- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Chronic Insomnia Could Increase The Risk Of Dementia By 40%: Study

A new study has pointed out that people who have chronic insomnia could be at higher risk of dementia. One of the best things a person can do to recover from a tiring day, whether it is from a stressful day or after a tiring workout. However, it is not easy for everyone, there are many people who suffer with sleep problems like chronic insomnia.
An estimate of 16.2% of people around the globe suffer with insomnia according to 2025 Sleep Medicine Reviews, which is a condition that makes it hard to fall or stay asleep. A big number of these people have what's called chronic insomnia, meaning they've had this problem for at least three months, with poor sleep happening three or more nights a week.
Previous studies have already connected insomnia to serious health problems like heart disease and diabetes. But now, a new study in the medical journal Neurology has found an even more concerning link: people with chronic insomnia might be at a much higher risk for developing dementia and other memory problems. The study suggests that their brains could be aging faster as a result.
How Does Insomnia Cause Dementia?
For this study, researchers followed 2,750 older adults for an average of five and a half years. At the beginning, everyone was mentally healthy. The researchers found that the people who had chronic insomnia had a 40% higher chance of developing dementia or mild cognitive impairment (MCI).
Researchers explain that this is a huge finding because it means chronic insomnia could be a bigger risk factor for memory loss than having both high blood pressure and diabetes. They also discovered that those who slept less had more of the tell-tale signs of Alzheimer's disease in their brains, like amyloid plaques, and other signs of damage to their brain's blood vessels. This shows that poor sleep isn't just about feeling tired—it's linked to real, physical changes in the brain.
Why You Should Prioritize Sleep?
Experts believe that a big part of the problem is that insomnia is often overlooked. Many older adults just assume that bad sleep is a normal part of getting older. However, doctors stress that chronic insomnia is a real medical issue that goes beyond typical age-related changes. They urge doctors to start talking to their patients about their sleep habits during every check-up.
The good news is that chronic insomnia is a treatable condition. The main treatment is a type of talk therapy called Cognitive Behavioral Therapy for Insomnia (CBT-I). The hope is that by recognizing and treating insomnia, doctors can help protect a person's brain health for years to come.
How Does Insomnia Affect Our Memory
Previous studies have shown that our cognitive abilities are affected by how much we sleep. A 2020 study published in the Journal of Neuroinflammation, explained that there is a strong connection between a person's sleep and their risk of developing Alzheimer's. We know that sleep is crucial for learning and creating memories. Studies have found that a lack of sleep and conditions like insomnia are not just a symptom of Alzheimer's—they may also play a role in its development.
This means that sleep disorders can have a significant impact on whether someone gets Alzheimer's and how fast the disease progresses. Because of this, it's important for doctors to pay more attention to sleep issues when diagnosing and treating patients. By properly screening for and managing sleep disorders, we might be able to help prevent or slow down the progression of Alzheimer's disease.
Bruce Willis’ Wife Emma Says He Is Unaware of His Dementia Diagnosis
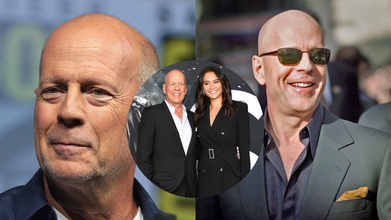
Credits: Wikimedia Commons
Bruce Willis was diagnosed with frontotemporal dementia in 2022. His wife, Emma Heming Willis recalled the day when Bruce was diagnosed with the condition and how it made her feel "lost, isolated and afraid." Talkin to PEOPLE, Emma said, Bruce "never connected the dots" that he has been diagnosed with frontotemporal dementia. “I think that's like the blessing and the curse of this, is that he never connected the dots that he had this disease, and I'm really happy about that. I'm really happy that he doesn't know about it,” she shared about Bruce, 70.
Bruce Willis' Diagnosis
"On the day Bruce got his diagnosis, we walked out of the doctor's office with a pamphlet and an empty goodbye. No plan, no guidance, no hope, just shock," she explained in front of a packed auditorium, People reported.
In one instant, the family's future disappeared. The Oscar-winning actor, famous for his quick wit and performances in Die Hard and The Sixth Sense, would be leaving his career behind. Emma found herself thrust into a whole new role of full-time caregiver at the same time.
She continued to explain, "I found myself having to keep my family intact, raise our two small girls, and tend to the man that I love while dealing with an illness I hardly knew anything about."
Emma's emotional candor resonated with hundreds of families who have received similar diagnoses and encouraged her to author a book, The Unexpected Journey, scheduled for publication in September. In Emma's words, "This is the book I hope will assist the next caregiver. It is packed with encouragement, wisdom, and the encouragement necessary to walk this path.
What Is Frontotemporal Dementia?
Frontotemporal dementia is a less prevalent type of dementia that mainly occurs in the frontal and temporal lobes of the brain. It tends to affect behavior, personality, language, and movement more than memory, particularly in its initial stages.
In contrast to Alzheimer's, which generally strikes older individuals, FTD can hit at an earlier age—sometimes as young as 40. The symptoms can range from changes in personality, emotional flatness, or the inability to show empathy to impulsiveness, so it is especially hard for spouses and children to cope.
Emma's case illustrates how abrupt and disrupting this diagnosis can be—not only for the patient but for caregivers as well.
Whereas Bruce Willis' diagnosis hit global headlines, the mental toll taken by Emma, his caregiver, was largely in the background—until she decided to come forward.
Caregiving is a respectable position, but it's also a challenging and thankless one. For those who are caring for loved ones with dementia or other chronic illnesses, the stress of "keeping it all together" can result in a condition called caregiver burnout.
"Caring for someone is the most intimate and demanding work of love," Emma explained, "but when you're not noticed or supported, it begins to undermine your health—mentally and physically."
‘Work Stress Makes You Gay’: Why Malaysian Minister's Remark Proves The Need To Understand Sex, Gender And Sexuality

Credits: X and Canva
Work stress could make you gay, said a Malaysian minister Zulkifli Hasan, as continued government intervention of what is described as 'sexually deviant behavior' has pressured the country's LGBTQ community. This happened two weeks after religious authorities and police acted on complaints from a sultan and Islamist politicians that a camping retreat was promoting the LGBTQ lifestyle, reported South China Morning Post.
Religious Affairs Minister Hasan on Tuesday said that work stress could be among many other factors that is pushing people into sexual orientations other than heterosexuality. “Societal influence, sexual experiences, work stress and other personal factors come under this category [of possible causes],” Zulkifli said in a written parliamentary reply to a question by Siti Zailah Mohd Yusoff, a lawmaker with the opposition Islamist party PAS.
Also Read: Andy Kershaw Diagnosed With Spinal Cancer That Left Him Unable To Walk
He cited a 2017 study by Sulaiman et.al., that said such elements "can contribute to the increase in LGBT acts".
His comments have attracted a lot of backlash, with many people on social media mocking him. A social media user Muaz Zam said, "By this logic, I am genuinely shocked my entire office isn't gay by now". Another one read: "In other words: they never work hard in the parliament."
However, these claims are not scientifically back. Work related stress can impact a person, but cannot change their sexuality. It can, however, cause health effects. What it does not do is change one's sexuality and this is why one should know the difference about gender, sex and sexual orientation or sexuality.
'Work Stress Makes You Gay': The Difference Between Gender vs Sex

While these both terms are often used interchangeably in official forms, there is a difference between the two.
As per the Council of Europe, gender is an area that cuts across thinking about society, law, politics, and culture.
Read: Trump Administration Deadnames Transgender Former HHS Officer Rachel Levine in Official Portrait
Definition Of Gender vs Sex by WHO
The World Health Organization notes that sex refers to: "the different biological and physiological characteristics of males and females, such as reproductive organs, chromosomes, hormones, etc.”
Whereas, gender refers to: "the socially constructed characteristics of women and men – such as norms, roles and relationships of and between groups of women and men. It varies from society to society and can be changed. The concept of gender includes five important elements: relational, hierarchical, historical, contextual and institutional. While most people are born either male or female, they are taught appropriate norms and behaviours – including how they should interact with others of the same or opposite sex within households, communities and work places. When individuals or groups do not “fit” established gender norms they often face stigma, discriminatory practices or social exclusion – all of which adversely affect health."
Definition Of Gender vs Sex by The European Institute For Gender Equality
“Sex refers to the biological and physiological characteristics that define humans as female or male. These sets of biological characteristics are not mutually exclusive, as there are individuals who possess both, but these characteristics tend to differentiate humans as females or males.”
“Gender refers to the social attributes and opportunities associated with being female and male and to the relationships between women and men and girls and boys, as well as to the relations between women and those between men. These attributes, opportunities and relationships are socially constructed and are learned through socialisation processes. They are context- and time-specific, and changeable. Gender determines what is expected, allowed and valued in a woman or a man in a given context. In most societies, there are differences and inequalities between women and men in responsibilities assigned, activities undertaken, access to and control over resources, as well as decision-making opportunities. Gender is part of the broader sociocultural context. Other important criteria for sociocultural analysis include class, race, poverty level, ethnic group and age.”
The main difference is that gender is a social construct, whereas sex is the biologically labelled term based on organs and hormones.
Read More: Trump's Top Health Nominee Wants ‘Corrective Care’ For Trans People
What Is Sexuality?

As per the American Psychological Association (APA), sexuality is the capacity to derive pleasure from various forms of sexual activity and behavior. The Lanarkshire Sexual Health describes sexual orientation as a way to describe the feelings you have for someone you fancy or are attached to.
While sexuality can change overtime, it is not a choice. There is no evidence that sexual orientation can be forced to change through therapy.
Can Stress Impact Sexuality?
While stress can impact sexual function by reducing libido, causing fatigue, and triggering hormonal changes, it does not change one's sexual orientation. Jason Teoh, who writes on LGBTQ issues, project partner at NSW Department of Planning, Housing and Infrastructure, notes: "Sexual orientation is not caused by stress. It is not caused by trauma, influence or difficult life circumstances."
The WHO notes: sexual orientation is a natural, stable part of human identity shaped by biology, genetics, and early development. The WHO removed homosexuality from its disease classification in 1990. The American Psychiatric Association did the same in 1973.
The 4 Parkinson's Signs That Appear Years Before Diagnosis

Credit: Canva
Parkinson's disease is a progressive, neurodegenerative movement disorder caused by the loss of dopamine-producing brain cells, primarily affecting people over 60. Apart from motor loss, the disease also causes cognitive decline, depression, anxiety and swallowing problems.
The first symptom may be a barely noticeable tremor in just one hand or sometimes a foot or the jaw. Over time, swinging your arms may become difficult and your speech may become soft or slurred. The disorder also causes stiffness, slowing of movement and trouble with balance that raises the risk of falls.
However, before clear symptoms begin to appear, Neurologist Rachel Dolhun says certain signs may help identify the onset of the disease decades before it is diagnosed.
“It’s important to stress that not everyone who has these symptoms goes on to develop Parkinson’s,” said neurologist Rachel Dolhun. “But we know that in some people, these can be some of the earliest signs," she told The Washington Post.
Here is what you should look out for:
1. Loss Of Smell
Loss of smell, or hyposmia, is a common and early non-motor symptom of Parkinson's disease, affecting up to 90 percent of patients. This symptom can significantly impact quality of life by reducing the enjoyment of food and diminishing appetite.
While strongly linked to Parkinson's, smell loss can also stem from other causes, including sinus problems, COVID-19, or aging.
2. Acting Out Dreams
Acting out dreams, known as REM Sleep Behavior Disorder (RBD), involves physically enacting vivid, often unpleasant dreams through shouting, punching, or kicking during sleep.
This typically happens because the brainstem fails to temporarily paralyze muscles during REM sleep. It is a strong early warning sign of Parkinson's disease, often appearing years or decades before motor symptoms. About 50 percent of people with Parkinson's experience RBD.
READ MORE: Parkinson’s Patients May Soon Walk Better With This New Personalized Brain Therapy
3. Constipation
Constipation is a very common and significant non-motor symptom of Parkinson's disease that is caused by nerve changes slowing gut muscles and potentially exacerbated by low activity and dehydration.
Constipation can also be caused by Parkinson's medications such as anticholinergics, amantadine and other common drugs such as opioids, iron/calcium antacids.
4. Dizziness As You Stand
The autonomic nervous system fails to properly constrict blood vessels or increase heart rate upon standing, often due to a lack of norepinephrine. This causes the autonomic nervous system to fail in regulating blood pressure. Over time, this leads to Neurogenic Orthostatic Hypotension.
Beyond dizziness, symptoms include blurred vision, weakness, fatigue, cognitive "fog," and "coat hanger pain" (pain in the neck/shoulders). Often times, patients experience dizziness in the morning or immediately after meals.
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking questions and reviewing your medical history. Various imaging and diagnostic tests used to detect disease includes CT scan, PET scan, MRI scan and genetic testing.
© 2024 Bennett, Coleman & Company Limited

