- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Can A Rash Be A Sign Of COVID-19? Here’s Everything You Should Know

Credits: canva
When COVID-19 first emerged, it was largely seen as a respiratory illness. Over time, doctors discovered that the virus can affect nearly every major organ, including the heart, kidneys, liver, and skin. While cough, fever, and fatigue remain common signs, some people also develop unusual skin reactions. So, can COVID-19 actually lead to rashes? Here’s what experts have found.
Can COVID-19 Really Cause Rashes?
When COVID-19 first emerged, it was largely seen as a respiratory illness. Over time, doctors discovered that the virus can affect nearly every major organ, including the heart, kidneys, liver, and skin. While cough, fever, and fatigue remain common signs, some people also develop unusual skin reactions. So, can COVID-19 actually lead to rashes? Here’s what experts have found.
What Do COVID-19 Rashes Look Like?
Skin changes linked to COVID-19 are not among the most common symptoms, but they do occur. These rashes may appear on the neck, mouth, or toes and are often caused by inflammation in the body, as per Health website. They can look like flat or raised patches, small round spots, or itchy bumps. In some people, these rashes appear while they’re infected; in others, they show up weeks later.
Why Do These Rashes Occur?
Researchers believe COVID-related rashes are connected to how the virus interacts with the body’s ACE2 receptors, which are found in the skin. When the virus attaches to these receptors, it can trigger the release of inflammatory proteins called cytokines. This inflammation may lead to skin irritation, itchiness, or lesions.
Common Types of COVID-19 Rashes
1. COVID Toes
One of the most recognized skin signs of the virus, “COVID toes,” resembles chilblains, which are cold-weather sores. They appear as pink, red, or purple patches, sometimes with swelling or blistering. This condition is seen more often in younger people and may occur even after other symptoms fade.
2. Hives (Urticaria)
Hives tend to appear suddenly and can spread across any part of the body. They’re itchy, raised, and may come and go within hours or days.
3. Neck Eczema
Some people develop eczema-like rashes on the neck, chest, or trunk during or after COVID-19. The patches can be itchy and vary in color depending on skin tone—pink on lighter skin and brown, gray, or purple on darker skin.
4. Oral Rash
COVID can also cause soreness or peeling inside the mouth or on the lips. The area may feel dry, irritated, or scaly as it heals.
5. Vesicular and Papular Rash
These small, itchy bumps can be filled with fluid (vesicular) or solid (papular). They may appear anywhere on the body and are often linked with ongoing inflammation.
6. Pityriasis Rosea
This condition begins with a single large patch on the chest, back, or abdomen, followed by smaller spots that form a tree-like pattern. Though harmless, it can take several weeks or months to fade.
7. Purpuric or Vasculitic Rash
These rashes appear as dark, bruise-like spots caused by small blood vessel damage under the skin. The color may range from red and purple to brown or black, depending on skin tone.
How Long Do COVID Rashes Last?
The duration depends on the type of rash and the person’s immune response. Most clear up within 2 to 12 days, but some, especially in long COVID cases, may persist for weeks.
How Are COVID Rashes Treated?
Many rashes resolve without any special treatment. To relieve itching or pain, applying mild hydrocortisone cream can help. For more severe or persistent cases, doctors may recommend:
- Antihistamines to reduce itching
- Corticosteroids to lower inflammation
- Blood thinners if the rash is linked to blood vessel irritation
Your doctor will determine the safest treatment depending on the type of rash and overall health.
Disclaimer: This article is for general informational purposes only and should not be considered medical advice. Always consult a qualified healthcare professional before starting, stopping, or changing any medication, or if you experience any unusual symptoms or side effects.
Having Difficulty Concentrating? Experts Say ‘Popcorn Brain’ Might Be To Blame — All You Need To Know About This Syndrome

Credits: Gemini/Canva
Do you struggle to concentrate and find it hard to focus on one task for more than a few minutes? You might be dealing with what psychologists are calling “popcorn brain”. The name may sound lighthearted, but experts say the condition is real and growing more common.
With constant use of smartphones, laptops, tablets, and televisions, people, especially teenagers and young adults, are spending most of their waking hours in front of screens. This nonstop exposure is leading to what’s now known as Popcorn Brain Syndrome, a modern problem that is affecting focus, attention span, and emotional balance.
To understand the condition better, we spoke with Dr. Astik Joshi, Child, Adolescent, and Forensic Psychiatrist at Veda Clinic, Rohini, and Fortis Hospital, New Delhi.
What Is Popcorn Brain Syndrome?
Popcorn Brain Syndrome refers to a state where the brain becomes so used to fast, constant digital stimulation that it struggles to adjust to slower, real-world activities. Much like popcorn rapidly popping in a microwave, the brain starts craving constant bursts of new information. When the pace slows down, like during reading or in-person conversations, the mind becomes restless, impatient, or easily bored.
According to Dr. Joshi, “Popcorn brain syndrome isn’t a formal medical term or diagnosis. It’s a phrase used to describe how our minds can’t stay still and keep jumping from one thought to another, just like popcorn pops when exposed to heat.”
However, now, the term “popcorn brain” has been gaining attention in mental health circles. It was first introduced by David M. Levy, Ph.D., a computer scientist at the University of Washington, who described it as a state where people become so used to multitasking online that real life feels too slow and uninteresting.
The syndrome is not limited to social media enthusiasts or office workers glued to their emails, the constant pings and alerts from our devices make this phenomenon relatable to almost everyone.
How Does Popcorn Brain Syndrome Affect Your Brain?
Popcorn brain can cause difficulty focusing, frequent distraction, restlessness, and poor time management. Dr. Joshi explained that screen time creates a continuous flow of stimulation that makes our thoughts and emotions jump around, causing mental and emotional unease.
“This constant mental restlessness can have a negative impact on teenagers and young adults,” he said. “Their brains are still developing, and they haven’t yet built full control over their emotions and thoughts. Continuous exposure to screens interferes with healthy brain development and emotional regulation.”
According to a Healthline report, people experiencing popcorn brain also often complain of eye strain, headaches, blurred vision, and neck or shoulder pain, symptoms that overlap with computer vision syndrome (CVS) or digital eye strain.
Social Media Is to Blame for Popcorn Brain Syndrome
It is no surprise that social media plays a major role in this growing issue. Studies show that frequent use of phones, computers, and apps like Instagram can deeply affect our ability to concentrate.
One study published in Scientific Reports found that simply having a smartphone nearby reduced participants’ focus during attention tests. When their phones were switched off or placed out of sight, their concentration levels improved noticeably.
Another study by Stanford University showed that constantly shifting attention between screens—whether social media, phones, or TV, makes it harder to complete even simple tasks. In a 2022 survey conducted by King’s College London, half of adults in the U.K. admitted they felt their attention spans had shortened significantly over time.
How To Cure Popcorn Brain Syndrome?
To break the cycle of checking your phone every few minutes and give your brain a reset, Dr. Aditi Nerurkar, Harvard Physician, suggests four simple practices:
Limit your scrolling time
Restrict yourself to no more than 20 minutes twice a day for social media or non-essential phone use. “Use your phone only for calls, messages, and important emails,” she advises. To keep track, set a timer whenever you scroll.
Turn off notifications
Disable push alerts and pop-ups that tempt you to pick up your phone unnecessarily.
Keep your phone away while working.
Place your smartphone at least ten feet from your desk so you can focus on tasks. “Do the same at home, especially when you’re spending time with family,” says Dr. Nerurkar.
Don’t sleep next to your phone
Avoid placing your device on your bedside table. This prevents you from checking it right before bed or first thing in the morning. Let loved ones know to call if there’s an emergency, and keep the ringer on instead.
Dr. Nerurkar acknowledges that cutting down on screen time won’t be easy at first. To make it easier, replace the habit with small, grounding activities, like grabbing a notepad, fidget toy, or book, or simply walk around for a minute or two when you feel the urge to reach for your phone.
Listeria Pasta Outbreak: Worried About Infection? Here’s How To Stay Safe
Credits: Canva
Recalled Pasta Meals Listeria: A Listeria outbreak has taken six lives across 18 U.S. states in the past week, according to the Centers for Disease Control and Prevention (CDC). Two additional deaths have been reported in connection with a nationwide Listeria outbreak linked to recalled pasta salads and prepared meals, as noted by Emegypt.
From symptoms and affected products to safety measures, here is everything you need to know about the ongoing Listeria outbreak in the U.S. As the Listeria pasta outbreak spreads further, here’s a look at what it involves and how to prevent this potentially fatal infection.
What Is Listeria Pasta Outbreak?
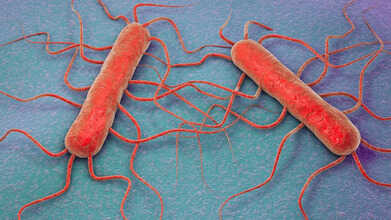
The illness stems from a foodborne bacterial infection. When the bacterium Listeria monocytogenes contaminates food and causes poisoning, it is known as a Listeria outbreak, according to the Cleveland Clinic. The CDC has confirmed 27 Listeria cases across 18 states, with 25 hospitalizations so far. The source has been traced to Listeria monocytogenes found in precooked pasta meals produced by Nate’s Fine Foods Inc.
Listeria Recalled Pasta Meals: What Is Listeria Monocytogenes?
Listeriosis is a type of food poisoning caused by the bacterium Listeria monocytogenes, often referred to simply as “Listeria.” The Cleveland Clinic notes that most people experience mild symptoms such as fever, headache, nausea, or diarrhea. However, for individuals with weakened immune systems or those over the age of 65, the infection can lead to serious or even life-threatening complications.
Pregnant women are also at high risk since the infection can pass to the baby during pregnancy or delivery, leading to miscarriage, premature birth, or severe health problems for the newborn.
Listeria Outbreak: What Foods Have Been Recalled For Listeria?
According to USA Today, the following items have been recalled due to possible Listeria contamination:
- Marketside Grilled Chicken Alfredo (32.8 oz)
- Sprouts Farmers Market Smoked Mozzarella Pasta Salad
- Giant Eagle Smoked Mozzarella Pasta Salad
- Kroger Deli Bowtie and Penne Pasta Salads
- Scott & Jon’s Shrimp Scampi with Linguini Bowls (9.6 oz)
- Trader Joe’s Cajun Style Blackened Chicken Breast Fettuccine Alfredo (16 oz)
- Albertsons Store-Made Deli Pasta Salads
- Marketside Linguine with Beef Meatballs & Marinara Sauce (12 oz)
Listeria Outbreak: How To Prevent The Deadly Infection?
The U.S. Food and Drug Administration (FDA) recommends three key steps to reduce the risk of Listeria infection:
Maintain Proper Cooling Temperatures
Keeping food cold slows the growth of Listeria. If your refrigerator doesn’t have a digital temperature display, use a thermometer to check and adjust the settings. Place another thermometer in the freezer for accuracy.
• Your refrigerator should be at 40°F (4°C) or below.
• Your freezer should be at 0°F (-18°C) or below.
Consume Ready-to-Eat Foods Promptly
The longer leftovers or ready-to-eat meals stay in the refrigerator, the greater the chance that Listeria may grow. If a food item starts to smell, taste, or look unusual, it’s best to discard it.
Keep Your Refrigerator Clean
Regular cleaning helps prevent bacteria from spreading. Wipe spills as soon as they occur, this prevents Listeria from multiplying and contaminating other items. Wash shelves and walls with hot water mixed with mild dish soap, rinse thoroughly, and dry with a clean cloth or paper towel.
What Really Happens In Your Brain During Deep Sleep

Credits: CANVA
Sleep takes up nearly one-third of a person’s life, yet many still wonder what really happens while we rest. Until the mid-20th century, scientists believed sleep was simply a time when the body and brain shut down.
Research now shows that sleep is far from passive, it’s an active, restorative process essential for mental and physical health. As Johns Hopkins neurologist and sleep expert Dr. Mark Wu explains, the brain remains deeply engaged during sleep, performing vital tasks that influence memory, mood, and overall well-being.
The Stages of Sleep
Experts say the human sleep cycle has four main stages that repeat throughout the night. The first three make up non-rapid eye movement (non-REM) sleep, while the fourth is REM sleep, the stage most closely linked with dreaming.
In the first stage of non-REM sleep, the brain and body begin to shift from wakefulness to rest. Brain activity slows, muscles relax, and it is common to experience small, sudden twitches.
During the second stage, the body’s temperature drops slightly, and breathing and heart rate slow. Brainwaves continue to decelerate, though quick bursts of activity may still appear as the brain processes and stores information.
The third stage marks deep sleep, which is the most restorative phase. Here, the body fully relaxes, and the heart rate, breathing, and brain activity reach their lowest levels. This stage is crucial for waking up feeling refreshed and for healing and repair processes throughout the body.
The final stage is REM sleep, which begins about 90 minutes after you fall asleep. It starts short, roughly 10 minutes, but lasts longer with each cycle. During REM, the eyes move rapidly beneath the eyelids, breathing quickens, and heart rate and blood pressure rise to near waking levels. This is when most dreaming occurs. Interestingly, as people age, the amount of REM sleep they experience gradually decreases.
How The Body Regulates Sleep
According to Dr. Wu, two main forces govern sleep: the circadian rhythm and the body’s sleep drive.
The circadian rhythm acts as the body’s internal clock, controlled by a cluster of brain cells that respond to light and darkness. This rhythm triggers the release of melatonin at night and halts it when morning light appears. People who are completely blind often struggle with sleep because their brains can’t register these light cues properly, as per the John Hopkins Study.
The sleep drive works much like hunger. The longer you stay awake, the stronger your urge to sleep becomes. Unlike hunger, though, your body can override your willpower, if exhaustion sets in, it can force sleep to happen, even during daily activities or while driving. In extreme fatigue, brief “microsleep” moments lasting just a few seconds can occur without a person realizing it. However, taking long naps later in the day can reduce this natural sleep pressure, making it harder to fall asleep at night.
Why Sleep Matters For Your Brain
Anyone who has felt mentally sluggish after a sleepless night knows how strongly rest affects the brain. Adequate sleep is key to brain plasticity—the ability to learn, adapt, and form memories. Without it, the brain struggles to retain new information and perform cognitive tasks. Scientists also believe that deep sleep allows the brain to clear out toxins that build up during waking hours, improving long-term brain health.
Sleep impacts far more than the mind. Poor sleep can worsen conditions like depression, high blood pressure, migraines, and even seizures. It weakens the immune system, leaving the body more vulnerable to infection. Metabolism also suffers, as just one night without enough rest can temporarily throw the body into a prediabetic state.
As Dr. Wu explains, “There are countless ways sleep supports health.” From mental clarity to physical repair, the hours we spend asleep are some of the most important for keeping the body and brain functioning at their best.
© 2024 Bennett, Coleman & Company Limited

