- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
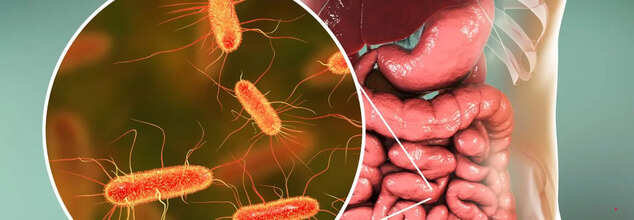
How Does Your Gut Microbiome Impact Your Overall Health?
Credit: Canva
Your body hosts trillions of bacteria, viruses, and fungi, collectively known as the microbiome. While some bacteria are linked to disease, many play essential roles in supporting your immune system, heart health, weight management, and overall well-being. This article delves into the significance of the gut microbiome and its impact on health.
What Is Gut Microbiome?
Microorganisms, or microbes, reside in various parts of your body, but the majority are concentrated in the intestines, particularly in the cecum, a part of the large intestine. This collection of microbes is referred to as the gut microbiome.Interestingly, bacterial cells outnumber human cells in the body, with approximately 40 trillion bacterial cells compared to 30 trillion human cells. With up to 1,000 species of bacteria present in the gut, each plays a distinct role. While most bacteria contribute positively to health, some can be harmful. Together, these microbes weigh around 1–2 kilograms, functioning almost like an additional organ essential for overall well-being.
How Does Gut Microbiome Influence Your Health?
The relationship between humans and microbes has evolved over millions of years, with the gut microbiome playing a crucial role from birth. Initial exposure to microbes occurs during birth, and some evidence suggests that exposure begins in the womb. As the microbiome diversifies, it starts influencing key bodily functions:
Digestion of breast milk: Beneficial bacteria like Bifidobacteria help break down essential sugars in breast milk, supporting infant growth.
Fiber digestion: Some bacteria process fiber into short-chain fatty acids, which contribute to gut health and reduce risks of obesity, diabetes, and heart disease.
Immune system regulation: The gut microbiome interacts with immune cells, influencing how the body responds to infections.
Brain health: Emerging research suggests a link between the gut microbiome and brain function, potentially affecting mental health and neurological processes.
Gut Microbiome And Weight Management
An imbalance between beneficial and harmful microbes, known as gut dysbiosis, may contribute to weight gain. Studies on identical twins—one with obesity and the other without—suggest that microbiome composition plays a role in body weight independent of genetics. Additionally, animal studies indicate that gut bacteria can influence weight gain, even when calorie intake remains constant.
Probiotics, beneficial bacteria found in supplements and certain foods, can help restore gut balance and support weight loss, though their effects may be modest.
Gut Health And Disease Prevention
The gut microbiome plays a vital role in preventing and managing conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Imbalances in gut bacteria may lead to bloating, cramps, and digestive issues. On the other hand, beneficial bacteria like Bifidobacteria and Lactobacilli help strengthen the intestinal lining, reducing the risk of gut-related disorders.
Impact On Heart Health
Research suggests that the gut microbiome influences heart health by affecting cholesterol levels and blood pressure. Certain harmful bacteria produce trimethylamine N-oxide (TMAO), a compound linked to blocked arteries and heart disease. However, probiotics, particularly those containing Lactobacilli, may help reduce cholesterol levels and promote cardiovascular health.
Blood Sugar Regulation And Diabetes Risk
The gut microbiome also plays a role in regulating blood sugar levels. Research on infants genetically predisposed to type 1 diabetes indicates that gut microbiome diversity declines before disease onset. Furthermore, individual variations in gut bacteria may explain why people experience different blood sugar responses to the same foods.
Connection Between Gut And Brain
The gut is physically connected to the brain through nerves, and certain bacteria help produce neurotransmitters like serotonin, which influence mood and mental health. Studies indicate that people with mental health disorders often have different gut bacteria compared to those without such conditions. Additionally, some probiotics have shown promise in alleviating symptoms of depression and anxiety.
Tips For Healthier Gut Microbiome
Maintaining a balanced gut microbiome is crucial for overall health. Here are some strategies to support gut health:
- Eat a diverse range of foods: A varied diet rich in fiber, legumes, and fruits promotes microbial diversity.
- Consume fermented foods: Yogurt, kefir, and sauerkraut contain probiotics that enhance gut health.
- Limit artificial sweeteners: Some artificial sweeteners can encourage the growth of harmful bacteria.
- Include prebiotic foods: Bananas, oats, and asparagus contain fibers that nourish beneficial bacteria.
- Breastfeed infants when possible: Breastfeeding promotes a healthier gut microbiome in babies.
- Choose whole grains: Whole grains contain fiber and beneficial compounds that support digestive health.
- Opt for a plant-based diet: Vegetarian diets may reduce inflammation and support a healthier gut microbiome.
- Consume polyphenol-rich foods: Green tea, dark chocolate, and olive oil contain compounds that foster beneficial bacteria.
- Take probiotics if needed: Probiotic supplements can help restore gut balance after disruptions, such as antibiotic use.
- Use antibiotics cautiously: While antibiotics can be life-saving, overuse can harm beneficial gut bacteria.
Autism Rates Are Similar In Men And Women, But Girls Often Mask Symptoms, Study Finds

Credits: Canva
The number of autistic women is same as the number of autistic men, but women know to hide it well, says research. A study published in the BMJ, found that while the rates of diagnosis for autistic is found among young boys and girls, rates are almost identical by the time they reach adulthood. However, these new findings have also shown that women are more likely to "mask" signs of autism in order to fit in. This is why their diagnosis is done far later.
What Did The Study Find Out?
This is the first major study to find such high levels of condition among women. Previously, diagnoses rates were four times higher among boys and men than females.
Specialists say the findings highlight the urgent need to move away from outdated stereotypes that still influence how autism is recognized and diagnosed.
The international study, led by researchers at the Karolinska Institutet in Sweden, examined autism diagnosis rates among people born in Sweden between 1985 and 2000. More than 2.7 million individuals were followed for up to 37 years, making it one of the most comprehensive studies of its kind.
By 2022, around 2.8 per cent of the population studied had been diagnosed with autism spectrum disorder. The data revealed a clear pattern. In early childhood, boys were far more likely than girls to receive an autism diagnosis. However, this gap steadily narrowed during adolescence.
By the time participants reached their late teens and early 20s, diagnosis rates among men and women were broadly similar. Researchers noted that the male to female ratio of autism diagnoses decreased over time to the point that it may no longer be distinguishable in adulthood.
A Catch-Up Effect in Adolescence
Dr Caroline Fyfe, lead author of the study from the University of Edinburgh, said autism has long been viewed as a condition that mainly affects males. While that pattern was still visible in children under 10, the picture changed rapidly during adolescence.
Read: Mattel Launches First-Ever Barbie With Autism
She explained that diagnoses among girls rose sharply in the teenage years, creating what researchers described as a female catch-up effect. By the age of 20, autism rates were almost equal between men and women. According to Dr Fyfe, this suggests late or missed diagnoses in females rather than a true biological difference between sexes.
Masking and Mental Health Misdiagnoses
Experts say one major reason for delayed diagnosis is masking. Girls and women are often more likely to imitate social behavior, maintain eye contact and suppress traits traditionally associated with autism. While this can help them fit in socially, it can also make their difficulties harder to identify in clinical settings.
Dr Judith Brown from the National Autistic Society said gender should never be a barrier to diagnosis or support. She noted that autistic women who are misdiagnosed often develop additional mental health challenges due to years without appropriate understanding or help.
She added that the exhaustion of constant masking can contribute to anxiety and depression, reinforcing the importance of recognizing autism earlier in girls.
Clinical Biases Under Scrutiny
Dr Steven Kapp, senior lecturer in psychology at the University of Portsmouth, said research has consistently shown that clinical biases play a role in under-recognizing autism in women and girls. He explained that subtler behaviors and social adaptation often lead clinicians to overlook autism in females.
A linked editorial written by a patient and advocate echoed these concerns, warning that autistic women are frequently labelled with mood or personality disorders while waiting for a correct diagnosis. As a result, many are forced to self-advocate simply to be recognized as autistic.
Experts say the findings should prompt changes in diagnostic approaches, ensuring that autistic girls and women are no longer left unseen.
The Crown Actor Clair Foy Had Parasites For 5 Years

Credits: Wikimedia Commons
Actor Claire Foy has revealed that a long, uncomfortable health struggle picked up while travelling ended up reshaping her relationship with caffeine. The Crown star, 41, said she gave up tea and coffee after discovering she had stomach parasites, an experience she described as “gross” and “absolutely rank.”
Foy shared the story during her appearance on The Table Manners Podcast with hosts Jessie and Lennie Ware on February 4, where the conversation moved from food to a period of unexplained weight loss and constant hunger.
“I kept losing weight, and I didn’t know what was going on,” she told the hosts. Despite eating regularly, she said she never felt full. “I was so hungry,” Foy recalled, adding that the situation left her confused and worried.
Diagnosis After Years of Symptoms
The actor explained that the cause was eventually traced back to stomach parasites she had picked up while travelling in Morocco. The diagnosis came after medical tests, including stool samples, which she candidly described as unpleasant but necessary.
According to Foy, doctors told her she had been carrying the parasites for around five years, a length of time she herself described as “quite a long time.” While she did not name the specific parasites, she shared one detail that stuck with her. “They travel as a pair, I got told by the doctor,” she said, reacting with visible disgust even years later.
Living with the condition took a toll on her body and routine. The ongoing symptoms pushed her to rethink how she approached treatment and daily habits, including what she consumed.
Read: 10 Signs You May Have A Parasite
Clair Foy Had Parasites For 5 Years: Why Caffeine Had to Go
It was during treatment that Foy made the decision to give up caffeine entirely. She explained that she wanted to avoid very strong antibiotics if possible and instead followed a strict diet alongside other treatments. “I basically had to go on this diet,” she said. “I didn’t want to take really hardcore antibiotics.”
As part of that process, caffeine was cut out. “I took all this gross stuff and part of that was giving up caffeine,” Foy told the hosts. At the time, it was a major shift. She admitted she had been a heavy caffeine consumer, drinking around 15 cups of tea a day along with two coffees she had carefully planned into her schedule.
A Habit That Never Came Back
Giving up caffeine was not easy, but once she did, Foy decided to stick with it. “Once you’ve given it up, it’s such a mission to give it up, that I was like, well, maybe I’ll just give it a go,” she said.
Now fully caffeine-free, she even brought her own tea bags to the podcast recording. The show is known for hosts and guests sharing food and drinks in the Ware family kitchen, making her preparation a small but telling detail of how seriously she takes the change.
Medical experts note that parasitic infections usually require medication to clear completely, often involving antiparasitic drugs and sometimes antibiotics or antifungals. In many cases, a combination of treatments is needed.
'I Went Into Chemo-induced Menopause At 37', Says Lisa Ray About Her Cancer Journey And Its Side Effects

Credits: Lisa Ray Instagram and BBC screengrab
"I went into chemo-induced menopause at 37," said Lisa Ray, a Canadian actress during an interview with BBC. She also shared the clip of the interview on her Instagram account talking about the importance of awareness about the side effects of cancer and its treatment on women. Sharing the clip on her Instagram story, she wrote "This is me in menopause. Menopause does not have one face...I went into premature chemo-induced menopause at 37."
She revealed that she had blood cancer, called Multiple Myeloma. "At that time, it was the least of my worries. I had a blood cancer called Multiple Myeloma to contend with… But after recovering, I could focus on what being in menopause suddenly at 37 would mean. And I had no one to talk to," said Lisa, now 53.
What Is Chemo-induced Menopause?
Chemotherapy do not just target cancer cells, but it can also harm healthy cells, which are fast diving. Ovaries fall into that category and thus they stop producing hormones like estrogen and progesterone, which pushes the body into sudden menopause.
This condition is called iatrogenic menopause or chemotherapy-induced ovarian failure. While it could be temporary for some people, for others, it could be permanent. Experts explain that women under 30 could see their periods return after the treatment.
Chemotherapy works by attacking cells that grow and divide rapidly. While this helps destroy cancer cells, it also affects healthy cells, such as those responsible for hair growth, which is why hair loss is a common side effect.
This process can also impact reproductive organs, including the ovaries, and disrupt hormone production. As a result, levels of estrogen and progesterone—the key hormones involved in menopause—may become imbalanced due to chemotherapy’s effects on the endocrine system.
Damage to cells and these hormonal shifts can trigger menopausal symptoms and, in some cases, cause periods to stop altogether.
For people over 40, hormone levels may already be naturally declining. In such cases, chemotherapy can accelerate a menopausal transition that has already begun.
Chemo-induced Menopause Symptoms
The symptoms are same as one experiences in natural menopause, which include:
- Hot flashes
- Night sweats
- Mood swings
- Fatigue
- Vaginal dryness
- Loss of libido
However, Lisa also points out the emotional impact, which could be intense especially for someone who is young and was not expecting to face menopause for decades. “Both menopause and disease-induced menopause have been treated with shame and silence for too long,” Lisa wrote on her Instagram post.
Chemo-induced Menopause: What Can Help?
Hormone Replacement Therapy (HRT): When considered safe and not restricted by hormone-sensitive cancers, HRT can help manage symptoms while supporting bone strength and heart health.
Non-hormonal treatments: Certain medications, including SSRIs, SNRIs, and gabapentin, may reduce hot flashes, while vaginal moisturizers and lubricants can relieve dryness.
Lifestyle changes: Staying physically active, following a calcium and vitamin D-rich diet, maintaining a healthy weight, and managing stress can significantly support overall wellbeing.
Fertility support: Options such as egg or embryo freezing before treatment, along with consultations with a fertility specialist afterward, may help preserve future parenthood possibilities.
© 2024 Bennett, Coleman & Company Limited

