- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can Right To Die Be Practiced By Non-Terminally Ill Patients?

Credits: Canva
When Canada first passed its assisted dying legislation, also known as the Bill C-14 in 2016, it soon became a landmark in healthcare and personal autonomy. It is officially known as Medical Assistance in Dying (MAID) and was initially available only to those adults who were terminally ill. The eligibility criteria had strict parameters: the person had to be suffering from a "serious and incurable illness", be in an "advanced sate of irreversible decline", experience "intolerable suffering", and crucially their natural death had to be "reasonable foreseeable".
This legal threshold was also known as Track 1. This was modeled on end-of-life care and largely served people with terminal cancer or other severe illness who wanted control over their dying process. Track 1 is a relatively swift procedure, with some patients receiving MAID within a day of applying.
However, many Canadians live with severe, non-terminal conditions and they felt left out. These were people with degenerative diseases, chronic pain, or spinal injuries. They had and continued to suffer deeply, but were not imminently dying. They also began to request for MAID, however, were routinely denied.
ALSO READ: What Are The Dutch Guidelines Of Active Euthanasia And The Countries That Allow It
This led to a legal challenge by Jean Truchon, reports The New York Times. He is a man with spastic cerebral palsy whose suffering wasn’t deemed terminal. In 2019, a Quebec court ruled that the “reasonably foreseeable death” clause was unconstitutional. This case prompted the introduction of Bill C-7 in 2021, which created Track 2 — extending MAID eligibility to people with serious, incurable conditions causing enduring suffering, even if their deaths weren’t foreseeable.
Track 2 includes additional safeguards: a 90-day assessment period, evaluation by two independent clinicians, and consultation with specialists if necessary. Applicants must also be informed of other ways to alleviate their suffering and show they’ve seriously considered those options. While mental illness alone was technically included under Track 2, implementation has been delayed until 2027 due to concerns about inadequate mental health infrastructure.
Despite its tighter process and ethical complexities, Track 2 MAID has steadily gained use. In 2023, there were 622 deaths under Track 2 compared to 14,721 under Track 1. Still, Track 2 has ignited national debate, with critics claiming it opens the door to premature death among vulnerable populations — and supporters defending it as a compassionate choice for those trapped in non-terminal agony.
Also Read: First Sign Of Diabetes Might Show Up In Your Eyes—Here’s What To Look For
Paula Ritchie And The Doctor Who Stepped Forward To Assess Track 2 Patients
A 52-year-old woman from Smith Falls, Ontario had a far from simple case, assessed by Dr Matt Wonnacott, who agreed to assess Track 2 patients. He believed that these patients too had the right to autonomy and must be able to guide care decision, including the right to choose death when suffering becomes unbearable, reports The New York Times.
Paula had a long history of chronic pain and mental health challenges: fibromyalgia, chronic fatigue syndrome, migraines, depression, PTSD, borderline personality disorder, and more. But things got worse in early 2023 after a head injury. She began experiencing vertigo, migraines, uncontrollable muscle movements, and an overwhelming dizziness that made even basic tasks impossible.
Doctors failed to find a physical cause. Some attributed her symptoms to psychological distress, while others diagnosed post-concussion syndrome. Treatments ranged from Percocet and Ativan to acupuncture and reiki, but nothing worked. Paula’s life shrank to a single room, her body wracked with pain, her mind spinning. She tried to end her life — and failed.
YOU MAY WANT TO READ: Plea of Chilean Woman With Muscular Dystrophy Sparks National Debate on Euthanasia Bill
Frustrated by her inability to access help or relief, Paula began pursuing MAID. Her first request was denied. But she persisted, calling the regional MAID coordination center daily until she was finally reassessed by Wonnacott and a psychiatrist, Dr. Elspeth MacEwan.
During the assessment, Wonnacott asked if she would wait five years for a hypothetical cure. Paula said no — she could barely get through a day. She felt tortured. A veterinarian, she told a friend, would euthanize a dog in better shape.
Importantly, Wonnacott found her reasoning sound. She was not acting out of untreated mental illness or impulsivity. She had sought treatment. She had given it time. And she had thought carefully about her request. MacEwan agreed. Paula met the criteria under Track 2.
Fingernail Colour Changes Can Reveal Underlying Disease: What Each Shade May Indicate

Credits: AI Generated
Experts have urged people to keep an eye on their fingernails, as unusual changes might point to underlying health problems. According to specialists, certain nail colours could indicate the risk of severe illnesses. While some changes may be harmless, specific colour alterations could require medical attention. The American Academy of Dermatology Association (AAD) has outlined concerning nail symptoms on its website.
The organisation stated: "Have you noticed a change to any of your nails lately? A change in colour, texture, or shape can be harmless, but it can also be a sign of disease. If you notice any of the following changes to a fingernail or toenail, it's time to see a board-certified dermatologist."
Fingernails Colour Change: What Changes Could Signal Serious Health Conditions
Based on this advice, AAD specialists recommend watching for these nail colours:
- White
- Half pink, half white
- Yellow
- Dusky red half-moons
- A dark streak
They explained: "Nail colour changes can sometimes reflect conditions inside the body. Certain shades may serve as warning signs for specific diseases."
White Nails: Could Indicate Liver Problems or Diabetes
The AAD points out that nails turning white may be a sign of liver disease or diabetes. In liver disease, this is particularly likely in people with cirrhosis, the most advanced stage of the condition.
However, nails can naturally become whiter with age. Still, it is recommended to have any noticeable changes checked by a healthcare professional.
Half Pink, Half White Nails: Possible Sign of Kidney Disease
Nails that appear half pink and half white may indicate kidney problems. The AAD describes this pattern as “a white colour on the upper part of one or more nails and a normal to reddish-brown colour below.”
Yellow Nails: Could Signal Lung or Circulatory Issues
Yellowing of the nails may be linked to lung disease and could reflect problems in the circulatory or lymphatic systems.
"When these systems don’t function properly, fluid can accumulate in the soft tissues beneath the skin, causing nails to turn yellow," explains the Cleveland Clinic. That said, yellow nails can also result from fungal infections or smoking.
Dusky Red Half-Moons: Potential Early Sign of Cancer
The AAD warns that a new or changing dark streak under a nail could indicate cancer, particularly melanoma, which is the most dangerous form of skin cancer. The NHS also advises seeing a GP if “you have a dark area under a nail that has not been caused by an injury.”
Dark Patches Under the Nails: When to Seek Immediate Care
Noticing a dark patch beneath your nail may point to skin cancer. Experts recommend visiting a GP as soon as possible if this occurs.
Other Nail Colours To Watch
Additional nail colours that may indicate health issues, according to the AAD, include:
- Blue nails: Could indicate insufficient oxygen in the blood.
- Pale nails: Might point to anaemia.
- Blue half-moons: Could suggest exposure to toxins or poisoning.
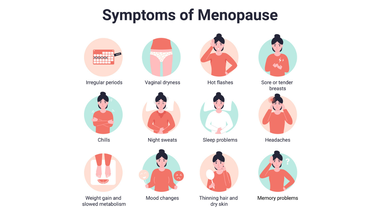
Perimenopause Isn’t Just Hot Flashes, Doctors Explain the Lesser-Known Signs

Credits: iStock
Many in their late 30s and early 40s find themselves Googling weird stuff, including 'why am I having a tingling feelin in my arm?' 'why do I feel like something is brushing across my arm?', and more. This is what many call a phantom feeling arm, which means there is nothing actually tickling, but you feel it anyway. Medically, it is known as paresthesia, a tingling feeling or numb sensation, usually what people refer to as the pins and needles sensation. This is caused by temporary pressure on a nerve or any underlying nerve damage issue.
If you look up anything like that, many women claimed, it instantly shows: perimenopause.
Despite an increased awareness around it, perimenopause and menopause still remain a taboo. In a survey, it was found that 54 per cent of women were concerned about the uncertainty they are about to face in their perimenopause and menopause period.
Menopause is not just hot flashes, it is much more than that. Dr Mahima Gulati, an endocrinologist at UConn Health points out symptoms like gaining weight despite "doing everything right", brain fog, aching joints, sleepless nights, exhausting days, and depleted energy. She says "These symptoms are real. This is not something women are imagining, and it is not just aging. There are real biological changes happening, and women deserve evidence based care and support as they move through them."
What Can Help Women Dealing With Menopause and Perimenopause?
Before going into the solution, let us first understand what these term really mean.
Perimenopause: It is the period when a menstruator transitions to menopause, or when the period stops permanently. This phase is characterized by fluctuating hormone levels, irregular periods, which could be shorter, longer, heavier, or lighter, hot flashes, sleep problems and mood changes.
Menopause: This is the natural, permanent end of menstruation defined as 12 consecutive months without a period. This typically occurs between ages 45 to 55.
What Can Help In Menopause And Perimenopause?
Form Connections
“For women to sit in a room and realize they are not alone is incredibly therapeutic. Connection itself reduces the burden of chronic conditions,” points out Dr Gulati.
The doctor points out that women often learn from each others’ experience and this is why social connections are extremely important in this time.
Pay Attention On Sleep
Sleep problems are one of the most common and exhausting symptoms of perimenopause and menopause. Hormonal changes can disrupt deep sleep, causing women to wake up in the early hours, deal with night sweats, and struggle to fall back asleep. When this happens regularly, it leads to severe energy drain, not just tiredness.
To improve sleep, Gulati focuses on simple, practical habits. These include keeping a regular sleep schedule, avoiding caffeine and alcohol in the evening, reducing screen time after 7 p.m., keeping phones out of the bedroom, and practicing calming activities like yoga or meditation. Drinking enough water during the day can also help regulate body temperature at night and reduce hot flashes.
Managing Stress Differently
Instead of trying to eliminate stress, which is often unrealistic, Gulati encourages women to change how they respond to it. Stress is treated as a signal to reassess priorities, set boundaries, and ask for support when needed. This shift helps build resilience and prevents burnout.
Movement Beyond Exercise
Physical activity becomes especially important in midlife, but it’s not just about workouts. Strength training helps protect muscles and bones, while regular movement throughout the day, balance exercises, and flexibility work support long-term health. Reducing long sitting hours is just as important as planned exercise.
Reducing Harmful Habits
Gulati also advises cutting back on alcohol and avoiding tobacco. After menopause, alcohol can worsen sleep, increase belly fat, and raise the risk of conditions like breast cancer and osteoporosis. Limiting late-night screen use can further improve sleep quality.
Eating to Support the Body
Nutrition is another key focus. Rather than aiming for perfection, Gulati encourages small, steady improvements like eating more vegetables and protein, staying hydrated, and choosing foods that may ease menopausal symptoms. The goal is better energy, sleep, and overall health, not just weight loss.
The Hidden Glaucoma Warning Signs Every Middle-Aged Adult Should Know
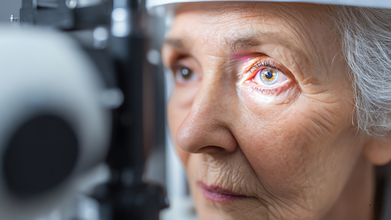
Credit: Canva
Glaucoma is an umbrella term for a group of eye diseases that create pressure inside your eyeball, which can damage delicate, critical parts at the back of your eye, including the optic nerve.
While most of the diseases are progressive, meaning they gradually get worse and eventually cause permanent vision loss and blindness. In fact, glaucoma is the second-leading cause of blindness worldwide and is the leading cause of blindness for people over 60 years old.
Dr Niteen Dedhia, Medical Director, Ojas Maxivision Eye Hospital tells Business Standard: "Glaucoma slowly and quietly causes damage to the optic nerve. Changes in eye pressure, blood flow and nerve fibres occur over time, while the brain often compensates for the loss.
"As a result, symptoms go unnoticed, and by the time vision loss becomes apparent, the damage is usually permanent."
Many forms of glaucoma have no warning signs and the effect is extremely gradual, to the point that you may not notice a change in vision until the condition is in its late stages.
Here are some symptoms that mid-age people need to keep an eye out for:
1. Gradual loss of circumferential vision
One of the earliest symptoms of glaucoma is damage and subsequent loss of peripheral vision. Dr Dedhia noted: “Glaucoma starts by damaging the peripheral vision but doesn’t affect the centre (front) vision."
If you seem to struggle with spotting objects approaching from the side or bump into things more often, you may be experiencing early stages of the disease and not merely experiencing normal ageing.
2. Difficulty seeing or reading in the dark or low light settings
Difficulty adjusting to darkness, discomfort in dimly lit spaces or having trouble navigating at night can be early warning signs may point to reduced contrast sensitivity linked to glaucoma rather than simple eye strain.3. Frequent changes in eye power
Dr Neeraj Sanduja, Ophthalmologist, Eye Surgeon at Viaan Eye Centre, Gurgaon told the publication: "Needing frequent prescription changes or feeling that glasses 'never feel quite right' may reflect subtle visual field changes caused by glaucoma rather than simple refractive error progression."
4. Eye pressure or unusual discomfort
Open-angle glaucoma, the most common form of the condition that causes patchy blind spots in your side vision, is often painless or limited to a mild sense of pressure or heaviness in the eyes.
Those suffering from open-angle glaucoma may notice a dull ache after prolonged screen time or reading that improves with rest. Frequently mistaken as regular eye strain, it is often ignored, however, may indicate subtle increases in eye pressure that require professional evaluation.
5. Frequent headaches with eye strain
Frequent headaches, especially when accompanied by eye strain or blurred vision, should not be ignored as migraine pain as it may signal rising eye pressure or early glaucoma changes, Dr Dedhia warns.
Who Is at Risk for Glaucoma?
Certain groups of people have a higher than normal risk of getting glaucoma which includes those who:
- have high eye pressure
- are farsighted or nearsighted
- have had an eye injury
- use long-term steroid medications
- have corneas that are thin in the center
- have thinning of the optic nerve
- have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body
- are over age 40
- have family members with glaucoma
- are of African, Hispanic, or Asian heritage
© 2024 Bennett, Coleman & Company Limited

