold Answers to Neurodegenerative Diseases
The study was led by Professor Andreas Prokop from the University of Manchester, who examined the role of so-called motor proteins using fruit flies as a model. These proteins are responsible for transporting materials inside nerve cells. Fruit flies are widely used in genetic research because experiments can be carried out quickly and at low cost while still offering insights relevant to human biology.
Professor Prokop explained that many human genes linked to neurodegenerative disease have close equivalents in fruit flies, performing nearly identical roles in nerve cells.
Axons and the Role of Motor Proteins
The research focused on axons, the long and fragile nerve fibres that act like cables, carrying messages between the brain and the rest of the body to control movement and behaviour. For axons to stay healthy, motor proteins must move essential materials along internal tracks called microtubules.
These motor proteins are vulnerable to genetic mutations, which can interfere with their function and ultimately cause axons to break down.
Why Different Mutations Cause Similar Damage
Professor Prokop said scientists have long struggled to explain why both disabling mutations, which reduce motor protein activity, and hyperactivating mutations, which keep them constantly switched on, can result in very similar forms of neurodegeneration.
To investigate this puzzle, his team studied fruit flies carrying different types of motor protein mutations.
What Happens Inside Damaged Nerve Fibres?
The researchers found that both disabling and hyperactivating mutations lead to the same physical damage inside axons. Healthy microtubules, which normally form straight bundles, begin to decay and curl into disorganised structures. Professor Prokop compared this change to the difference between dry spaghetti and overcooked spaghetti. This curling is a clear sign that axons are breaking down.
Transport, Damage and Repair Inside Axons
Axons rely on a complex internal system to survive over time. Materials must be transported from the nerve cell body to distant parts of the axon, a process carried out by motor proteins moving along microtubules.
Professor Prokop explained that if mutations prevent motor proteins from transporting cargo, axons begin to decay. Many inherited neurodegenerative diseases can be traced back to this failure. However, the study also showed that hyperactivating mutations cause a different but equally damaging problem.
Why Too Much Activity Can Be Harmful?
When motor proteins are constantly active and unable to pause, they generate excessive wear and tear along microtubules. Even under normal conditions, transport damages microtubules over time, much like traffic creates potholes on roads. This damage usually triggers repair and replacement mechanisms inside the cell.
The researchers found that when motor proteins are either overactive or when repair systems fail, the balance between damage and repair breaks down. The result is microtubule curling and axon decay.
The Role of Oxidative Stress
At first glance, disabling mutations might seem less harmful because fewer motor proteins mean less internal traffic and therefore less damage. However, the researchers discovered the opposite effect.
Reduced transport means vital supplies fail to reach the axonal machinery. This shortage triggers oxidative stress, a harmful condition linked to cell damage. Oxidative stress, the team showed, disrupts microtubule maintenance and leads to the same curling seen with hyperactive motor proteins.
Based on these findings, Professor Prokop and his team proposed what they call the dependency cycle of axon homeostasis. This model suggests that axon maintenance depends on motor proteins and microtubules, but those same systems rely on ongoing transport to function properly.
If mutations interfere with this balance, either by causing oxidative stress or by upsetting the repair process, the entire cycle collapses.
Professor Prokop said parallel research from his group strongly supports this model. He added that because the genetic foundations of fruit flies and humans are surprisingly alike, it is highly likely that the same mechanisms operate in people. According to Professor Prokop, there are already strong signs that these findings apply beyond fruit flies and could reshape how scientists understand and eventually treat neurodegenerative disease.
© 2024 Bennett, Coleman & Company Limited

