- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Goosebumps Aren’t Just About Cold, Then What Are They?

Image Credit: Canva
They're known by many names—goose pimples, goosebumps, or even cutis anserine, which is what doctors call them—but the effect is always the same: small bumps on your skin when you're cold, emotional, or even frightened. They might be small, but goosebumps are a fascinating leftover from our ancient history, a biological response that binds us to the animal kingdom in more than one way. But why do they happen, and are they useful for anything? Let's explore the science behind goosebumps.
Each and every hair in your body is connected to it an infinitesimally small muscle called the arrector pili. Activating theses muscles tightens them up and lifts the associated hair perpendicularly out from the hair shaft, in turn causing minute bulges overlying the attached hairs. Activation is caused through stimulation of nerves activated by these special muscles leading ultimately to release by the brain controlling the system.
The nerves surrounding the arrector pili send electrical messages that instruct these muscles to tense up. The process is not voluntary, and you can't decide when the goosebumps will occur. But what's behind this action?
Why We Get Goosebumps?
A Chilling Reaction to Cold
The most typical cause of goosebumps is cold exposure. When the body senses a decrease in temperature, the sympathetic nervous system is triggered, making the arrector pili muscles contract. This will lift body hair, which, in thick-furred animals, traps a layer of warm air. In humans, though, our fairly thin body hair makes this purpose largely ineffective.
Fear and the Fight-or-Flight Response
Ever felt your hair stand on end when you hear something creepy in the dark? That's your fight-or-flight response activating. When we sense danger, the body releases a hormone called adrenaline, getting us ready for action. In animals, this makes them look bigger and more formidable to predators. Humans don't have sufficient body hair for this to work, but the physiological reaction is still there.
Emotional and Aesthetic Triggers
Goosebumps are not just reserved for fear or cold; they also happen when we feel strong emotions. Whether it is listening to a moving piece of music, seeing a moving moment, or feeling intense nostalgia, goosebumps tend to follow intense emotional experiences. This response is believed to be associated with the reward system of the brain, releasing dopamine when we feel something intensely moving.
Sexual Arousal and Excitement
Another less familiar cause of goosebumps is sexual excitement. Like the physical responses of blushing or increased heart rate, goosebumps can occur as a reaction to increased emotional or physical stimulation. This once again relates to the autonomic nervous system, which controls involuntary body responses.
Are Goosebumps an Evolutionary Leftover or Still Functional?
For animals, the advantage of piloerection is obvious—it prevents body heat from escaping and is a defense mechanism against predators. But for us, goosebumps are a vestigial trait, much like the tailbone or wisdom teeth. Without fur, do goosebumps have any functional purpose now?
Surprisingly, new studies indicate that goosebumps might be involved in hair growth. A study in the journal Cell discovered that nerves that cause goosebumps are entangled with hair follicle stem cells. When these nerves stimulate the arrector pili muscles, they also stimulate hair follicle stem cells, which could encourage hair regeneration. Although this process is more applicable in hairy animals, it presents interesting possibilities for hair growth therapies in humans.
Is There A Reason Why You Should You Be Worried?
Goosebumps are usually harmless in most cases. But in some rare cases, they can be indicative of underlying medical conditions, which include:
Temporal Lobe Epilepsy: Certain seizures can cause a condition called piloerection seizures, which cause repeated episodes of goosebumps.
Autonomic Nervous System Disorders: Certain disorders of the autonomic nervous system can lead to abnormal goosebump reactions.
Opiate Withdrawal: Goosebumps are frequent in heroin or opioid withdrawal, leading to the expression "quitting cold turkey," as the bumps have the appearance of a plucked turkey.
If you observe too much or chronic goosebumps without a clear cause, it might be a good idea to see a medical professional.
Since goosebumps no longer play a meaningful survival role for humans, it's possible that they might slowly disappear over the course of evolutionary time, as other vestigial characteristics have. But with new evidence connecting goosebumps to hair growth, they could be more important than we originally thought.
Ramadan Fasting: Avoid Excess Salt And Caffeine To Boost Kidney, Prostate Health, Say Experts

Credit: Canva
Dehydration is a serious concern for people fasting during the month-long Ramadan period, and can severely impact kidney and prostate health. Experts suggested that avoiding excess salt and caffeine can help.
While Ramadan fasting is generally safe for people with early-stage chronic kidney disease (CKD), maintaining adequate hydration between iftar and sehri -- the two important meals each day for faithful observing the fasting -- is of significant importance.
Dehydration can lead to acute kidney injury and electrolyte imbalances for individuals with advanced CKD. As prolonged fasting hours -- more than 12 hours a day -- urine becomes concentrated, increasing the risk for kidney stones and Urinary Tract infections (UTIs).
For men with prostate problems, fasting during Ramadan can pose challenges, such as Benign Prostatic Hyperplasia (BPH) or an enlarged prostate, primarily due to dehydration.
“As a practicing urologist and kidney transplant surgeon in India, I often notice a rise in kidney stone pain and urinary infections during Ramzan. When patients fast for long hours -- especially in our warm climate -- urine becomes highly concentrated. That increases the risk of stones and UTIs. Men with prostate enlargement sometimes report worsening urinary flow because they consciously reduce fluid intake,” Dr. Pankaj Panwar, Additional Director, Urology, Fortis Escorts Okhla, New Delhi, told HealthandMe.
The doctor advised people “to hydrate strategically between Iftar and Sehri, avoid excess salt and caffeine”.
How Excess Salt And Caffeine Impact Ramadan Fasting
Consuming high-sodium foods such as processed meats, pickles, salty snacks, and fast food during iftar or sehri can increase thirst and dehydration.
High salt intake forces the body to pull water from cells to dilute the sodium, leading to severe thirst. It can also lead to bloating.
Similarly, caffeine in coffee, tea, chocolate, and energy drinks can be diuretic and cause the body to lose fluids and salts through increased urination. Particularly, drinking coffee or tea at sehri -- the pre-dawn meal -- can lead to faster dehydration during the day.
Caffeine consumption, especially late in the evening, can also interfere with sleep, making it harder to wake up for sehri.
“Ramzan is a sacred month of fasting, but prolonged abstinence from water, especially in hot climates, can increase dehydration risk. Concentrated urine puts stress on the kidneys and may worsen kidney stones or trigger urinary tract infections,” Dr. Mangesh Patil, Urologist at Saifee Hospital, Mumbai, told HealthandMe.
Dehydration during Ramadan fasting can lead to symptoms like headaches, extreme thirst, fatigue, and dizziness. But in case of severe dizziness, fever, confusion, or blurred vision, the experts warned of immediate medical help.
“Do not ignore warning signs like flank pain, fever, or difficulty passing urine. A little planning can prevent an emergency hospital visit,” Panwar said.
Patil said warning signs include severe flank pain, burning urination, fever, vomiting, blood in urine, or reduced urine output. Men with Benign Prostatic Hyperplasia may notice worsening urinary symptoms.
Tips To Prevent Complications
- Drink 2-3 liters of water between iftar and sehri
- Include water-rich fruits
- Avoid excess salt and caffeine
- Individuals with kidney disease, stones, UTIs, or prostate issues should consult their doctor before fasting.
How Age And Genetics Can Determine Antibodies Production In Your Body
Credit: Canva
Ever wondered how your body generates antibodies in the face of a virus attack? A new study by French researchers showed that our age, biological sex, and human genetic factors can determine our immunity levels.
The human body, when exposed to a virus, defends itself by producing molecules called antibodies. Their main function is to identify pathogens and kill them.
Scientists from the Institut Pasteur, the CNRS, and the Collège de France noted that these factors not only boost the quantity of antibodies produced in the body but also determine the specific viral regions to target.
The February 2026 study, published in the journal Nature Immunology, can pave the way for the development of personalized treatments, especially for individuals who are most vulnerable to infection.
"This study provides a detailed, integrated view of how age, sex, and human genetics shape the antibody response," said Lluis Quintana-Murci, Head of the Human Evolutionary Genetics laboratory at the Institut Pasteur.
"It shows that these factors even determine which specific regions of a given virus are targeted by antibodies, with important implications for vaccine and therapeutic design," Quintana-Murci added.
How Age And Sex Influence Immunity
The findings revealed that individuals produce antibodies that target different parts of the virus when attacked by the same virus. Age was identified as the dominant factor influencing antibody production. The team noted that more than half of the antibody repertoire varies depending on age.
Further, some antibodies were found to increase with age, while others decreased. This was seen particularly in the case of influenza H1N1 and H3N2 viruses.
In young adults, the antibodies mainly targeted a part of the viral surface protein known as hemagglutinin (HA), which evolves rapidly. In older individuals, it focused on a more stable region of the same protein known as the stalk domain.
Women were also found to produce more antibodies against HA. On the other hand, men tended to target other viral proteins (NP and M1), despite comparable vaccination rates between the two sexes.
How Human Genetics Shape Antibody Production
The team identified mutations in genomic regions known to encode the immunoglobulin repertoire. These variants determine which genes are used to produce antibodies.
Using an African cohort, the study revealed population disparities in terms of the molecular targets of their antibody repertoires.
In the case of Epstein-Barr virus (EBV), antibodies were found to recognize different viral proteins depending on the geographical and epidemiological context.
This difference can be explained by the level of exposure -- Africans are more exposed to a particular strain of EBV in which the protein EBNA-4 is the primary antibody target.
How Was The Study Conducted?
The research is based on data from the Milieu Intérieur cohort, launched 15 years ago to study variations in the immune response in 1,000 healthy individuals.
Using an innovative sequencing technology, the scientists analyzed blood plasma samples to measure antibody responses against more than 90,000 fragments of viral proteins, covering a large number of viruses responsible for infections such as influenza, respiratory infections, gastroenteritis, and herpesvirus infections.
Epstein Files: Post-mortem Notes And New Documents Shed Light On Late Sex Offender's Death
Epstein Files: After the Department of Justice (DOJ) released more files on the late sex offender and financer Jeffrey Epstein, previously unseen photographs, including medical details and a detailed timeline of his final weeks in custody have resurfaced. All of this new information has added fresh scrutiny to the case.
A 23-page long document, labelled unclassified titled Jefferey Epstein Death Investigation was prepared by the New York field officer of the FBI. The material has been examined by BBC Verify and was reported to contain close-up images of Epstein's body, notes from his post-mortem examination and psychological observations that were recorded shortly before his death in August 2019.
As per BBC, the photographs included detailed views of injuries to Epstein's neck and show medics attempting to resuscitation after he was found unresponsive in his jail cell. As per the timestamps visible in the files, the images were taken at 06:40 local time on 10 August 2019, almost 16 minutes after a prison staff discovered him.
As per the DOJ's Office of the Inspector General's review report released in June 2023, on August 10 at 6.30am, two SHU staff on duty CO Tova Noel and Material Handler Michael Thomas delivered breakfast to inmates, when Noel was delivering breakfast from the food slot of the door to Epstein's SHU tier, there was no response. Thomas unlocked the door and saw Epstein hanged. The review report mentions that he immediately "yelled for Noel to get help and call for a medical emergency". According to Noel, within seconds of Thomas calling out for the clutter she hit the body alarm, which is a button on an MCC staff member's radio that is used to signal distress or an emergency. Noel also recalled Thomas saying, "Breathe, Epstein, breathe." As per Noel, when she saw Epstein, he looked "blue and did not have a shirt or anything around his neck".
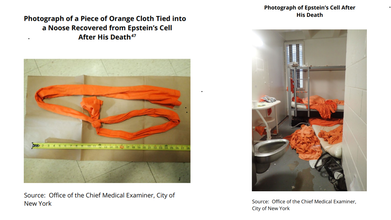
Read: Epstein Files Photos Show A Bottle Of Phenazopyridine, Why We Think This UTI Medication Was There
As per Thomas, when he entered Epstein's cell, he had an orange string, from a sheet or a shirt, around his neck that was tied t the top portion of the bunkbed. The review report notes: "Epstein was suspended from the top bunk in a near-seated position, with his buttocks approximately 1 inch to 1 inch and a half off the floor." As per Thomas, he immediately ripped the orange string from the bunkbed and Epstein's buttocks dropped to the ground, and lowered him to begin chest compressions until staff arrived.
As per the BBC reports, the location is not explicitly stated in the documents, but records indicate Epstein had already been transported to hospital at 06:39, where he was later pronounced dead, suggesting the images were likely taken there.
Some of the photographs show a tag attached to his hand with his name and date of death. In several images, however, his first name appears misspelled as “Jeffery”.
Epstein Files: Post-Mortem Of Jeffrey Epstein And Custody Timeline

The investigation file incorporates sections of an 89-page post-mortem report compiled jointly by the Department of Justice and New York’s Office of Chief Medical Examiner. Among the medical findings were scans documenting fractures in the thyroid cartilage of Epstein’s neck.
BBC Verify said it conducted reverse image searches and “could not find earlier versions” of the photos online before their recent release, indicating they had not previously circulated publicly.
The report also reconstructs Epstein’s detention inside the Metropolitan Correctional Center from his arrest on 6 July 2019 on federal sex-trafficking charges to his death five weeks later.
According to the timeline, Epstein was placed on suicide watch after a 23 July incident in which he was found injured in his cell. At the time, he claimed his cellmate — Nicholas Tartaglione — had attacked him.
Epstein Files: Jeffrey Epstein's Psychological Assessment Before His Death

The following day, during a psychological assessment, Epstein denied wanting to harm himself. BBC reported the document states he said he had “no interest in killing myself” and that it “would be crazy” to do so. Two days later, notes record him saying he was “too vested in my case” and wanted to return to his life.
Despite that, prison officials had recommended he not be housed alone and that guards perform checks every 30 minutes, including unannounced rounds.
The newly released records outline several security lapses the night before Epstein died.
His cellmate had been transferred out the previous day, leaving him alone. Prison logs show guards failed to conduct scheduled checks at 03:00 and 05:00, and the unit’s camera system was not functioning. Staff later discovered his body during a morning inspection.
The files also include two versions of the same FBI report: a full 23-page unredacted copy and a shorter 17-page redacted version that omits the psychological report and detention timeline. The reason for the dual publication has not been explained.
The Department of Justice has been contacted for comment, while the FBI declined to respond, reported BBC.
The release of the material does not change the official ruling of suicide, but its level of detail, particularly the photographs, mental-health notes and security failures — is likely to reignite debate over the circumstances surrounding Epstein’s death.
© 2024 Bennett, Coleman & Company Limited

