- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Explained: Can Stomach Cancer Spread To Other Organs?

Stomach Cancer (Credit: Canva)
Stomach cancer develops in the lining of the stomach. Also, known as Gastric cancer, it affects the elderly more than the adult. According to the American Cancer Society, about 6 of every 10 people diagnosed with stomach cancer each year are 65 or older. Also, the lifetime risk of developing stomach cancer is higher in men (about 1 in 101) than in women (about 1 in 155).
Oncologist Dr Pankaj Kumar Pande, Director–Surgical Oncology, Max Super Speciality Hospital, Shalimar Bagh, Delhi explained that this form of cancer spreads through three main pathways: Direct spread, lymphatic spread, and bloodstream.
1. Direct Spread: In its early stages, stomach cancer can invade nearby tissues and grow into the deeper layers of the stomach or spread to surrounding organs such as the oesophagus, liver, pancreas, or intestines.
2. Lymphatic Spread: Cancer cells can travel through the lymphatic system. The most common areas affected are the regional lymph nodes near the stomach, particularly those around the liver and diaphragm.
3. Bloodstream: "Cancer cells can enter the bloodstream and travel to distant parts of the body," which is a common route for stomach cancer to metastasize to distant organs.
He further explained that cancerous cells spread from the original tumour to other parts of the body through a process called Metastasis. The most common sites for the spread are the liver, lymph nodes, peritoneum, lungs, bones, and ovaries.
What Are the Early Warning Signs of Stomach Cancer?
The early warning signs of stomach cancer are often subtle and can be easily overlooked. Some of the common early signs include:- Indigestion or Discomfort: Mild indigestion, bloating, or a feeling of fullness after eating can often be dismissed as normal but may indicate an early stage of stomach cancer.
- Loss of Appetite: A lack of interest in food or feeling full quickly, which can be intermittently noticed and often attributed to stress or other non-cancer causes.
- Unexplained Weight Loss: Losing weight without trying or experiencing an unexplained drop in appetite, which may signal cancer progression.
- Abdominal Pain or Discomfort: Persistent or occasional pain in the stomach area, often after eating, can become more severe as the condition progresses.
- Nausea or Vomiting: Nausea, sometimes accompanied by vomiting, may occur especially after meals and is linked to cancer blocking or irritating the stomach.
- Heartburn or Acid Reflux: Persistent heartburn that doesn't respond to usual treatments could signal stomach cancer.
Dr Pande notes that "In the early stages, these symptoms tend to be mild and intermittent," leading many to attribute them to less serious digestive issues. Unfortunately, this often results in the cancer being diagnosed at a more advanced stage.
Recommended Lifestyle Changes After Cancer Treatment
After undergoing treatment for stomach cancer, adopting lifestyle and dietary changes can significantly improve recovery and reduce the risk of recurrence. Dr Pande advises patients to focus on a balanced diet, consisting of fruits, vegetables, whole grains, lean proteins, and fiber-rich foods, to aid digestion and overall health. "Eat small, frequent meals and stay hydrated with fluids like water or herbal teas," he recommends.As far a lifestyle alterations are concerned, he emphasizes the importance of regular physical activity, starting with light exercises to rebuild strength. He also suggests managing stress through relaxation techniques and prioritizing adequate sleep (7-9 hours a night) for effective healing. Additionally, regular check-ups and screenings are vital for ongoing monitoring.
Why the Inches on Your Neck Are More Dangerous Than Your Waistline?

Credits: Canva
When most people think about weight and health risks, the waistline is the focus. Doctors and researchers often measure body mass index (BMI) or waist-to-hip ratios to estimate whether someone is at risk of conditions like heart disease or diabetes. However, growing body of research indicates a different, often neglected measurement- neck size.
It might come as a shock, but neck size could provide an important insight into your risk for severe health conditions such as heart disease, diabetes, and sleep disturbances. And the part that might raise an eyebrow: even individuals with a healthy BMI are not in the clear. A thicker neck can be dangerous even in those who otherwise appear to be fit and healthy.
Neck size has nothing to do with appearance or clothing fit. Neck size is a reflection of fat distribution in the upper body. Upper-body fat is metabolically active; it releases fatty acids, hormones, and inflammatory factors into the blood more easily than fat elsewhere on the body, such as the hips and thighs.
When such substances overwhelm the system, they upset cholesterol equilibrium, increase insulin resistance, clog blood vessels, and ignite long-term inflammation. Eventually, that chain reaction elevates the risk for several conditions, ranging from cardiovascular disease to type 2 diabetes.
In a sense, neck size serves as a proxy for visceral fat—the unhealthy type that encircles inner organs and speeds up cellular aging.
What Is The Link Between Neck Size And Diseases?
Clinical evidence highlights just how potent this relationship is. Studies reveal that individuals who have thicker necks have a higher chance of developing:
Cardiovascular diseases like hypertension, atrial fibrillation (irregular heart rhythm), and even heart failure. Atrial fibrillation is especially worrying as it raises the risk of stroke and may ultimately lead to heart failure.
Coronary heart disease, where constricted arteries decrease the supply of oxygen-containing blood to the heart.
Type 2 and gestational diabetes, both associated with insulin resistance caused by upper-body fat.
Obstructive sleep apnea, a sleep disorder in which the airway repeatedly collapses, cutting off breathing. This disorder not only induces fatigue but also stresses the cardiovascular system.
The connection is so strong that more and more physicians now add neck size to sleep apnea assessments.
A 2022 study went further, linking a bigger neck to an elevated risk of erectile dysfunction in men, continuing to add another layer to the unseen risks of too much upper-body fat.
What Qualifies as a Risky and Dangerous Neck Size?
Scientists have found thresholds where risks become much higher:
- For men, a 17-inch (43 cm) or larger neck circumference.
- For women, 14 inches (35.5 cm) or larger.
What's surprising is that such risks continue even among individuals with normal BMI or healthy weight. And for each extra centimeter above these thresholds, research indicates increasing hospitalizations and deaths.
This implies you may be "healthy" on paper in terms of BMI, yet your neck circumference may tell a different tale.
Sleep, Stress, and Metabolic Strain
The implications of a thick neck go beyond the development of chronic disease. Obstructive sleep apnea is a perfect case in point. Individuals with larger necks have a higher risk of airway collapse when they sleep, resulting in broken sleep, dips in oxygen, and extreme exhaustion during the day. This then increases risks for accidents, cardiovascular stress, and poorer quality of life.
Aside from apnea, degraded quality sleep exacerbates metabolic control. If the body doesn't receive restorative sleep, blood sugar management, hormone function, and appetite take a hit—propelling the vicious cycle of weight gain and risk of disease.
Neck Size and the Obesity Epidemic
The significance of neck circumference is exacerbated by the trends in obesity in the modern world. In America, close to 2 out of every 5 adults and 1 out of every 5 children are obese, based on the Centers for Disease Control and Prevention. Scholars observe that though the risk factor is in neck circumference across populations, it is most specifically relevant for individuals already with a history of living with obesity.
This makes it a potentially potent agent for determining people most at risk, more than BMI or waistline alone can indicate.
Measuring your neck circumference can be done in less than one minute. With a tape measure, place it around the thinnest area of your neck so that it is snug but not constricting.
If the measurement is over the thresholds, it's not a reason for alarm, but it's a good idea to take it seriously. Neck circumference is just a piece of the health puzzle, but it can be an early warning sign—one you have control over.
What Can You Do To Reduce Neck Circumference?
Yes, your neck size can change. Targeted lifestyle changes can lower fat stored in the upper body, including the neck. Here's how:
- Cardiovascular activity such as walking, swimming, or cycling burns fat and lessens total adiposity.
- Strength training builds muscle and enhances a higher rate of metabolism, making it simpler to maintain fat off in the long run.
- Optimal sleep regulates hormones associated with appetite and fat storage.
- Well-balanced nutrition—prioritizing whole grains, vegetables, fruits, pulses, lean protein, and healthy fats—maintains metabolic health without surplus calories.
The secret is consistency. Regular healthy habits over time shrink visceral fat, which can then lower neck circumference and reduce the risk of associated health issues.
Medical professionals warn against substituting neck circumference for a complete medical evaluation, but it can be used as a simple, underutilized measurement to accompany BMI and waistline checks. For others, it could be the initial indicator that triggers further examination.
Social Connection Isn’t Just Fun: How Socializing Could Literally Add Years To Your Life?

Credits: iStock
Food, water, and oxygen are the obvious essentials for survival but to truly thrive, our brains demand something else: human connection. Social interaction is not a luxury, it is as vital to our wellbeing as exercise or sleep. Whether it’s a quick chat with a neighbor, a phone call with a friend, or a day spent volunteering, the evidence is piling up that socializing does more than lift our spirits. It may actually help us live longer.
A new study published in the Journal of the American Geriatrics Society found that older adults who stay socially active are significantly more likely to live longer compared to those who are socially isolated. That single finding adds weight to decades of research showing that connection is one of the strongest predictors of healthy aging.
Are Humans Wired for Social Connection?
Unlike solitary animals, humans evolved as pack creatures. Our survival has always depended on working together, relying on one another for food, safety, and support. Even in modern life, this wiring hasn’t changed. Whether you thrive in large groups or prefer just a handful of close relationships, your brain still needs meaningful social contact.
Neuroscientists have discovered that interacting with others activates brain regions that remain dormant when we’re alone. These regions are linked to empathy, judgment, and communication. Without stimulation, they weaken over time, contributing to cognitive decline. Research shows that consistent socialization can slow the onset of dementia and preserve memory function. In contrast, chronic isolation can shrink brain volume and accelerate mental decline.
The recent U.S. study followed more than 2,200 adults aged 60 and older. Researchers collected lifestyle data, psychosocial assessments, and blood samples, then tracked the participants for four years. The results were striking: those with high levels of social engagement were 42% less likely to die during that period than those with little or no engagement.
It wasn’t just any kind of interaction that mattered. Certain activities—like volunteering, caring for grandchildren, or joining sports clubs—had particularly strong links to longer life. These activities share a few traits: they provide purpose, involve movement, and encourage ongoing interaction with others.
Lead author Ashraf Abugroun of the University of California, San Francisco, put it plainly: “Staying socially active is more than a lifestyle choice. It is closely linked to healthier aging and longevity.”
What is The Biology Behind 'Socialising'?
Why does socializing influence longevity so strongly? Researchers point to two interconnected factors: biological aging and physical activity.
Social engagement appears to slow down markers of biological aging in the body. People who remain active in community or group settings often show healthier inflammatory profiles, better immune function, and improved cardiovascular health. At the same time, social life encourages movement—whether it’s walking with a friend, dancing at a community event, or gardening with neighbors. Physical activity itself reduces risk of chronic disease and extends lifespan, and social settings make that activity more consistent and enjoyable.
Benefits of Social Connection for Human Beings
The benefits aren’t only physical. Social activity is strongly tied to mental health. Research has consistently shown that loneliness increases the risk of depression, anxiety, and even suicide. On the other hand, maintaining friendships and close relationships boosts self-esteem, lowers stress hormones, and fosters resilience.
For example, group activities such as exercise classes or community clubs provide a natural buffer against daily stress. Conversations and shared experiences remind us we’re not alone in our challenges. A 2016 study in Psychology and Aging found that people who remain socially active into late life report higher satisfaction and happiness than those who withdraw. Happiness itself has been shown to improve health outcomes, creating a reinforcing cycle.
COVID-19 reminded us of the costs of isolation. Lockdowns cut people off from family, friends, coworkers, and community activities. Rates of depression and anxiety surged worldwide. For older adults especially, the sudden withdrawal of social contact proved damaging. Even virtual connection, while better than none, couldn’t replace the benefits of in-person interaction. The lesson was clear: social engagement isn’t optional for wellbeing—it’s essential.
Are Social Needs Same For Everyone?
Not everyone needs the same amount of socializing to feel fulfilled. Extroverts may thrive on daily interaction with large groups, while introverts may prefer only a few hours with close companions. What matters most is not the number of interactions but their quality and consistency. Both groups—introverted and extroverted require some level of social contact to maintain cognitive and emotional health.
Even solitary-seeming activities often include subtle forms of social connection. Watching TV shows or movies involves empathizing with characters. Browsing social media sparks feelings of comparison, judgment, or admiration—all forms of social processing in the brain. Humans are constantly scanning and responding to other humans, whether in person or virtually.
How to Stay Social at Any Age?
For older adults, socializing may take intentional effort. Retirement, loss of loved ones, or health issues can reduce opportunities for connection. But small changes make a big difference. Scheduling regular calls with family, joining local clubs, volunteering, or simply sharing meals with neighbors can reintroduce the richness of human interaction. For younger adults, staying connected is equally important for long-term brain health and resilience.
Even if mobility or geography make in-person gatherings difficult, technology can help. Video chats, online group activities, and community forums provide meaningful interaction. But experts agree that whenever possible, face-to-face connection has the strongest impact.
Think of social activity as preventive medicine. Just as you wouldn’t skip your daily walk or balanced meals, regular interaction should be built into your routine. It keeps the brain active, the body healthier, and the spirit lifted. For older adults in particular, it may even add years of life.
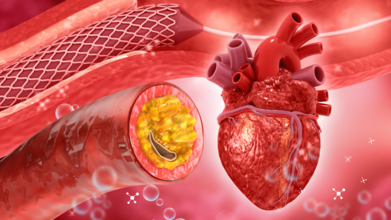
Do You Have A 'Fatty Heart'? Here's How To Tell And Changes That Can Save Your Life
Credits: iStock
The human heart is a remarkable organ. It beats over 100,000 times a day, pumping blood and oxygen through a vast network of vessels that keep us alive. Scientists are constantly uncovering new insights into its function, and one of the more recent discoveries gaining attention is something called “fatty heart.”
The idea that fat can accumulate around the heart is surprising to many. Most people are familiar with belly fat or the pinchable fat just under the skin. But the fact that fat can wrap itself around the heart, interfere with its rhythm, and silently raise the risk of life-threatening conditions is less widely known. Understanding what fatty heart is, how it develops, and what it means for long-term health is key to prevention and early intervention.
What Is Fatty Heart?
Everyone has some amount of fat around their heart. Known as pericardial fat, this tissue acts as a cushion, a source of energy, and even a thermal insulator. In healthy amounts, it supports the cardiovascular system. The problem begins when this fat becomes excessive.
The fat that sits closest to the heart muscle is called epicardial adipose tissue (EAT). Researchers describe it as both protective and potentially harmful. In newborns and healthy adults, EAT provides energy reserves and shields the coronary arteries. But when too much accumulates, it transforms from a neutral tissue into a biologically active one, releasing inflammatory molecules that can contribute to atherosclerosis (plaque buildup), oxidative stress, and ultimately heart disease.
Can You Have Fatty Heart If You’re Slim?
A common misconception is that fatty heart only affects people with obesity. That isn’t true. Research shows even lean individuals can have dangerous levels of heart fat.
A study published in the Journal of the American College of Cardiology found that about 10% of participants with a BMI under 25 still carried excess pericardial fat. The risk rose sharply with weight, 29% of those overweight and 55% of obese participants had high levels. Importantly, regardless of body size, the more fat wrapped around the heart, the higher the risk of heart failure.
This means someone with a normal BMI can still silently harbor significant cardiovascular risk, which makes regular monitoring and lifestyle habits essential.
What Is The Link Between Heart Fat and Heart Disease?
The connection between fatty heart and cardiovascular disease is now well established. A systematic review published in Circulation: Cardiovascular Imaging examined 29 studies with more than 19,000 participants. It found that increased EAT—whether measured through ultrasound or CT scans—was strongly associated with major heart complications, including heart attacks, ischemic strokes, heart failure, and atrial fibrillation (Afib).
Studies reveal that epicardial fat behaves differently than the fat under your skin. It is biologically active, releasing inflammatory substances and damaging the endothelium (the thin lining of blood vessels). It also generates reactive oxygen molecules, which, if not neutralized by antioxidants, contribute to oxidative stress—a process that damages cells and accelerates cardiovascular decline.
According to a 2022 review in Nature Reviews Cardiology, nearly 2,000 studies over the past two decades have reinforced these findings. The verdict is clear: fatty heart is not just an incidental observation—it’s a critical risk factor.
What Causes Fatty Heart?
Dr. Anil Mishra, a cardiologist at BM Birla Heart Hospital, notes that fatty heart is often the outcome of modern lifestyles combined with underlying health conditions. “While most people are familiar with fatty liver disease, very few realize that fat can also accumulate around the heart. This silent but dangerous problem can increase the risk of heart failure, arrhythmia, and other life-threatening complications,” he explains.
Some of the most significant causes include:
Obesity – Excess body fat is a major driver, triggering inflammation and even fibrosis within the heart muscle. It also disrupts rhythm, frequently causing atrial fibrillation.
Diabetes – Metabolic disturbances in type 2 diabetes accelerate fat deposition around the heart.
High cholesterol – Elevated LDL cholesterol leads to fatty buildup in both arteries and heart tissue.
Excess alcohol consumption – Heavy drinking harms both liver and heart, fueling fatty deposits.
Sedentary lifestyle – Limited activity reduces calorie burning, allowing fat to settle around critical organs.
Genetics – A family history of cardiovascular disease can predispose someone to this condition.
Symptoms of Fatty Liver That Should Not Be Ignored
In its early stages, fatty heart is often silent. Many people discover it only through imaging tests performed for other reasons. But as it advances, symptoms may appear, including:
- Persistent fatigue and weakness due to reduced pumping efficiency.
- Chest discomfort or heaviness as fat presses against heart structures.
- Shortness of breath, even with light exertion like walking upstairs.
- Irregular heartbeat or palpitations, sometimes due to atrial fibrillation.
- Swelling in legs or abdomen, a sign of poor circulation and fluid buildup.
- Difficulty breathing at night while lying flat.
Dr. Mishra emphasizes that ignoring these warning signs can delay diagnosis. “If you notice unexplained fatigue, breathlessness, or palpitations, consult a doctor without delay. Early intervention can make all the difference,” he advises.
How to Stay Protected?
The good news is that fatty heart is not an inevitable condition, and like many cardiovascular risks, it can be reduced through consistent lifestyle choices and timely medical care. Staying physically active is one of the most effective ways to protect the heart, as regular exercise helps burn visceral fat, including epicardial fat. Activities such as walking, swimming, cycling, or strength training for at least 150 minutes a week can make a measurable difference.
A heart-healthy diet is equally important—one that emphasizes whole grains, vegetables, fruits, lean proteins, and healthy fats like olive oil and nuts, while limiting processed foods, added sugars, and saturated fats.
Managing chronic conditions such as high blood pressure, diabetes, and elevated cholesterol through medication and lifestyle adjustments is also essential to lower the risk.
Limiting alcohol intake plays a role too, since heavy drinking promotes fat accumulation around both the liver and the heart, making moderation—or abstinence if advised—a key preventive step.
Maintaining a healthy weight can further reduce the burden of fat around the heart; even modest weight loss has been shown to decrease epicardial fat levels.
Finally, scheduling regular medical checkups is crucial, as imaging techniques like CT scans or echocardiography can detect excess heart fat early, well before noticeable symptoms begin. Together, these steps can significantly improve long-term heart health and reduce the risks associated with fatty heart.
Fatty heart is a silent but serious condition that challenges the traditional way we think about fat and cardiovascular risk. It can strike lean or overweight individuals alike, and it is strongly tied to heart disease, arrhythmia, and failure.
What this really means is that taking care of your heart requires more than watching the scale. It requires attention to lifestyle, awareness of symptoms, and proactive medical care. With exercise, a balanced diet, and timely screenings, you can protect your heart from this hidden risk and give it the resilience it needs to keep beating strong for years to come.
© 2024 Bennett, Coleman & Company Limited

