- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Bubonic Plague Changed The Human Immune System, Here's How
Credits: Canva
After the California bubonic plague case, where a resident who went camping at South Lake Tahoe area tested positive for plague, lot has been talked about the disease. The bubonic plague is often remembered as one of the deadliest pandemics in human history.
Today, with the California resident case, we all know that it still lingers in scattered regions, but antibiotics make it far less threatening.
What is less widely known is that the plague may have permanently altered human biology, leaving an imprint on the immune system that persists even now.
Also Read: Bubonic Plague California Resident: Here's All That You Need To Know About The Disease
The Bacterium Behind the Plague
The plague is caused by Yersinia pestis, a rod-shaped bacterium carried by fleas that thrive on rodents and other wild animals. While unremarkable in appearance under a microscope, this microbe has shaped centuries of human history. At its peak during the 14th century, the Black Death killed tens of millions across Europe, with entire towns and communities wiped out in a matter of months.
Earlier outbreaks of plague are believed to stretch back thousands of years, with traces of the bacterium found in ancient human remains. Yet the medieval Black Death was unlike anything before, spreading rapidly through trade routes and devastating Europe within a few short years.
Natural Selection in the Wake of the Black Death
The scale of mortality during plague outbreaks raised an intriguing question: could survival have been influenced by genetics?
If certain individuals carried genetic variations that helped them fight off the infection, those traits might have been passed on to their descendants. In essence, the plague may have acted as a brutal filter, altering the genetic makeup of future generations.
Modern genetic studies now provide evidence for this idea. By comparing DNA from plague victims with that of later populations, researchers have observed that people who lived through the plague era and passed on their genes tended to carry variants that supported stronger immune defenses. This suggests that the catastrophe of the Black Death created a surge of natural selection across affected regions.
Unlocking Clues from Ancient Bones
For a long time, studying the genetic impact of plague was extremely difficult. DNA preserved in centuries-old skeletons is often degraded and contaminated by soil and microbes. However, advances in ancient DNA sequencing opened new doors.
Scientists discovered that the inner ear’s bony labyrinth, one of the densest parts of the human body, preserves intact DNA remarkably well. Extracting genetic material from this area has allowed researchers to examine how plague survivors may have differed from those who succumbed.
With these methods, mass graves of plague victims have become key resources for understanding how the disease influenced human biology. By sequencing genomes from skeletons buried before, during, and after outbreaks, scientists can track changes across generations.
The Role of HLA Genes
One of the clearest examples of plague-driven selection lies in the human leukocyte antigen (HLA) system. This group of genes is essential for immune defense, helping the body recognize and destroy cells infected by pathogens. Even subtle differences in HLA variants can determine whether someone is more resilient against a particular disease.
Evidence suggests that during the plague years, people carrying certain HLA variants were more likely to survive. These protective versions of the genes became more common in descendants over time. This mirrors what scientists have observed in more recent pandemics, such as Covid-19, where some people showed natural resistance thanks to genetic variations in immune-regulating genes.
A Gene Called ERAP2
Another key discovery centers on a gene known as ERAP2. This gene produces a protein that helps immune cells break down foreign invaders, including bacteria like Yersinia pestis. Researchers studying remains from plague cemeteries in London and Denmark found that individuals who carried a particular version of ERAP2 were twice as likely to survive the Black Death.
By the end of the 14th century, this protective variant had become widespread among Europeans, appearing in roughly half the population in London and even more frequently in Denmark. It is one of the strongest pieces of evidence showing how a pandemic can reshape human genetics in just a few generations.
Balancing Benefits and Risks
However, the story is not entirely one of benefit. Genes that protect against deadly infections may also carry hidden costs.
For example, some of the same immune-system variations that helped ancestors survive plague outbreaks are now associated with autoimmune disorders, where the immune system mistakenly attacks healthy tissue. This illustrates the trade-offs of evolution: what once ensured survival may create vulnerabilities in a very different modern environment.
Why More Research is Needed
While the genetic evidence is compelling, scientists caution that we are only beginning to understand the full scope of plague’s impact. To get a clearer picture, thousands more ancient genomes from across Europe and Asia need to be analyzed. Only then can researchers determine how widespread these adaptive changes really became.
There is also debate over whether plague was the most significant driver of immune evolution. Diseases like smallpox, which persisted for centuries and claimed hundreds of millions of lives, may have exerted an even greater influence. The challenge is teasing apart the effects of different pathogens across different time periods.
What To Remember
You May Like To Read: What History Teaches Us About Plague? Are There More Than One Type?
Despite its reputation as a medieval killer, plague has not disappeared. Small numbers of cases are still reported each year in parts of the world, from the western United States to Madagascar. Thanks to antibiotics, survival rates are far higher today, but the fact that the disease persists is a reminder of its enduring presence in nature.
Rodents and fleas continue to serve as reservoirs for Yersinia pestis. Outbreaks in isolated communities highlight the delicate balance between human society and the microbial world. While the scale of devastation seen during the Black Death is unlikely to return, the evolutionary lessons it left behind remain relevant.
Centuries later, the legacy of plague survives in our DNA. Some of the same genetic defenses that once meant the difference between life and death still influence how our immune systems function today.
Wearing Contact Lenses This Monsoon? Here Is What Eye Doctors Want You to Know

Credits: Canva
Monsoons are more than just good, hot food. And while most of us are quick to pull out umbrellas and raincoats, very few think about protecting our eyes, especially if we wear contact lenses. And according to eye specialists, this oversight could cost us more than just a little irritation.
Why Your Eyes Are at Risk in the Rainy Season
The humid climate during the rainy season creates the perfect environment for viruses to thrive. On top of that, people tend to spend more time indoors and in close contact with one another, which raises the risk of viral infections spreading by nearly 50 per cent. Add to this the common flu, which weakens immunity, and your eyes become more vulnerable than ever.
Contaminated water is another culprit. Dr Jayapratha Selvaraj, General Ophthalmology, points out that poor water hygiene can worsen eye conditions such as conjunctivitis (commonly known as pink eye) and keratitis, an infection of the cornea. “These infections are especially troublesome for people who wear contact lenses,” she says.
Dr Venkatesan C, Senior Consultant – Ophthalmology, agrees, adding that fungal and bacterial keratitis become more common during the monsoon. “They may start with redness, irritation, or pain, but if not treated right away, they can cause serious visual problems,” he warns.
Contact Lens and Monsoon
Contact lenses are a blessing for millions, particularly students and professionals who find glasses cumbersome. But during the monsoon, they can turn into little traps for germs.
“Contact lenses are safe if you follow the rules. But the moment hygiene slips, lenses can let bacteria or fungi stick to the eye’s surface,” says Dr Venkatesan. The moist, humid environment during the rainy season accelerates this risk. Tears dry more slowly in such weather, keeping the surface of the eye damp, a perfect breeding ground for infections.
Students, in particular, face greater danger. Many wear their lenses for long hours, share lens solutions with friends, or even swim in pools or rainwater while keeping their lenses on. Each of these habits, says Dr Venkatesan, can drastically raise the risk of infection.
Golden Rules of Lens Care in the Rainy Season
You do not have to abandon your lenses every time it rains. With the right care, you can enjoy both the rain and clear vision.
Dr Selvaraj lists the basics:
- Wash your hands thoroughly before touching or wearing lenses.
- Store lenses only in their designated case.
- Never use expired lenses.
- Avoid rinsing or storing lenses in tap water or saline; always use proper lens solution.
- Do not sleep, bath, or swim with lenses on.
Dr Venkatesan adds a few more monsoon must-dos:
- Always use fresh lens solution; never top up old liquid in the case.
- Take off your lenses before going out in the rain.
- If your doctor has not recommended it, do not sleep in your lenses.
- If you notice persistent redness, discharge, or blurred vision, remove your lenses immediately and see an eye doctor.
When Infections Happen
Despite best efforts, sometimes you still get infections. Viral conjunctivitis, for example, often resolves on its own, but that does not mean you should ignore it. “Ophthalmologists may prescribe antibiotic and lubricant eye drops to reduce discomfort and prevent spread,” explains Dr Selvaraj.
If the cornea gets involved, as in keratoconjunctivitis, timely medical treatment becomes crucial. Viral eye infections can remain contagious for up to two weeks, so doctors urge patients to:
- Wash hands frequently.
- Avoid sharing towels, bed sheets, or handkerchiefs.
- Resist rubbing or touching the eyes.
- Switch to glasses and only return to contact lenses after medical clearance.
You do not have to give up your lenses during monsoon, but you do have to respect the hygiene rules. Even a small slip-up, like rinsing lenses in tap water or wearing them during a sudden downpour, can lead to painful infections and, in some cases, long-term vision loss.
As Dr Venkatesan puts it, “You may enjoy the beauty of the rainy season without hurting your eyes if you take basic steps and get medical care right away.”
This Contact Lens Health Week 2025, know that your eyes deserve as much protection as your clothes and shoes. And when it comes to contact lenses in the monsoon, a little extra care goes a very long way.
Dr Jayapratha Selvaraj is an ophthalmologist at Dr Agarwal's Eye Hospital, Chennai
Dr Venkatesan C is a senior ophthalmology consultant at SRM Global Hospitals, Chennai
Do You Drink Coffee Too Hot? It Could Increase Cancer Risk By 6 Times

(Credit - Canva)
Drinking a hot cup of coffee on a winter morning or chilly evening is one of the best feelings one in the world. However, did you know this habit could lead to you risking your health?
A new study suggests that drinking very hot tea or coffee often might increase your risk of a type of throat cancer known as oesophageal squamous cell carcinoma (ESCC). Researchers looked at the habits of over 450,000 people in the UK. They found that those who drank eight or more cups of "very hot" drinks a day were almost six times more likely to get this cancer over a 12-year period.
A "very hot" drink was defined as being hotter than 149°F (65°C). The study also found that the more hot drinks a person had, the higher their risk. For example, drinking four to six cups a day raised the risk by almost four times, and six to eight cups raised it by nearly five times.
Do Hot Drinks Lead To Cancer?
Although scientists don't know the exact reason, they think that drinking very hot liquids over and over might damage the cells in your throat. This constant damage could eventually lead to cancer.
In a study with animals, drinking very hot water (158°F or 70°C) actually helped tumors grow in rats. A separate study in Iran also found that people who drank tea hotter than 140°F (60°C) had a higher risk of throat cancer.
Experts from Cancer Research UK noted that 60°C is "a lot hotter than most cups of tea." They added that if you let your tea cool for a few minutes or add cold milk, you are likely not to increase your risk of cancer. The key takeaway is to avoid drinking beverages at extremely high temperatures.
Do Hot Drinks Harm Our Health?
According to Memorial Sloan Kettering Cancer Center, the idea that very hot drinks like coffee or tea could cause cancer has been around for a long time. The theory is that the heat could damage the lining of your throat, and over time, this damage could lead to cancer. While some animal studies have shown a link, this was at temperatures much hotter than what people would normally drink.
More recently, some studies from other countries have linked hot drinks to a type of throat cancer, but the evidence isn't very strong, especially for people in the U.S. and Europe. They explained how a study from China also found a higher risk of throat cancer in people who drank very hot tea, but these people were also heavy smokers or drinkers. This makes it difficult to say that the hot tea alone was the cause.
Do Hot Drinks Cause Cancer?
While many researchers have pointed that out there is a link, there are many crucial factors missing. Experts explain that these studies are misleading for several reasons:
- The type of cancer linked to hot drinks (squamous cell carcinoma) is much less common in the U.S. than other types.
- The study participants often had other risk factors, like smoking, drinking alcohol, or living with environmental issues. This makes it hard to be sure if the hot tea was the real problem.
- The China study wasn't very scientific; it just asked people to guess how hot their tea was.
- Even the study from Iran, which actually measured the temperature, had a problem because almost everyone in that region drinks hot tea, so there was no good group to compare them to.
- Healthcare professionals explain that there is no solid evidence that drinking hot liquids by themselves increases your risk of cancer. At most, it might add to the risk if you also smoke or drink alcohol.
Australian Scientists Grow World’s First Lab-made Human Skin With Blood Supply
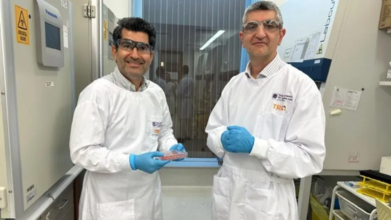
Photo: X
In a groundbreaking achievement, a team of Australian scientists has successfully grown the world’s first fully functioning lab-made human skin that comes with its own blood supply. This breakthrough, developed at the University of Queensland, could transform how we treat burns, skin grafts, and chronic skin diseases.
A Skin Model That Mimics Real Human Skin
The team, led by researchers at UQ’s Frazer Institute, used stem cells to create a replica of human skin that is almost indistinguishable from natural skin. This lab-grown model includes blood vessels, capillaries, hair follicles, nerves, different tissue layers, and even immune cells.
“This is the most life-like skin model developed anywhere in the world. It will allow us to study diseases and test treatments far more accurately,” explained lead researcher Dr. Abbas Shafiee, a tissue engineering and regenerative medicine scientist.
Until now, scientists were restricted in how closely they could study skin disorders and design therapies. With this new model, those barriers have been lifted.
Also Read: Japan Races To Develop World’s First Artificial Blood, Trials To Begin
How Scientists Built It
The process behind this innovation is as fascinating as the outcome. The team started by taking human skin cells and reprogramming them into stem cells. Stem cells are unique because they have the ability to transform into any type of cell in the body.
Once prepared, these stem cells were placed into petri dishes where they grew into miniature versions of skin, known as skin organoids. To make the skin more life-like, the researchers used the same stem cells to create tiny blood vessels. These were integrated into the organoids, enabling the skin to develop in a way that mirrored natural growth.
“It developed just like natural human skin, with layers, follicles, pigmentation, appendages, nerves, and most importantly, its own blood supply,” said Dr. Shafiee. The findings were recently published in the journal Wiley Advanced Healthcare Materials.
Six Years in the Making
The breakthrough did not happen overnight. The lab-grown skin model is the result of six years of research and testing. The development demonstrates how far regenerative medicine has come, particularly in the field of stem cell science.
By creating skin with its own blood supply, researchers believe they can take skin engineering to a whole new level. Previous skin models lacked this crucial feature, limiting how effective they were for research or medical use.
Potential for Treating Skin Diseases
Co-author Professor Kiarash Khosrotehrani from the Frazer Institute highlighted how this achievement could change treatment options for people with chronic skin conditions. “Skin disorders can be difficult to treat, and it’s a real breakthrough to provide hope for people living with these challenges,” he said.
The model may be especially useful for studying and developing treatments for inflammatory and genetic skin conditions such as psoriasis, atopic dermatitis, and scleroderma. It could also lead to more effective skin grafts for burn victims and people with severe injuries.
© 2024 Bennett, Coleman & Company Limited

