- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Explained: Why Some Women Start Experiencing Joint Pain As They Approach Menopause

Menopause marks the end of a woman's reproductive years, signaling the permanently stopping of menstrual periods and that they will no longer be able to conceive. It's a natural biological process, not a disease, and a normal part of aging. The period leading up to menopause is known as the menopausal transition or perimenopause.
According to the National Institute of Aging while some women experience menopause with minimal or no symptoms, others may face a range of challenges. Common menopausal symptoms include hot flashes, night sweats, sleep disturbances, joint and muscle pain, decreased libido, mood swings, difficulty concentrating, and memory lapses. If these symptoms significantly impact your quality of life, it's essential to consult a healthcare provider to discuss potential lifestyle modifications or medical treatments.
Some women experience a great deal of joint pain, to the point that their normal active lifestyle gets affected and makes even regular tasks difficult to do! And this is known as the musculoskeletal syndrome of menopause.
How does Menopause Affect Bone Health?
According to the Lancet Rheumatology it is an undeniable fact that gender plays a significant role in the development of certain rheumatic conditions, particularly those affecting the musculoskeletal system. Women, in particular, often experience increased joint and muscle pain, especially during menopause. This suggests that there is a strong link between sex hormones and pain sensitivity.
While there's growing evidence that any deficiencies in sex hormones can influence you getting of musculoskeletal diseases or it becoming worse over time, the specific mechanisms behind this relationship remain unclear. The potential benefits of hormone replacement therapy in removing these symptoms are still being explored, particularly in terms of prevention and treatment of established conditions.
In a research paper published in the National Library of Medicine more than 70% women who have entered their menopause phase expereience muscoloskeletal symptoms while 25% of those women will be disabled during the transition to perimenopause to postmenopause.
Will Hormone Replacement Therapy Work?
According to the North American Menopause Society’s position statement on hormone therapy experts believe that the decline in estrogen during menopause plays a significant role in the development of musculoskeletal symptoms. Estrogen helps regulate inflammation, and its decrease can contribute to increased joint pain and muscle weakness. Hormone therapy, particularly estrogen therapy, has been suggested as a potential treatment for the musculoskeletal syndrome of menopause. However, more research is needed to fully understand its benefits and risks, as well as to identify the optimal dosage and duration of treatment.
How Can You Manage These Symptoms?
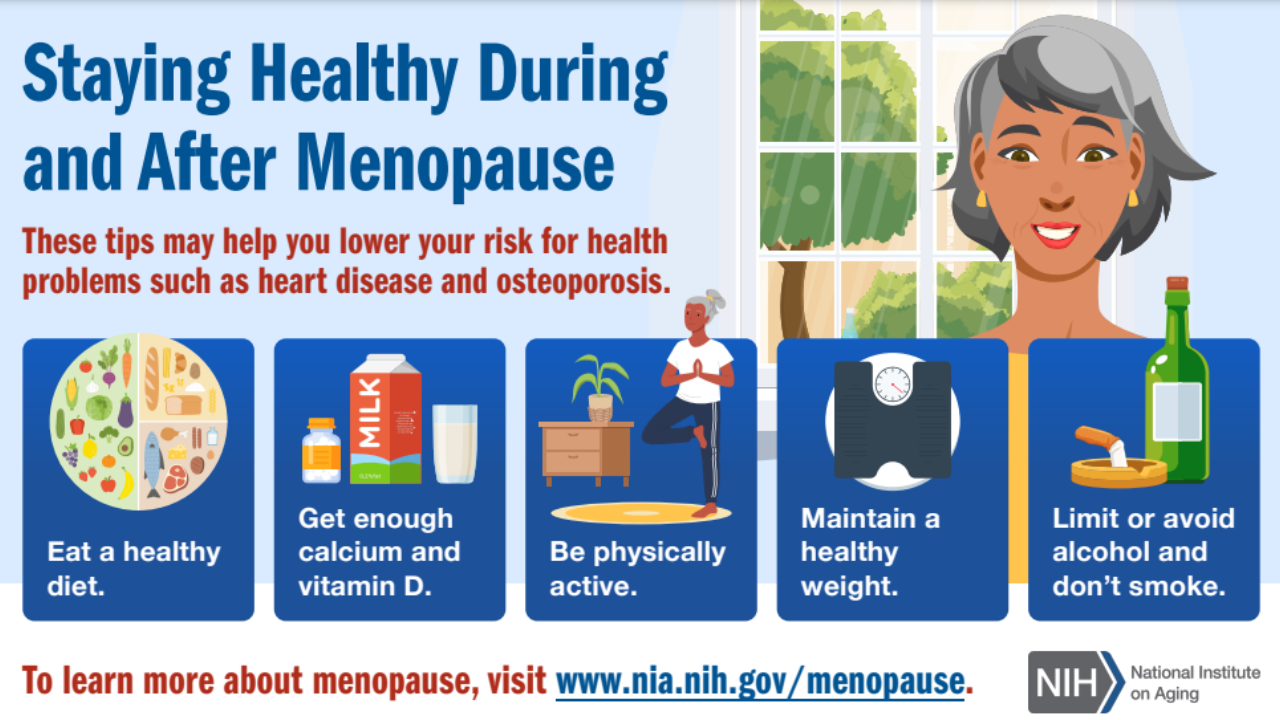
While research continues, women can take several steps to manage menopausal muscle and joint pain. A well-balanced diet rich in anti-inflammatory foods, such as the Mediterranean diet, can help reduce inflammation and alleviate symptoms. Increasing protein intake is essential for maintaining muscle mass, while adequate calcium and vitamin D3 intake are crucial for bone health. Regular physical activity, including both aerobic exercise and strength training, can help improve muscle strength, bone density, and overall fitness. Incorporating balance exercises and stretching into your routine can further enhance mobility and reduce the risk of falls.
This Year, Doctor's Day Reminded That Doctors Too Are Humans And Can Get Emotionally Exhausted

Credits: Canva
This year's Doctor's Day was a reminder to all that doctor's too are human. The theme specifically focused on healing the healers, emphasizing on the need for people to recognize doctor's struggle and treat them with empathy and sympathy.
No Lines Between Personal And Professional Life
Health and Me had earlier reported on how doctors, even when they are not at work receive work questions all the time. In a previous interview with Health and Me, Dr Guru N Reddy, a senior gastroenterologist, shared, “I didn’t spend time with my family when my kids were growing up. My work always came first and then came my family.” He also shared that how whenever he is gone for a gathering, it turns into an unofficial consultation desk. “Can I quickly show you this report?” “There’s this pain that won’t go, can you suggest something?” These are the questions he is faced with even at family events.
All such scenarios will undoubtedly make a doctor feel overwhelmed. In fact, a survey conducted by Medtalks, a doctor engagement platform, revealed that doctors are burdened by growing mental and emotional burden.
Also Read: Healthier Popcorn Alternatives You Can Try For Your July 4 Movie Nights
The survey, though small scale, conducted among 200 doctors across public and private health care, revealed an important issue. It found that 74% of respondents felt emotionally exhausted on a weekly or even on a daily basis. This survey also highlighted the depth of burnout and chronic stress in the medical profession.
Many doctors also agreed that even after their work hours, they were still entertained with questions related to their patients health through WhatsApp. The data revealed that over 83% of doctors felt that they were under constant stress as their patients continued to contact them through WhatsApp, phone calls, and digital messages, with many asking them for urgent queries. This round-the-check communication has blurred personal and professional boundaries, which has disassociated doctors from their own families.
Also Read: Measles Outbreak Update: Kentucky Confirms Its First Case
Looming Fear Of Threat And Violence On Doctors
The survey also found that threat and violence against doctors were a major source of stress and concern. Indian Medical Association (IMA) President, Dr Dilip Bhanushali, in an earlier interview with Health and Me had said, "Violence against doctors is not rare—it’s routine."
He further added: “We’ve seen mobs arrive with kerosene, petrol, even swords, burning down hospitals. There was a law during COVID promising seven years imprisonment and non-bailable warrants for attacks on doctors, but it hasn’t been enforced. Most states still have weak three-year, bailable punishments.”
He also pointed towards the RG Kar Medical College’s case where a female postgraduate trainee doctor was raped and murdered and her body was found in a seminar room on campus. Doctors across the nation went on a strike, demanding justice. “But we cannot go to the roads and do strikes every time. Despite it all, we uphold our Hippocratic oath.”
The survey too echoed the same feelings, where many respondents admitted that this fear has directly influenced their approach to diagnosis, communication, and decision-making. Doctors are now acting more defensively.
The strain on doctors is intensified by mounting administrative duties, fear of legal action, limited institutional support, and rising expectations to deliver flawless outcomes.
Over one-third of doctors reported working more than 60 hours a week, while only 17 percent are able to take a full, uninterrupted day off on a regular basis. Most respondents said they receive minimal support in coping with these demands. Strikingly, just 14 percent felt the current healthcare system allows them to prioritise their own wellbeing, whereas 52 percent said it does not.
Later Dinners Are A Recipe For Disaster - Study Finds The Best Time To Eat Dinner For Health

When it comes to dinner, many of us focus on what we eat, aiming for healthy and delicious food. But we often don't think about when we eat it, squeezing dinner in whenever our busy schedules allow. However, a growing amount of research suggests that when you eat can be just as important for your health as what you eat. And it seems that eating dinner earlier might be the way to go.
What's the Best Time for Dinner?
Scientists haven't found one single "perfect" dinner time, but it's generally best to avoid eating late for your metabolism. Try to finish dinner at least two hours before you go to bed, and ideally even longer. According to a 2024 study published in the JAMA Network Open, good goal is to eat dinner sometime between 5 p.m. and 7 p.m.
Of course, life happens, and sometimes you'll have to eat later. If it's just occasionally, don't worry too much. Just try not to eat a very large meal right before bed. In fact, research suggests that dinner shouldn't be your biggest meal of the day, which is different from what many Americans are used to. Instead, try to eat most of your calories earlier in the day, around when you wake up or in the middle of the day.
Why Does When You Eat Dinner Matter?
Our bodies have internal "clocks" that manage how we function throughout the day. This means that the exact same meal can affect your body differently depending on the time you eat it.
For instance, one study found that when healthy young adults ate the same dinner at 10 p.m. instead of 6 p.m., their blood sugar levels went higher and their bodies processed fat less effectively. Late dinners can have this impact even if you're not eating right before bed.
One reason for this could be melatonin, a hormone your body releases at night to help you sleep. As melatonin levels rise, it seems to make it harder for your body to control blood sugar, leading to bigger and longer-lasting spikes after a late meal. Research also shows that eating dinner late can make you hungrier, cause your body to burn fewer calories, and even lead to changes in your body that promote fat gain.
How Late Dinners Affect Your Health
While many studies on meal timing are done in controlled lab settings, the findings suggest that regularly eating dinner late could increase your risk for health problems like type 2 diabetes and obesity. Many studies have already shown this connection. On the other hand, eating more of your calories earlier in the day seems to help with weight loss and improve signs of good metabolic health.
It's not just about metabolism either. Other research suggests that people who stop eating after 6 p.m. tend to get more sleep than those who eat until midnight. There's even a serious study from 2024 that links late eating to a higher risk of death. So, the general advice is clear: for most people, it's best to limit how much food you eat during the nighttime hours.
Tips for Eating Dinner Earlier
If you're used to eating late, changing your routine can be tough. To make the switch easier, start by making changes earlier in your day. If you often skip breakfast and grab a quick, small lunch, you'll likely be very hungry by evening. So, make sure you eat good, hearty meals earlier in the day that include plenty of protein, fiber, and healthy fats. This will help you feel less hungry at night.
Some people also find it helpful to set a specific "cut-off time" after which they stop eating, rather than just vaguely aiming for an earlier dinner. If you try this, it's okay to start small. Begin by closing the kitchen just 30 minutes before bedtime, then extend it to an hour, and so on. The key is to start where you are and build up gradually.
Australian Man Dies From An 'Extremely Rare' Rabies Like Infection After A Bat Bite

Credits: Canva
An Australian man in his 50s has died after contracting Australian bat lyssavirus (ABLV), a rare but deadly virus closely related to rabies. The man, who lived in northern New South Wales, was bitten by a bat several months ago and succumbed to the infection this week after being hospitaliszed in critical condition.
In a statement released on Thursday, NSW Health confirmed the fatality and extended condolences: “We express our sincere condolences to the man's family and friends for their tragic loss. While it is extremely rare to see a case of Australian bat lyssavirus, there is no effective treatment for it.”
What Is Australian Bat Lyssavirus?
First identified in 1996, Australian bat lyssavirus belongs to the Lyssavirus genus, the same family as the classical rabies virus (RABV). Like its more globally prevalent cousin, ABLV causes a fatal form of viral encephalomyelitis—an inflammation of the brain and spinal cord. Once symptoms develop, there is no known cure or treatment.
Transmission occurs when the saliva of an infected bat enters the body through a bite or scratch. According to NSW Health, any bat in Australia—regardless of species—could potentially carry the virus. In this case, officials have not yet identified the exact bat species responsible for the infection.
Early Symptoms Often Misleading
The early symptoms of ABLV infection mimic those of the flu, including headache, fever, and fatigue, which can delay diagnosis. However, the disease rapidly progresses to paralysis, delirium, convulsions, and ultimately death.
Symptoms may appear days, weeks, or even years after exposure, adding another layer of complexity to diagnosis and response.
This recent death is only the fourth recorded human case of ABLV infection in Australia, and tragically, all four have been fatal.
A Preventable Tragedy
While the disease has no cure, prompt medical treatment after exposure can prevent infection. NSW Health strongly urges the public to avoid all contact with bats. In the event of a bite or scratch, the following steps should be taken immediately:
- Wash the wound thoroughly with soap and water for at least 15 minutes
- Apply an antiseptic with antiviral action
- Seek urgent medical attention for administration of rabies immunoglobulin and a rabies vaccine series
Dr. Jeremy McAnulty, Director of Health Protection at NSW Health, emphasized the importance of public awareness: “No matter how minor the scratch or bite may seem, immediate treatment is essential. Rabies vaccines are extremely effective when administered quickly.”
The Broader Context: Lyssaviruses and Rabies Risk
Australian bat lyssavirus may be rare, but its relation to rabies—one of the deadliest infectious diseases globally—makes it especially concerning.
According to a 2021 study titled "Rabies Infection: An Overview of Lyssavirus-Host Protein Interactions," lyssaviruses are negative-sense, single-stranded RNA viruses known to infect mammals and cause fatal encephalomyelitis. Despite differences in geography and host species, illnesses caused by rabies virus (RABV) and other lyssaviruses are virtually indistinguishable once symptoms appear.
Worldwide, rabies still causes approximately 60,000 deaths annually, mostly in Asia and Africa. The fatality rate of clinical rabies—once symptoms begin—is nearly 100%, underscoring the importance of pre- and post-exposure prophylaxis.
Flying Foxes and Microbats Under Scrutiny
ABLV has been found in multiple Australian bat species, particularly flying foxes and insect-eating microbats. These animals often come into contact with humans, especially in urban or suburban environments where bats may roost or forage.
Despite the important ecological role bats play—as pollinators, pest controllers, and seed dispersers—public health officials continue to stress no direct handling of bats by untrained individuals. Wildlife carers and veterinarians are advised to wear protective gear and be vaccinated against rabies.
Public Health Measures Going Forward
This latest case serves as a stark reminder of the persistent, though rare, risk that Australian bat lyssavirus poses to human health. NSW Health is reinforcing education campaigns and urging any bat encounters to be reported immediately.
Authorities continue to collaborate with wildlife and disease surveillance networks to monitor ABLV across bat populations and ensure rapid response to potential exposures.
In closing, NSW Health reiterated, “Although Australian bat lyssavirus cases are extremely rare, they are always fatal without timely treatment. Awareness and early action can mean the difference between life and death.”
© 2024 Bennett, Coleman & Company Limited

