- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
How Smoking And Alcohol Worsen Your Diabetes Symptoms
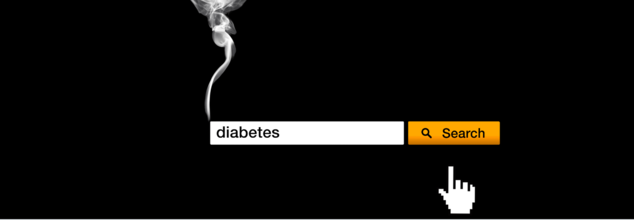
How Smoking And Alcohol Worsen Your Diabetes Symptoms
Both smoking and alcohol consumption have terrible negative effects on an individual. While in some instances, the effects of smoking may not surface promptly in an individual, the ones who suffer from any disease or who have diabetes experience worsening symptoms and more complexities within the management.
Both habits create resistance to insulin, endanger glucose control, and create long-term complications, such as cardiovascular diseases, nerve damage, and kidney failure not to be taken lightly lightly because it is all related to each other.
Smoking and Its Impact on Diabetes
Smoking rapidly increases insulin resistance; a primary characteristic feature of the disease type 2 diabetes. Nicotine and other chemicals in cigarette smoke impair the body's capacity to utilize its own insulin appropriately. Eventually, that makes it difficult to regulate blood sugar level by causing hyperglycemia (high blood sugar), one among the most common side effects of diabetes.
Of course, other lifestyle parameters such as good nourishment, working on the management of stress levels, and optimal movement therapy, which is a combination of creative workouts, calisthenics, yoga, functional exercises, and sleep cycles, play equally important roles in balancing the insulting levels.
Smoking is also another promoter of inflammation in the body, which leads to poor control of blood sugar. Chronic inflammation will damage one's blood vessels; therefore, glucose cannot easily diffuse into the cells. So, it's your duty to maintain an alkaline medium in your blood, through good food, healing fruits, cleansing help vegetables, and even nuts and seeds that act as fortifiers.
Smoking increases the production of free radicals, exacerbates oxidative stress contributing to increased causation of diabetic retinopathy, neuropathy, and nephropathy.
Moreover, smoking accelerates the heart rate and blood pressure-advantageous factors that are harmful to a patient with diabetes. People who suffer from the disease face higher risks to their cardiovascular system, and smoking hastens this risk by contributing to a condition known as atherosclerosis, or the build-up of plaque in the arteries, which eventually can contribute to heart attacks, strokes, and other effects of cardiovascular problems.
Hence, cosmic and natural elements are meant to create harmony inside the body so that the body finds itself regulating in sync.
Alcohol and Its Impact on Diabetes
Alcohol consumption may also affect blood sugar as it elevates blood sugar, especially when taken with sugars or overindulged. It is also often combined with salty foods and nuts that are also causing the blood pressure to rise. On the other hand, it can lead to hypoglycemia or low blood sugar, especially when taken on an empty stomach or together with drugs such as insulin or sulfonylureas. This is because alcohol damages the functions of the liver in releasing glucose to the blood for release, especially after heavy intake.
Therefore, they are at greater risk for both hypoglycemia and hyperglycemia, since the effects of alcohol on glucose metabolism are unpredictable. Low blood sugar because of alcohol may be dangerous and lead to symptoms such as dizziness, confusion, and even loss of consciousness. Conversely, over-ingestion of alcohol leads to levels of high blood sugar and poor diabetes control, with an increased chance of complications from DKA among those with type 1 diabetes.
Alcohol tends to induce appetite and causes overeating that can make one have unhealthy weight levels-another thing that one has to sort in managing diabetes. A large amount of taking alcohol leads to putting on too much weight, which will then increase insulin resistance.
Smoking and alcohol combined create the perfect storm of risks for the individual with diabetes. Each alone compromises insulin function, raises blood pressure, and contributes to cardiovascular issues. Together they increase risk for severe complications and make more difficult to control blood sugars.
And smoking and alcohol abuse can even worsen the symptoms of diabetes, making it complicated in management and poses grave threats to health.
Simple steps toward better control of diabetes, minimal complications, and good quality of life that improves one's Longevity, Immunity, and Vitality are quitting smoking and moderate alcohol use.
Does Bigger Penis Help You Ski Better? Why Olympians Are Injecting Hyaluronic Acid - Explained

Credits: Canva
What won't people do to get that gold. In the quest for so, Olympians re injecting hyaluronic acid in their penises. The reason? For skiing, it helps them fly better and further.
In January, a German newspaper, Bild reported that jumpers were injecting, what now is dubbed as Penisgate in their penis. The newspaper claimed that athletes inject the acid in the penis before they are measured for their suits.
Does Bigger Penis Help You Ski Better?: What Does Penisgate Do To The Penis?
Hyaluronic acid is used for cosmetic surgery, especially as a filler. Surgeons have also used it for penile girth enlargement. This is exactly why it is being used by the Olympians.
Injecting hyaluronic acid will increase the penile girth. However, experts point out that this means, one has to insert a lot of it in the penis to have this worked out. It is not a permanent solution, and can only last up to six to 12 months, depending on the absorption.
Inserting this will increase the penile girth or the penis circumference by one or two centimeters. As per the International Ski and Snowboard Federation, FIS, the surface area of their suits during competition could be increased by this, which increases their flight in the air, reported BBC.
"Every extra centimetre on a suit counts. If you suit has a 5% bigger surface area, you fly further," said FIS ski jumping's men race director Sandro Pertile, reported by BBC.
Does Bigger Penis Help You Ski Better?: Why Are Olympians Injecting Their Penises With Hyaluronic Acid?
Ahead of each season, ski jumpers undergo measurements using 3D body scanners and are required to wear only elastic, body-tight underwear during the process.
Regulations allow suit measurements a tolerance of just 2–4 cm. As part of this assessment, athletes’ crotch height is also recorded. The suit’s crotch height must match the athlete’s own measurement, with an additional 3 cm permitted for men.
Hyaluronic acid injections into the penis can last for up to 18 months.
Athletes have previously faced scrutiny for attempting to boost performance through alterations or manipulation of their suits.
Does Bigger Penis Help You Ski Better?: What Are The Risks Of Injecting Hyaluronic Acid In Penis?
Experts caution that penile injections using hyaluronic acid can pose serious short- and long-term risks.
They warn that improper technique or incorrect dosing may lead to pain, disfigurement, deformity, infection, inflammation, altered sensation, and sexual dysfunction. In rare cases, infections can worsen, causing tissue death (gangrene) and even loss of the penis.
COVID Vaccination Is Not Linked To Reduce In Childbirth, Says Study

Credits: iStock and Canva
A large population-based study from Linköping University in Sweden has found no evidence that COVID-19 vaccination caused a decline in childbirth during the pandemic, countering persistent rumors that mRNA vaccines affect fertility. The findings have been published in the peer-reviewed journal Communications Medicine.
The study was conducted amid widespread misinformation, particularly on social media, suggesting that COVID-19 vaccines reduce the chances of becoming pregnant. These claims gained traction as several countries, including Sweden, recorded a drop in birth rates during the later stages of the pandemic, prompting questions about a possible link to vaccination.
“Our conclusion is that it’s highly unlikely that the mRNA vaccine against COVID-19 was behind the decrease in childbirth during the pandemic,” said Toomas Timpka, professor of social medicine at Linköping University and one of the study’s authors.
Why Researchers Investigated the Claim
Since the early months of the pandemic, unverified claims about vaccines and fertility have circulated widely online. When official data later showed fewer babies being born in some regions, researchers decided to examine whether vaccination could plausibly explain the trend or whether other social and demographic factors were at play.
Read: Ahmedabad Toddler Swallows Hulk Toy, Showed X-Ray, Doctors Remove It Via Endoscopy
To address the issue, the research team carried out an extensive analysis using real-world healthcare data rather than surveys or self-reported outcomes.
Study Looks at Nearly 60,000 Women
The study analyzed health records of all women aged 18 to 45 years living in Region Jönköping County, a region with a total population of around 369,000 people. This amounted to nearly 60,000 women included in the analysis.
Between 2021 and 2024, about 75 per cent of these women received at least one dose of a COVID-19 vaccine. Researchers examined data on childbirths, registered miscarriages, vaccination status and deaths using official healthcare records, allowing for a comprehensive comparison between vaccinated and unvaccinated groups.
Importantly, the researchers adjusted their analysis for age, recognizing that age is one of the most significant factors influencing fertility and pregnancy outcomes.
No Difference in Births or Miscarriages
When childbirth rates were compared between vaccinated and unvaccinated women, the researchers found no statistically significant difference. The same held true for miscarriage rates among women who became pregnant during the study period.
“We see no difference in childbirth rates between those who have taken the vaccine and those who haven’t,” said Timpka. “We’ve also looked at all registered miscarriages among those who became pregnant, and we see no difference between the groups there either.”
These findings align with several earlier international studies that have similarly found no association between COVID-19 vaccination and reduced fertility.
Other Factors Likely Behind Falling Birth Rates
According to the researchers, the decline in childbirth observed during the pandemic is more plausibly explained by broader demographic and social trends.
People currently in their 30s, the age group most likely to have children, were born in the second half of the 1990s. That period was marked by economic challenges and lower birth rates in Sweden, meaning today’s pool of potential parents is smaller than in previous generations.
In addition, pandemic-related factors such as health concerns, economic uncertainty, delayed family planning and lifestyle changes during lockdowns may have contributed to fewer pregnancies.
One of the study’s key strengths is its large, representative sample drawn from an entire region rather than a selected group. By using verified healthcare records and accounting for age-related effects, the researchers aimed to minimize bias and improve reliability.
The study received financial support from several sources, including the Swedish Research Council.
These Are The 2 Major Reasons For Cancer, Says WHO

Credits: Canva
In 2022, there were almost 20 million new cases of cancer and 9.7 million cancer-related deaths worldwide, noted the National Cancer Institute (US). By 2050, it is predicted that the number of new cancer cases will rise to 33 million per year, with deaths rising to 18.2 million. While there are many reasons for cancer, a new comprehensive study by the World Health Organization (WHO) revealed that there are two major habits that are the leading cause of cancer.
As per WHO, more than 38% of cancer cases worldwide are linked to modifiable risk factors. The study is published in the journal Nature Medicine and it suggests that millions of diagnoses each year could be avoided through lifestyle changes, medical interventions, and environmental improvements.
WHO Study Says These 2 Major Habits Could Cause Cancer
Tobacco Use
As per the Association of Tobacco Use and Cancer Incidence, in India, the risk of any cancer with smoke and smokeless tobacco is 2.71 and 2.68, respectively. The study noted that risk of cancer due to tobacco use is consistent especially in India. Site-specific analysis showed higher risks of respiratory system cancers of 4.97 and head and neck cancers of 3.95.
As per several studies, including Cancer Research UK and National Institutes of Health (NIH), tobacco causes approximately 2.5 million cancer deaths globally, every year. This means, it accounts for 1 in every 4 global cancer death. It is also linked to 16 to 20 different types of cancer.
The WHO ranked it as the top reason for cancer, which is responsible for 15% of all global cancer cases. The impact is more in men, leading to 23% more new diagnoses.
Alcohol Use
The WHO study ranks it as the second most significant lifestyle factor that accounts for 700,000 new cases annually, leading to 3.2% of global cancer cases.
As per the National Cancer Institute (US), alcohol consumption is a significant, preventable cause of cancer, responsible for an estimated 741,300 to 750,000 new cancer cases worldwide in 2020. It is linked to cancers of the mouth, throat, esophagus, liver, colon, and breast. Even light-to-moderate drinking contributes, with about 185,100 cases annually tied to consuming two or fewer drinks per day.
What Are The Other Causes Of Cancer As Per WHO Study
Air pollution is a major cause of lung cancer, particularly in heavily polluted regions. In East Asia, for instance, around 15 per cent of lung cancer cases in women are linked to poor air quality. Experts say this underlines the urgent need for cleaner energy and stricter pollution controls.
Infections are another significant contributor, accounting for about 10 per cent of new cancer cases globally. High-risk strains of the human papillomavirus are the leading cause of cervical cancer, while stomach cancer is often linked to infections associated with unsafe water and poor sanitation.
Other important risk factors include high body mass index, lack of physical activity and excessive exposure to ultraviolet radiation, all of which continue to drive cancer rates across different populations.
© 2024 Bennett, Coleman & Company Limited

