- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can Dopamine Fasting Make You Happy Or Is It Just A Fad?

Credit: Canva
Fasting may reset your body, but can it reset your mind? The new trend of dopamine fasting claims it can. And wait, there's more. This trend also works against dopamine resistance, implying that things that did not make you happier before will now do. You see, dopamine is a part of the brain's reward system and plays an important role in your pleasure reception. While this neurotransmitter is not directly linked to an individual's happiness, it triggers feelings of satisfaction, motivation and pleasure.
However, a person can also reach a stage of dopamine resistance if they continue to indulge in activities that trigger its frequent or constant release. In this case, the individual stops feeling the impact of this neurotransmitter and thus, does feel good or happy.
So does dopamine fasting work?
Dopamine fasting is a practice where individuals limit their exposure to activities or stimuli that typically provide a surge of dopamine. The idea behind dopamine fasting is to reset or recalibrate the brain's reward system. This is usually done by abstaining from gratifying things or experiences like social media, junk food, and even sex. Proponents of dopamine fasting argue that continual overstimulation from digital devices, social media, and easily accessible indulgences has numbed our brain's reward pathways. By regularly denying ourselves these dopamine triggers, the idea claims, we might restore our ability to acquire fulfilment from life's basic pleasures.
How Does Dopamine Imbalance Affect Your Mental Health?
Having too much or too little dopamine in some parts of the brain is linked to some mental illnesses including depression, schizophrenia and psychosis. Having too much dopamine is linked to being aggressive and having trouble controlling your impulses. Dopamine imbalances are also related to ADHD and addiction.Having low levels of dopamine can make you less motivated and excited about things. In Parkinson's disease, there is not enough dopamine in the areas of the brain important for movement. This leads to problems with muscle stiffness and movements such as walking.
The symptoms of a dopamine imbalance depend on what is causing the problem. They include physical symptoms such as:
- muscle cramps, spasms or stiffness
- digestion problems, such as constipation or reflux
- pneumonia
- trouble sleeping
- moving or speaking more slowly than usual
- feeling tired and unmotivated, or sad and lacking hope
- having low libido (sex drive)
- hallucinations (experiencing something that's not real)
How Can I Adjust My Dopamine Levels?
Adjusting dopamine levels is complicated, as it is involved in many different roles in the brain. Your doctor won't measure your dopamine levels directly, and there is no simple test to measure it. Your symptoms will be the clues that tell your doctor if you have too much or not enough dopamine. They will then prescribe medicines to adjust your dopamine level, based on your symptoms, and make adjustments based on how your body responds and how you feel.
ALSO READ: Not Just a Screen Time Fix: 5 Timeless Health Habits from the ’50s
From First Period to Menopause: How Your Cycle Evolves Over the Years | Women's Day Special

Considered to be a key symbol of fertility and reproductive years, a woman's menstrual cycles are an integral and natural part of her life. However, they are more than just a monthly event, but instead a reflection of their hormonal, metabolic and even emotional health.
Due to genetics and other lifestyle factors, every woman experiences their cycle differently, which leaves many second-guessing about their hormonal balance, thyroid function, metabolic health, stress levels and even sleep quality.
Dr Archana Dhawan Bajaj, Gynaecologist and IVF Expert, Nurture exclusively tells Healthandme: "Knowing these patterns would guide people to understand when the changes are normal worry and when they are upheaval of a problem. Although the cycles vary among individuals, some features of such cycles are common between individuals, including the length of the cycle, flow, symptoms, as well as consistency, which are used to determine a normal state at various ages.
Here is what you should know and keep an eye out for during each phase:
The Early Years: Finding a Rhythm
Dr Maya PL Gade, Consultant, Gynaecology & Obstetrics at Kokilaben Hospital tells Healthandme: "In the first 2–3 years after menarche i.e. your first period, irregular cycles are common. Nearly 40–50 percent of adolescents do not ovulate consistently at first. The brain–ovarian hormonal axis is still maturing, so cycles may be longer than 35 days (than their typical 28 day monthly cycle) , bleeding may be heavy and cramps can feel intense.
Dr Rohan Palshetkar, Consultant IVF Specialist, Bloom IVF also warned that bleeding for more than 7–8 days continuously, soaking pads every 1–2 hours or going more than 90 days without a period may signal hormonal imbalance, clotting disorders, or conditions like PCOS.
He told Healthandme: "It is important to note that early teen cycles often happen without ovulation. For teenage girls, developing stable cycle will take some time due to ovaries adjusting to produce hormones. It is only in their late teens and early 20s that the girls will get the cycles more regular."
Normal Menstrual Cycle: According to Dr Bajaj, a normal cycle can be between 21 and 45 days. During bleeding, flow can be light, heavy, and cramps, mood swings, or even fatigue may accompany the adaptation of the organism to the hormonal changes.
Abnormal Menstrual Cycle: The expert explained: "Extensive bleeding, which needs the replacement of sanitary items every hour to two hours, long than seven or eight days, excruciating pain, or lack of periods in several months could be a sign of hormonal imbalance, thyroid complications, or polycystic ovarian syndrome."
20s and Early 30s: The Stable Phase
Talking about the post-teenager phase, Dr Gade said: "For many women, this is when cycles become more predictable, typically every 21–35 days, with 3–7 days of bleeding. Ovulation is more regular and PMS patterns are clearer. However, this is also the stage where lifestyle has a strong impact."
"Fertility is also at its peak in the 20s and early 30s, making it easy for women in this age group to become pregnant. With childbirth and breastfeeding, the chances of cycle alteration, its flow and length are high," Dr Palshetkar added.
Dr Gade also noted that high stress, poor sleep, intense exercise, crash dieting, thyroid disorders, or PCOS can disrupt ovulation and any sudden irregularity in this decade is often the body’s early warning system. A consistently painful period is also not “normal”, it may point to endometriosis or adenomyosis, both of which are frequently underdiagnosed,"
Keeping this in mind, it is essential for girls in their 20s and early 30s to track their period for regularity and flow, Dr Palshetkar advised.
Normal Menstrual Cycle: Dr Bajaj told this publication: "The average period to undergo a cycle is 21 to 35 days at an average of three to seven days with a moderate flow. The symptoms can be mild and include bloating, cramps or breast tenderness that can be easily treated."
Abnormal Menstrual Cycle: Talking about abnormal alterations, the gynaecologist said: "Excessive menstrual bleeding, cramps that impair normal life or inter-menstrual bleeding may be some of the early signs of endometriosis, fibroids, hormonal disruption or chronic stress."
Late 30s to 40s: The Hormonal Transition
Dr Gade explained: "Fertility begins to decline gradually after 35 due to reduced ovarian reserve. Cycles may shorten initially because ovulation happens slightly earlier. As women move into perimenopause, a transition that can last 4–8 years, hormone levels fluctuate unpredictably. Estrogen doesn’t simply drop; it rises and falls unevenly.
"This explains why many women notice heavier bleeding, clotting, worsening PMS, new-onset anxiety, sleep disturbances or cycles that skip months and then return. Studies suggest that up to 90 percent of women experience noticeable cycle changes during this phase.
"Importantly, very heavy bleeding at this stage should not be ignored. It can sometimes be linked to fibroids, endometrial thickening, or other structural changes in the uterus."
Moreover, Dr Palshetkar also warned: "For some, there is a noticeable and increasing gap between periods before menopause. Fertility decline is a reality in the age group, though it is not impossible to get pregnant.
Normal Menstrual Cycle: Dr Bajaj elaborated to Healthandme: "The hormonal shifts at this age may make the cycles a bit shorter or longer. Flow can either become thicker or thinner and premenstrual symptoms can be more pronounced as the body slowly transitions into perimenopause."
Abnormal Menstrual Cycle: Additionally, she said: "Very heavy bleeding, very prolonged intervals between the periods, bleeding following intercourse or sudden spotting between menstruation may be considered an issue, as these can be indicators of hormonal disorders, the presence of fibroids, or other gynecological problems."
Menopause: A New Baseline
Ultimately, Dr Gade detailed: "Menopause is diagnosed after 12 consecutive months without a period, with the average age globally around 50–51 years. Hormone levels stabilize at lower levels, and while periods stop, symptoms like hot flashes, vaginal dryness, bone density changes, and metabolic shifts may appear."
"Post-menopause, a woman’s reproductive health sees a significant decline of estrogen levels, fertility, and inability to produce any eggs. However, it still sees noticeable hormonal fluctuations and resultant health troubles.
"Facing PMS-like symptoms like mood swings and irritability is not uncommon. Medical attention is required when women notice severe pain or very heavy bleeding at
any age after menopause.
"The changes and evolution in the menstrual cycles are proof of her complete health during the course of the life she lives. And it impacts the way she lives or can live through her lifetime," Dr Palshetkar added.
Normal Menstrual Cycle: Lastly, Dr Bajaj said: "Prior to menopause, the cycles can become irregular since of the hormonal fluctuations and some symptoms like hot flushes, sleeping problems or mood swings can appear."
Abnormal Menstrual Cycle: While she noted that slight spotting is possible post-menopause due to fluctuations in estrogen and progesterone levels, the expert advised: "Post-menopausal vaginal bleeding is regarded as abnormal and needs to be medically examined because it may be due to underlying health conditions that must be addressed."
Hailey Bieber Revealed How A Mini Stroke At 25 Led To Her Discovering A Hole In Her Heart

(Credit - SHE MD Podcast/haileybieber/Instagram)
Hailey Bieber recently opened up about a mini stroke or Transient Ischemic Attack (TIA) she experienced when she was just 25. In an episode of the SHE MD podcast, hosted by Mary Alice Haney and Dr. Aliabadi, Hailey discussed how the mini stroke actually led her to find out an even bigger issue in her heart.
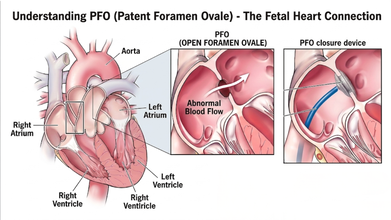
Dr. Aliabadi, a world-renowned OBGYN based in Los Angeles, who is also Hailey’s doctor, explained that this ordeal led Hailey’s medical team to discover a PFO, also known as a hole in her heart
In the interview, the founder of Rhode Beauty detailed how she had the classic stroke symptoms and said: “[My] whole right side of my arm went numb. I couldn't speak. Like my words were coming out all jumbled. The right side of my face was drooping. It was like a classic stroke symptom”
She explained that the reason why her team called it a mini stroke is because it ended within 31 minutes. By the time she reached the hospital, she didn’t need any clot busting medicine or procedure.

What Caused Hailey Bieber’s Mini Stroke?
Dr. Aliabadi explained that Patent Foramen Ovale (PFO) is extremely common phenomenon and a majority of people go through life never knowing they have it.
The Cleveland Clinic explains that the PFO is a small flap or opening between the upper chambers of your heart that everyone has. However, it usually closes up before the age of three. Most of the time, a PFO doesn’t cause symptoms and would not need treatment; however, in rare cases, it could lead to a stroke and or a TIA.
How Was Hailey’s Heart Condition Diagnosed
Hailey explained that her heart is slightly tilted in her chest and standard echocardiogram couldn't see the opening at first which led ER doctors to be unable to detect it.
As a result, she had to see a specialist for a Transcranial Doppler test. Doctors listened to the sound of blood "shunting" (moving the wrong way) through her heart to finally confirm the hole was there, which was much larger than they expected.
Also Read: Women Heart Symptoms Could Differ From Men, Explains Expert
What Is Transcranial Doppler Test?
According to the Cleveland Clinic, it is an ultrasound test that uses sound waves to detect conditions that affect blood flow to and within your brain. It can detect strokes caused by blood clots, narrowed sections of blood vessels, and numerous other heart-related issues.
How Did They Fix Hailey Bieber’s Heart?
Instead of an open-heart surgery, doctors performed a modern, minimally invasive procedure on Hailey's heart. She detailed the procedure where the doctors reached her heart through a vein in her groin. They threaded a tiny "button" made of metal and Teflon up to her heart and used it to securely plug the hole.
Hailey also learned she has some genetic factors that put her at a higher risk for blood clots and inflammation. Despite suffering a life-altering stroke, she views it as a "blessing in disguise" as it led her to find these issues early.
Now, she manages her health through a clean lifestyle, focusing on sleep, exercise and keeping her heart inflammation low.
Reducing Mother-To-Child HIV Transmission To Zero Key To End AIDS In India: Experts

Credit: iStock
Reducing mother-to-child HIV transmission, also called vertical transmission, to zero is crucial to achieve the end AIDS target by 2030 in India, in line with the UN Sustainable Development Goals, said experts.
At the 17th National Conference of the AIDS Society of India (ASICON 2026), health officials and experts together deliberated on the progress made in the country against HIV and also called for a stronger last-mile effort to eliminate AIDS from the country.
While India has made a major reduction in vertical HIV transmission, with just 0.7 percent of infant diagnoses. But the experts stressed the need to further reduce it to zero.
From 25 percent in 2020, the vertical transmission of HIV has come down to 11.75 percent in 2023, according to Dr. Glory Alexander, President of AIDS Society of India (ASI).
“Before treatments were available to prevent vertical transmission, the risk of a newborn acquiring HIV in India ranged from 15 percent to 45 percent. The risk was nearly 45 percent among infants who were breastfed,” Dr. Alexander said.
She attributed the reduction to the introduction of antiretroviral therapy (ART) and implementation of HIV prevention and treatment guidelines.
"The government has successfully reduced the rate of infant HIV diagnosis (risk of a child getting infected with HIV due to vertical transmission) to 0.71 percent. We need to further reduce it to zero to eliminate vertical transmission of HIV,” Dr. Alexander added.
Intensifying Last-Mile Approach
India reportedly has 27-29 million pregnancies every year.
As per the latest National AIDS Control Organization (NACO) report, 83 percent of all pregnant women are tested for HIV, and 78 percent of all pregnant women are tested for syphilis in India.
“Out of an estimated 19,000 pregnant women who might be living with HIV in India, over 16,000 were reached by the government-run program and linked to services -- half of them were newly diagnosed with HIV,” Dr. Alexander said.
NACO runs 794 antiretroviral therapy centers across the country and provides free HIV treatment to 18 lakhs people with HIV.
NACO's over 700 “Suraksha Sewa Kendras” also provide preventive services for people who are at risk of acquiring HIV.
Dr. Ishwar Gilada, Emeritus President of AIDS Society of India (ASI), called India's progress "commendable."
"But to end AIDS, the last mile approach has to be accelerated and intensified manifold,” the expert said.
Increase HIV Testing Manifold
Dr. Gilada stressed the need to "ensure that all key populations know their status, and those with HIV are linked to treatment, care, and support services and remain virally suppressed".
If a person with HIV is virally suppressed, then there is zero risk of any further HIV transmission, as per the WHO, he added.
Indian data shows 9-43 times higher HIV rates (as compared to the general population) among key populations, such as men who have sex with men, transgender people, sex workers, people who inject drugs, among others.
These key populations are hard to reach, which warrants community-led and science-backed approaches, said Dr. Gilada.
Reducing Advanced HIV Disease
Despite commendable progress in India’s HIV response, there is a huge number of cases of advanced HIV disease (AHD) -- about one third of all people living with HIV in the country, the experts said.
The World Health Organization (WHO) defines AHD as a CD4 count less than 200 cells per cubic millimeter/ or WHO stage 3/4 in adults/adolescents, and all children less than 5 years old.
It indicates a severely weakened immune system, high mortality risk, and vulnerability to infections like TB and cryptococcal meningitis.
AHD cases in India are majorly among those who are HIV infected but are not on lifesaving antiretroviral treatment.
"This could be because HIV infection is undiagnosed in people until they present with opportunistic infections to healthcare centers, or they were not able to adhere to the treatment for a range of reasons,” said Dr Trupti Gilada, Joint Secretary, AIDS Society of India (ASI).
TB, which is preventable and treatable, is the most common opportunistic infection among people with HIV.
Another concern is the rising antimicrobial resistance in HIV patients. Studies show that people with HIV are 2-3 times more likely to get drug-resistant forms of TB.
© 2024 Bennett, Coleman & Company Limited

