- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Could Your Bathroom Habits Signal Colon Cancer? 5 Warning Signs You Shouldn't Ignore

Could Your Bathroom Habits Signal Colon Cancer? 5 Warning Signs You Shouldn't Ignore
Colon cancer is one of the major cancers that kill individuals worldwide, representing a form of colorectal cancer. This is a cancer that starts in the colon but can spread into the rectum, and the incidence is on the rise to raise a serious health concern. Colon cancer often produces no symptoms in its early stages, but when it is detected, treatment can be incredibly effective, considering that it develops slowly.
The incidence of colorectal cancer in the young is increasingly becoming an issue, and knowledge of the symptoms and importance of screening for this disease is critical.
The Colorectal Cancer Alliance estimates that around 150,000 Americans are diagnosed annually. In response to this rise, medical professionals encourage people to recognize early warning signs and undergo regular preventive screenings, such as colonoscopies, since they are "lifesavers" because they can detect the disease very early.
Uncommon Symptoms
The more people know about colon cancer, the more they must be aware of its symptoms, many of which can occur at any time and thus lead to a visit to a medical doctor for examination. A cancer specialist such as Dr. Waqqas Tai believes that "Even subtle changes in bowel habits or unexpected weight loss should not be brushed off lightly." He suggests a visit to a primary care physician if you've experienced any of the following symptoms:
Pencil-Thin Stools
Narrow stools may be indicative of a tumor in the colon, especially if the stool occurs near the bottom portion of the colon or in the lining itself. As Dr. Michael Cecchini, who is both a medical oncologist as well as co-director of the colorectal program at the Center for Gastrointestinal Cancers at Yale Cancer Center, noted, this symptom is "highly concerning." The stool will change shape because the forming obstruction from the tumor is obstructing the digestive pathway as it takes the form of a pencil.
Blood in the Stool
Blood in the toilet is never good news and should not be ignored. Sometimes, rectal bleeding results from hemorrhoids or anal fissures, but at other times, this could be a symptom of colon cancer. According to the Cleveland Clinic, blood in the stool warrants immediate medical attention to determine its cause. General surgeon Dr. Terry Simpson comments, "It may be nothing, but it may be something, and it's not worth betting your life for."
Anemia
Low red blood cell count or anemia has been said to be a potential symptom of colon cancer when it is triggered by a tumour hemorrhaging into the digestive tract. Actually, studies show that anemia develops in 30-75 percent of patients suffering from colorectal cancer.
According to Dr. Tai, "There's no healthy reason a man should be anemic." Low hemoglobin in women can also indicate an underlying issue or medical condition, like a deficit that ought to be explored through a colonoscopy, aside from heavy menstrual bleeding.
Acute Constipation and Diarrhea
The classic gastrointestinal symptom is alternating between very severe constipation and diarrhea, but this could be a sign of a blockage or tumor in the colon when persistent. Experts tell patients that these symptoms should "raise red flags" for them to have a colonoscopy done to rule out cancerous growth.
Unexplained weight loss, fevers, and night sweats
These symptoms fall together under the banner of "B symptoms," which usually come with the diagnosis of cancer. According to Dr. Tai, if a patient experiences hot flashes at night, weight loss without any alteration in eating behavior, and periodic fever in the daytime, attention needs to be strictly paid. Such symptoms, in some instances, can be indicative of the late stage of the disease and need an immediate checkup.
Why Early Screening Matters
The USPSTF suggests screening for colorectal cancer in adults aged 45 to 75 years. Those above and below this age range who are at increased risk should also be screened. Such individuals include those with a familial history of colorectal cancer or inflammatory bowel disease, or those who present with the symptoms discussed above.
Routine screening like colonoscopy helps identify the early stages of colon cancer potentially curable before it becomes uncontrollable.
Dr. Tai said colonoscopies are easy, painless procedures that may save your life if done before cancer progresses. Recently, he took to social media to beg people to please go visit their primary care physician and have a routine colonoscopy. One can prevent himself/herself from being a victim of this disease.
Preventive Steps
First of all, know the warning signs for colon cancer. Here are some important steps you can take:
1. Familiarize with symptoms: Pay attention to the following symptoms and seek appropriate medical advice if they are persistent: persistent changes in bowel habits, presence of blood in stools, unexplained weight loss, and unusual night sweats.
2. Routine Screening: The proper follow-through on screening guidelines for any individual who has an increased chance, like getting older and family history.
3. Healthy Lifestyle: Sound diet with lots of fiber, within healthy weight range, and exercise can reduce the risk of developing colon cancer further.
Colon cancer is a serious medical condition, with the incidence among young individuals on the rise. Early detection, coupled with regular screenings, reduces the risk of advanced stages. Detection in its early stage and treatment can ensure the problem of colon cancer is eradicated. The symptoms, therefore, can be lifesavers.
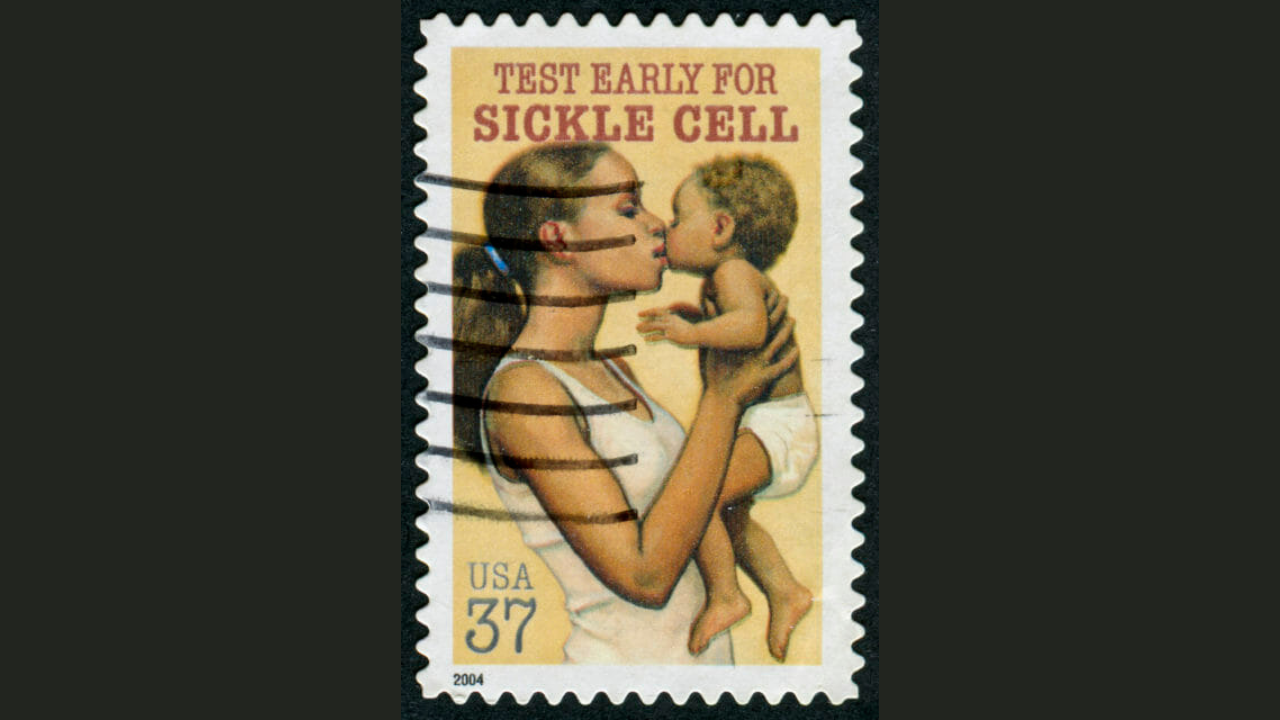
Sickle Cell Disease: Tracing The History Of The First Ever Genetic Disease To Be Diagnosed

Credits: PIB
A parasite that causes malaria is halted by sickle cells and makes people who carry the sickle cell trait more resistant to the disease. This is why sickle cell trait also occurs more in people who live in tropical and sub-tropical regions where cases of malaria were or still is common.
It comes from the copy of an abnormal sickle or the HBB gene and one copy of the normal HBB gene. The gene is an evolutionary response to malaria, where humans begin to develop an abnormal HBB gene and pass it onto to the next generation.
The "Black Disease"
The earliest documentation of sickle cell symptoms in medical texts could be found from the 1870s. However, it had not been formally identified until in 1910. when the first case was detected in the United States. The first case of sickle cell disease or SCD in the US was in 1904, when Walter Clement Noel, a 20-year-old dental student from Grenada, sought care for anemia at Chicago Presbyterian Hospital, where he met Dr James B Herrick. Dr Herrick was a cardiologist and professor of medicine and he was assigned noel who had experienced recurrent episodes of "muscular rheumatism" and "bilious attacks" over a period of 3 years.
This case was assigned to an intern Dr Ernest E Irons by Dr Herrick. Dr Ernest performed initial blood work on Noel and observed the unusual sickle-shaped red blood cells in the sample under the microscope. This is when Dr Herrick was told about it, leading to him publishing the first documented case study of SCD, titled, "Peculiar Elongated and Sickle-Shaped Red Blood Corpuscles in a Case of Severe Anemia."
However, the name, sickle cell anemia, was not coined until in 1922, by Vernon Mason. It was also the first diagnosed genetic disease and the first to be linked to the hemoglobin protein.
But, how did it gain the name "Black Disease"? This is because the disease often disproportionately affected Black Americans in the US, which caused racial bias and prevented people with sickle cell from receiving quality care.
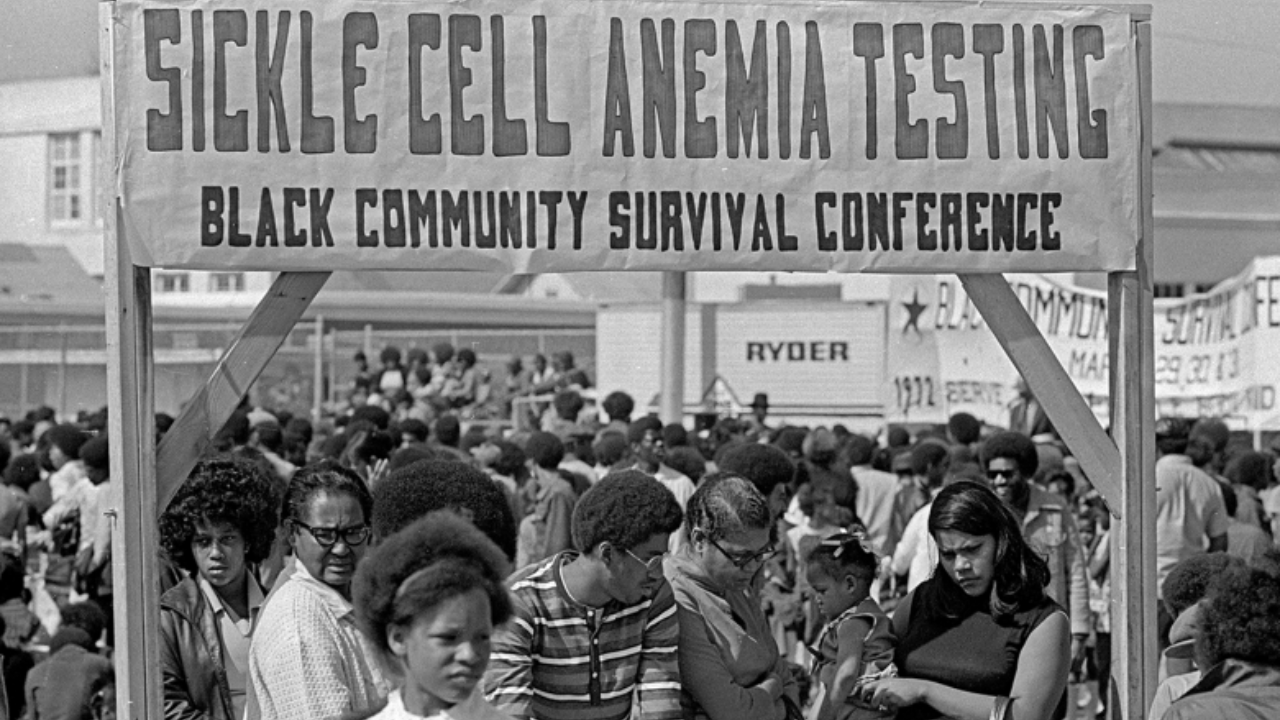
In response to this, in the 1960s, the Black Panther Party worked to expand community-based care for education and treatment of this disease. This was part of their initiative to tackle the sickle cell, which received little to no attention because it mostly affected a large part of Black community.
While Herrick may have described the first known case in the US, SCD did exist for generations in African and Mediterranean descent, due to the regions being prone to diseases like malaria. In African medical literature, it was known as "ogbanjes", which loosely translated into "children who come and go" as the infants born with this disease had a high mortality rates. One of the first records, as is also noted by the Sickle Cell Association from Africa is from a Ghanian family in 1670.
A Groundbreaking Discovery
In 1927, scientists Hahn and Gillespie made a discovery that reshaped our understanding of blood disorders. While studying red blood cells in a low-oxygen environment saturated with carbon dioxide, they observed a curious phenomenon: the cells twisted into sickle shapes—not just in patients with sickle cell disease (SCD), but sometimes in people without any symptoms at all.
This puzzling observation hinted at an invisible carrier state and eventually led to the identification of what we now call the sickle cell trait.

Fast-forward to the late 1940s and early 1950s, and the pieces of the puzzle began falling into place. In 1949, two scientists working continents apart independently uncovered the genetic blueprint of SCD.
Col. E. A. Beet, a military physician stationed in what is now Mozambique, published his findings in an African medical journal. Around the same time, Dr. James V. Neel at the University of Michigan released a parallel study in the journal Science. Both revealed that SCD follows an autosomal recessive inheritance pattern—meaning the disease only occurs when a person inherits two copies of the mutated gene. Those with just one copy? They carried the trait, but not the illness.
Together, their work laid the foundation for our modern understanding of genetic inheritance and reshaped how we screen for and manage sickle cell disorders today.
Heart Health Risk In Women Could Be Associated To Infertility: Study

(Credit-Canva)
Roughly one out of six people globally suffer with infertility according to the World Health Organization. A common issue that affects many, infertility, is a condition where a person is unable to reproduce offsprings. While the condition may be common, it can cause a lot of health problems as well as stress for people who wish to have children. To tackle this, people often opt for fertility treatment including reproductive technology called in vitro fertilization (IVF). However, could your infertility be a sign of impending health issues?
A new evidence review suggests a link between infertility in women and a heightened risk of heart problems, particularly among younger women and those undergoing fertility treatments.
Is Infertility An Early Warning for Heart Health?
Infertility may serve as an early sign for future heart health issues, according to researchers at the National and Kapodistrian University of Athens in Greece. This finding was recently presented in Copenhagen, Denmark, at a joint meeting of the European Society of Pediatric Endocrinology and the European Society of Endocrinology.
Researchers looked at data from many different studies – almost 21 of them! They compared nearly 179,000 women who couldn't get pregnant with about 3.4 million women who didn't have fertility issues. What they discovered was that women who were infertile had a higher chance of facing heart issues:
- They were 17% more likely to get heart disease, which is a general term for problems with the heart itself.
- They had a 16% higher chance of having a stroke, which happens when blood flow to the brain is blocked.
- They were 14% more likely to have problems with their heart or blood vessels in general.
Elevated Risk for Younger Women and Those Undergoing Treatment
The research highlights two groups of women who face an even bigger risk. First, it's younger women. The study found that women under 40 who were infertile had a 20% higher chance of heart disease. That's a significant increase for younger individuals. Second, it also showed that women who went through fertility treatments (like IVF) had an 18% greater risk of heart problems. This suggests that either the treatments themselves or the underlying reasons for needing them could be connected to heart health.
Implications for Clinical Care
Researchers believe that because infertility might be an early sign of heart problems, doctors can use this information. They can identify women who might need extra check-ups or special strategies to prevent heart disease earlier in life. It's like giving doctors a heads-up to be more careful with these patients. She also brought up an important question: what are the long-term effects of fertility treatments on a woman's heart? This is something doctors need to consider.
Researchers want to follow women’s health over time to really understand why infertility might be linked to heart health. They hope to figure out the exact biological reasons behind this connection and identify which specific groups of women are most at risk. The ultimate goal is to use all this information to create better guidelines for preventing heart disease early on and to improve heart care for women who have had infertility.
World Kidney Cancer Day: ‘Overusing 'Safe’ Painkillers Are A Hidden Cause Of Kidney Cancer

Headache? Take a painkiller. Joint pain? Take another. For all of us, over-the-counter (OTC) painkillers such as ibuprofen or acetaminophen are as much a part of daily life as a morning cup of coffee. They're fast, efficient, and appear harmless—who needs a prescription, anyway? But what if this blase dependence on painkillers is actually laying the groundwork for a much more devastating health emergency?
If that's your daily mantra, don't worry, you're in good company. In the age of instant gratification, all of us are turning to over-the-counter pain relievers as a quick fix for even mild pain. But what if this ostensibly innocuous habit is silently threatening your kidneys with a major health problem?
Painkillers, or analgesics, are usually a lifeline for individuals with chronic or severe pain. From recovery from surgery and migraines to arthritis and menstrual cramps, these drugs offer relief that ensures our quality of life is not drastically reduced. But beneath the pain relief lies a surprising question: whether the overuse of these drugs may exact too high a price-kidney damage and even kidney cancer.
Dr. Aditya Punamiya, a GI, HPB, and Gynecologic Oncosurgery Consultant, cautions, "The long-term and uncontrolled use of over-the-counter painkillers is emerging as an under-diagnosed but serious risk factor for kidney cancer." Dr Punamiya observations reveal an alarming pattern, numerous patients self-medicate for chronic pains—headaches, joint pains, or back pain—unaware of the additive damage to the kidneys.
Why We Turn to Painkillers So Easily?
Pain is a biological alarm system. Helpful in warning us of injury or sickness, chronic pain can strongly interfere with our functioning on a daily basis. To counter this, painkillers provide a feeling of control and comfort. For acute on-demand pain and chronic inflammatory diseases, drugs like NSAIDs and acetaminophen are not only handy but effective as well.
Sadly, the very ease of use of these drugs has led to their misuse. Painkillers are increasingly being consumed without medical supervision, particularly in nations such as India where OTC availability is prevalent but even within well-regulated economies such as the U.S., long-term use has become an undercurrent of an epidemic.
What Are The Types of Painkillers?
Over-the-Counter (OTC) Medications
Paracetamol (Acetaminophen): Good for fever and light pain, but hepatotoxicity is a serious issue above moderate doses.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Contains ibuprofen, naproxen, and diclofenac. These are useful for pain that is inflammation-related but have gastrointestinal and renal toxicity with long-term use.
Prescription Painkillers
Opioids (Tramadol, Morphine, Oxycodone): For severe pain only but pose the risk of respiratory depression, addiction, and endocrine disruption.
Topical and Alternative Therapies
Topical creams and patches containing drugs such as menthol or capsaicin are localized treatments with fewer systemic hazards.
How Do these Drugs Harm the Kidneys?
How do such drugs damage the kidneys? Dr. Punamiya clarifies, "Drugs such as ibuprofen, diclofenac, and naproxen, if taken in excess, can harm the kidneys in two ways. One, they weaken the kidneys' function to filter blood by cutting off blood supply. Two, they cause chronic interstitial nephritis over time, scarring kidney tissues." This scarring provides a fertile ground for RCC to grow.
The kidneys, essential organs responsible for filtering waste products from the blood, are especially susceptible to chronic exposure to NSAIDs and acetaminophen. Acute kidney injury, chronic kidney disease, and, in severe cases, kidney failure can result from excessive use of these compounds. The transition to kidney cancer is not as sudden but equally alarming, since the cumulative insult changes cellular mechanisms, possibly initiating malignant growth.
A landmark meta-analysis by Toni K Choueiri, Youjin Je, and Eunyoung Cho has again highlighted the relationship between chronic painkiller use and renal cell carcinoma (RCC)—the leading form of kidney cancer.
Non-Aspirin NSAIDs: Chronic use was linked to a 25% enhancement in the risk of RCC. Heavy consumption increased that threat by 56%, long-term consumption for more than 10 years especially concerning for women.
Acetaminophen: Associated with a 21% heightened risk of kidney cancer. Heavy users who took high doses saw their risk rise by 66%.
Aspirin: While most U.S.-based research found no conclusive link, some research from other countries suggested a connection, possibly due to regional variation in formulation or consumption habits.
Why Kidney Cancer Is a Silent Threat?
Kidney cancer is especially stealthy since it usually presents late without any symptoms. "Flank pain, hematuria and weight loss are typically late presentations," states Dr. Punamiya. For patients such as Sarah, who might have been taking painkillers for years, these signs may only manifest by the time cancer has metastasized, and so treatment is less effective.
Risk factors such as smoking, hypertension, diabetes, and obesity increase the risk, particularly in individuals with previous long-term analgesic use. Women also have an increased risk with non-aspirin NSAIDs, possibly because of hormonal or metabolic variation, although further work is required to explain this difference. He describes two principal mechanisms:
Decreased Renal Blood Flow: NSAIDs inhibit prostaglandins, decreasing kidney blood flow and compromising kidney filtration capability.
Chronic Interstitial Nephritis: Long-term NSAID use leads to fibrosis and inflammation of kidney tissue, setting the stage for RCC.
"Most patients self-treat for headaches or joint pain without knowing they're gradually driving their kidneys towards failure," he adds.
Why Early Detection Of Kidney Cancer Symptoms is Difficult?
Kidney cancer is infamous for its asymptomatic nature in the early stages. By the time symptoms such as pain in the flank, hematuria (urine containing blood), or unexplained weight loss appear, the disease is usually advanced. Patients with pre-existing risk factors—such as smoking, hypertension, and diabetes—and with a history of analgesic abuse are particularly susceptible.
Dr. Punamiya advises individuals to consult a doctor for ongoing pain rather than resorting to self-medication. "Routine screening and preventive caution are necessary, especially for vulnerable groups," he points out.
What Are Ways You Can Manage Pain Management Smartly?
Not every use of painkillers is risky. "Short-term, doctor-monitored use is generally safe," says Dr. Punamiya. The trick is not entering into uncontrolled, long-term use. Here's how to handle pain more safely:
Consult a Healthcare Provider
For long-term pain, consult a professional to treat the underlying condition, whether arthritis, neuropathy, or migraines. A customized treatment plan can minimize painkiller dependency.
Try Non-Drug Options
Physical therapy, acupuncture, yoga, and cognitive-behavioral therapy can treat chronic pain without medication risks. For sudden pain, ice, heat, or rest may be enough.
Use Painkillers Wisely
Follow instructions on dosing and avoid prolonged use outside of medical guidance. For NSAIDs, eat food when taking to reduce stomach discomfort, and drink enough fluids to aid kidney function.
Take Precautions
Encourage regular health screening for early detection of kidney problems, particularly among high-risk groups. Dr. Punamiya urges "preventive vigilance" with follow-up visits and attention to early signs such as blood in the urine or recurrent flank pain.
Lifestyle Matters
A balanced diet, exercise, and weight control can cut pain from conditions such as arthritis while reducing kidney cancer risk factors such as obesity and high blood pressure.
There may be the temptation to cover up pain instead of comprehending its cause but swallowing a pill with a glass of water can be an instant solution that might come at a price of long-term health. The growing body of evidence linking commonly used painkillers to kidney cancer is a call for informed, cautious use. As more people take their health into their own hands, the importance of education, medical guidance, and moderation cannot be overstated.
© 2024 Bennett, Coleman & Company Limited

