- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Is Huntington’s Disease Genetic? Here’s Everything You Should Know

Credits: Canva
Huntington’s disease (HD) is a condition that is hereditary and causes nerve cells in specific parts of the brain to slowly deteriorate and die. The disorder affects regions responsible for controlled and intentional movements, as well as those tied to mood, thinking, and personality. People with HD often develop jerky, dance-like body movements known as chorea, along with unusual postures and emotional or cognitive changes. For instance, they may experience sudden, uncontrollable motions in their hands, feet, face, or torso. These movements tend to worsen when the person feels anxious or distracted, and as the disease advances, they become more frequent and harder to manage.
Is Huntington’s Disease Genetic?
According to the National Institute of Neurological Disorders, Huntington’s disease is passed down genetically from parent to child. It follows an autosomal dominant inheritance pattern, meaning that only one copy of the faulty gene is enough to cause the illness. If a parent carries the gene, every child has a 50 percent chance of inheriting it. As it is known to be dominant, just one altered gene from either parent can trigger the disease.Also Read: Taking Amlodipine? NHS Issues Safety Warnings For Blood Pressure Patients, Here’s Why
The institute further explains that children who do not receive the mutated gene will never develop HD and cannot pass it on to their own children.
What Causes Huntington’s Disease?
Huntington’s disease stems from a mutation in the HTT gene. This defect creates an abnormal stretch in the DNA sequence, called an expanded CAG repeat. The mutation leads to the production of a faulty version of the huntingtin protein, which contains an excessively long polyglutamine chain.Over time, this unstable protein builds up in the brain and damages nerve cells. As the mutation is inherited in an autosomal dominant pattern, one copy of the defective gene is enough to cause the disorder.
Huntington’s Disease Can Now Be Treated With Gene Therapy
A new gene therapy treatment has shown promise in slowing the course of Huntington’s disease, marking what could be the first meaningful advance against this inherited brain disorder. In a recent clinical trial involving 29 patients in the early stages of HD, those who received a single, high-dose infusion of the therapy directly into the brain experienced a 75 percent slower progression over three years compared with the control group.The results, shared by the Amsterdam-based gene therapy company uniQure, were considered statistically significant across several clinical measures. Researchers also found lower levels of a harmful protein linked to brain cell damage in the spinal fluid of participants who received the treatment. Encouraged by these results, uniQure has announced plans to seek regulatory approval next year.
“This gene therapy represents a major step forward,” said Dr. Sandra Kostyk, a neurologist at Ohio State University Wexner Medical Center and one of the study’s investigators. “The data are encouraging.”
She added that while slowing the illness could mean more years of independence for patients, it is not a cure. Because of the small number of participants, more research and long-term follow-up are still needed.
Huntington’s Disease Symptoms You Need to Be Aware OfPeople with Huntington’s disease often lose control over their voluntary movements, which can affect daily functioning more severely than the involuntary jerks caused by chorea. Difficulties with voluntary movement can make it harder to work, communicate, and maintain independence.
According to the National Health Service, early signs may include trouble focusing or organizing tasks, forgetfulness, irritability, impulsive behavior, and changes in mood such as depression or anxiety. Other symptoms include small, uncontrollable jerks or twitches, clumsiness, and problems managing muscles.
Interestingly, symptoms can appear at any age but most often begin in a person’s 30s or 40s. When it develops before the age of 20, it is called juvenile Huntington’s disease. In such early-onset cases, symptoms may differ and the illness usually progresses more rapidly.
Taking Diazepam Or Alprazolam? Four Warning Signs Doctors Say You Must Watch For

Credits: AI Generated
A pharmacist has raised concerns for an estimated 4.8 million people in the UK who may be taking medicines such as diazepam or alprazolam. Fresh findings from Oxford Online Pharmacy suggest that one in five adults has obtained prescription-only drugs through illegal means. Anti-anxiety medicines top the list. Based on current population estimates, this could involve up to 4.8 million adults.
Another 10 percent of respondents said they had been offered medicines from unlicensed and unlawful sources, including online sellers, salons, corner shops, or even friends and family, although they chose not to take them.
As part of the study, a nationally representative group of UK adults was asked whether they had bought, received, or been offered medication from an unlicensed source. Among those who said yes, more than a third, around 35 percent, reported obtaining anti-anxiety medicines. These included selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and benzodiazepines such as Valium (diazepam) and Xanax (alprazolam), according to a report by the Mirror.
What Are Diazepam And Alprazolam Used For?
Diazepam, sold under the brand name Valium, and alprazolam, commonly known as Xanax, belong to a group of medicines called benzodiazepines. They work by calming activity in the brain and are mainly prescribed to manage anxiety. Diazepam is also used to treat seizures, muscle spasms, and symptoms of alcohol withdrawal.
Alprazolam, on the other hand, is more commonly prescribed for panic disorder. Diazepam stays in the body for longer, which makes it useful in withdrawal treatment, while alprazolam acts more quickly and is often chosen for sudden panic symptoms. Both medicines slow down the central nervous system to ease anxiety, but because of their effects and differences in how long they last, they should only be used under close medical guidance, as per Medicine Net.
Diazepam And Alprazolam: Why Are Doctors Warning Against It?
Kiran Jones, a clinical pharmacist at Oxford Online Pharmacy, has issued a strong warning for anyone thinking about using, or already using, anti-anxiety medicines sourced from the black market. “Anxiety is the most common mental health condition worldwide. At any given time, around 4 to 5 percent of people are living with an anxiety disorder. With such high numbers, it is not surprising that there is a growing illegal market for anti-anxiety drugs alongside those prescribed by qualified healthcare professionals. However, this trend is deeply worrying,” Jones said.
She explained that some benzodiazepines bought illegally are made to look like genuine prescription medicines but are actually counterfeit. These fake pills may contain extremely dangerous or even fatal substances, including synthetic opioids such as fentanyl. There is also a significant risk of addiction with these medicines, especially when they are taken over long periods. Over time, the body can develop tolerance, meaning higher doses are needed to achieve the same effect, which can quickly lead to dependence.
According to doctors and NHS guidance, there are several red flags people should be aware of:
Medication Appearance
If you have previously taken anti-anxiety medication, you may notice differences in the size or shape of tablets compared to what you were originally prescribed. If you are unfamiliar with the medicine, it is important to check online what the genuine product should look like and what the usual dosages are. You might also spot spelling mistakes in the drug name, manufacturer details, or listed ingredients, as well as differences in packaging design.
As per Mirror, these are often clear warning signs of a fake product. Proper packaging should always be sealed. If it appears opened, tampered with, or simply seems off, you should not take the medicine.
Medication Quality
Genuine medicines are produced to a consistent standard and should look uniform. Tablets should not be cracked, unevenly coated, or crumble easily when touched. Any signs of mould inside blister packs or containers should be treated as a serious warning sign.
You Have To Pay In Cash Or Via Bank Transfer
Reputable pharmacies and healthcare providers use secure and traceable payment systems. Requests for cash payments or bank transfers are commonly used by illegal sellers to avoid being identified and to keep transactions untraceable.
This lack of traceability makes it much harder to report scams, track down sellers, or get help if something goes wrong. If you come across an online provider and are unsure whether it is legitimate, you should check whether it is registered with the General Pharmaceutical Council before making any purchase. The UK government’s FakeMeds campaign also offers practical guidance on how to identify suspicious online sellers.
Disclaimer: This article is for general information only and should not be taken as medical advice. Always consult a qualified doctor, pharmacist, or healthcare professional before starting, stopping, or changing any medication, especially if you have an existing medical condition, are pregnant, breastfeeding, or taking other drugs.
Norovirus Cases Rise In The UK: How To Avoid Catching The Winter Vomiting Bug
Credits: AI Generated
Winter creates the perfect setting for coughs, colds, and stomach bugs. With people spending longer hours indoors, infections pass from person to person more easily. Right now, one virus in particular is spreading fast across the UK.
Norovirus, often referred to as the winter vomiting bug, is circulating widely. Several NHS trusts have announced a “critical incident” after a sharp rise in hospital admissions linked to norovirus and flu. A critical incident is declared when Accident and emergency departments are no longer able to provide all services safely.
With cases climbing this winter, many are asking the same question: how can you protect yourself from catching the winter vomiting bug?
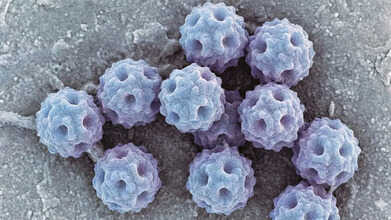
What Is Norovirus?
Norovirus is one of several viruses that infect the gut and cause symptoms such as diarrhoea, vomiting, and stomach cramps. These symptoms can continue for a few days and, in some cases, may lead to severe dehydration. Outbreaks are often reported in settings like cruise ships, nurseries, and care homes. You may have heard it called the “cruise ship virus.” These environments make it easier for the virus to spread because people are in close contact and often share food and drink sources.
Norovirus Symptoms To Take Note Of
Symptoms of norovirus typically appear between 12 and 48 hours after exposure, according to the California Department of Public Health (CDPH). People may experience repeated bouts of vomiting and diarrhoea throughout the day, with symptoms usually lasting one to three days.
As per the NHS, other symptoms include:
- Nausea and vomiting, often sudden and intense.
- Diarrhoea with loose, watery stools.
- Abdominal pain, including cramps and discomfort.
- Body aches, such as muscle pain and general weakness.
- Headaches.
- A mild fever.
Norovirus: How Can You Avoid Getting The Winter Vomiting Bug?
Try not to eat food prepared by anyone who is unwell or has recently been sick, although this is not always easy to manage. One of the most effective precautions is regular handwashing. Clean your hands with soap and water for at least 20 seconds, especially at key moments.
A useful habit is to wash your hands before putting anything in your mouth. This becomes even more important in group settings or if you are near someone who is ill.
If norovirus is a concern, make sure to wash your hands before eating in these situations:
- At shared meals, after serving dishes have been passed around and you have filled your plate.
- While snacking, if you are using shared utensils or pouring drinks from a communal bottle.
- After shaking hands when greeting people at gatherings involving food or drinks.
- In restaurants, after touching shared items such as menus or buffet and salad bar utensils.
- At work, if you are eating while using a computer or shared equipment.
- If washing your hands is not possible before handling food, it may be safer to eat using utensils only.
With proper care, most people bounce back from norovirus without complications. Staying well hydrated, getting enough rest, and managing symptoms should be your focus, while strict hygiene and isolation help stop the virus from spreading to others.
Lung Cancer Symptoms Can Show Up On Your Fingers: Here’s What To Look For

Credits: Canva
Lung cancer is especially dangerous because its symptoms often do not appear until the harmful cells have already spread through the body. However, there are some early warning signs you might be able to spot. Common indicators include breathlessness, wheezing, and a persistent cough that may bring up blood or mucus. While lung cancer is typically linked to respiratory problems like a chronic cough, shortness of breath, or chest discomfort, experts note that noticeable changes in your fingertips and nails can sometimes serve as early alerts for this potentially serious disease.
What Is Lung Cancer?
Lung cancer is a malignant growth that begins in the tissues of the lungs, usually from DNA damage in the cells lining the airways, which then grow uncontrollably to form tumors. Smoking is a major contributor, but other factors such as exposure to radon, asbestos, or inherited genetic conditions can also play a role.
Symptoms often include a persistent cough, chest pain, and difficulty breathing. Lung cancer is mainly classified into two types: Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC), according to the Cleveland Clinic.
Types Of Lung Cancer
Although many cancers can develop in the lungs, the term “lung cancer” usually refers to two main types: non-small cell and small cell lung cancer.
Non-Small Cell Lung Cancer (NSCLC)
NSCLC is the most common form, accounting for more than 80% of lung cancer cases. Common subtypes include adenocarcinoma and squamous cell carcinoma, while adenosquamous carcinoma and sarcomatoid carcinoma are less frequent forms of NSCLC.
Small Cell Lung Cancer (SCLC)
SCLC tends to grow more quickly and is more challenging to treat than NSCLC. It is often detected as a small tumor that has already spread to other areas of the body. Types of SCLC include small cell carcinoma (also known as oat cell carcinoma) and combined small cell carcinoma.
Lung Cancer Symptom On Fingers
Have you ever pressed your fingernails together and noticed a small diamond-shaped space of light? If that gap is missing, it could be a sign of finger clubbing, a condition where the ends of the fingers swell, which may indicate lung cancer.
This change occurs gradually, starting with the base of the nail becoming soft. Next, the skin around the nail bed may appear shiny, followed by the nails curving more than usual when viewed from the side.
Eventually, the tips of the fingers can enlarge and swell as fluid builds up in the soft tissue. While a missing diamond-shaped gap between your nails doesn’t automatically mean you have lung cancer, it can be a warning sign. If you notice this, it’s wise to consult your doctor.
What Are The Warning Signs Of Lung Cancer?
Lung cancer can present differently in every individual. Some people show multiple symptoms, while others may have none.
Key signs to watch for include:
- Swelling in the face or neck
- A cough that changes or worsens
- Frequent chest infections
- Shortness of breath
- Chest or shoulder pain
- Wheezing
- Coughing up blood or blood-stained phlegm
- Hoarseness
- A persistent cough lasting three weeks or longer
- Unexplained fatigue or low energy
© 2024 Bennett, Coleman & Company Limited

