- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Is It Safe To Drink Alcohol On Ozempic? Doctors Say The Effects Can Be Stronger

Credits: Canva
Ozempic (semaglutide) has quickly become a widely used drug for managing type 2 diabetes and supporting weight loss. With its growing use, many people are wondering whether it has any interaction with alcohol. There have also been reports suggesting that Ozempic may reduce alcohol cravings in some users.
While it is not always necessary to completely avoid alcohol while taking Ozempic, doctors say there are certain side effects and risks that should not be ignored. To understand this better, we spoke with Dr Monika Sharma, Senior Consultant in Endocrinology at Aakash Healthcare.
Also Read: Nicotine Pouches: Are They Really A Safer Alternative To Smoking, Or Just Another Health Risk?
Can Ozempic Make Alcohol Hit Twice as Hard?
Yes, alcohol can feel noticeably stronger when taken alongside medications like Ozempic, and this has a lot to do with how the drug alters digestion, metabolism, and brain signalling. Ozempic belongs to a class of medicines called GLP-1 receptor agonists. It is primarily prescribed for type 2 diabetes and is increasingly used for weight management. One of its key actions is slowing down stomach emptying, meaning that both food and liquids stay in the stomach longer before moving into the intestines.
Dr Sharma explains, “When alcohol is consumed, delayed gastric emptying can lead to uneven absorption. In some people, alcohol enters the bloodstream later but more rapidly once absorption begins, which can raise blood alcohol levels faster and intensify intoxication even with smaller amounts.”
Ozempic and Alcohol: Reduced Appetite and Drinking On An Empty Stomach
Another major factor is appetite suppression. Many people on Ozempic eat significantly less or skip meals altogether, either intentionally or due to reduced hunger. Drinking alcohol on an empty or nearly empty stomach allows it to be absorbed more quickly, as there is little food to slow the process. As a result, an amount of alcohol that once felt manageable may suddenly cause dizziness, flushing, nausea, or loss of coordination much sooner than expected.
Ozempic and Alcohol: Brain Effects and Alcohol Sensitivity
Ozempic also affects areas of the brain linked to reward, fullness, and impulse control. Emerging research suggests that GLP-1 receptor agonists may lower cravings for substances like alcohol, while at the same time increasing sensitivity to its effects. This means that even if the desire to drink decreases, the body’s reaction to alcohol may feel stronger or more unpleasant. Many users report unusual tiredness, light headedness, or nausea after just one drink, often describing it as alcohol “hitting twice as hard.”
Ozempic and Alcohol: Blood Sugar Changes and Hypoglycemia Risk
Blood sugar regulation is another concern. Alcohol can cause fluctuations in glucose levels, and when combined with a medication that tightly controls insulin release and glucose use, the risk of low blood sugar increases, particularly for people with diabetes. Symptoms of hypoglycemia include sweating, shaking, confusion, and palpitations. These signs can resemble alcohol intoxication or worsen its effects, making the experience more intense and potentially dangerous.
Ozempic and Alcohol: Dehydration and Slower Recovery
Dehydration also plays a role. Ozempic can cause side effects such as nausea, vomiting, and reduced fluid intake, all of which increase the risk of dehydration. Alcohol further depletes fluids, and when the body is already low on hydration, alcohol’s impact on the brain and heart becomes stronger. This can lead to faster intoxication, headaches, and a longer recovery time after drinking.
Ozempic and Alcohol: Gut Sensitivity and Worsening Side Effects
Gastrointestinal sensitivity should also be considered. Ozempic commonly causes nausea, bloating, acid reflux, and stomach discomfort, especially in the early months of treatment. Alcohol irritates the stomach lining and relaxes the lower oesophageal sphincter, which can worsen these symptoms. Together, even small amounts of alcohol can trigger stronger negative reactions, reinforcing the feeling that tolerance has suddenly dropped.
Why Alcohol Feels Stronger On Ozempic
While Ozempic does not directly interact with alcohol the way some medications do, its indirect effects on digestion, hydration, metabolism, and the nervous system can make alcohol feel more potent. This is why moderation is strongly advised. People taking Ozempic should limit alcohol intake, avoid drinking on an empty stomach, stay well hydrated, and pay close attention to how their body responds.
In short, Ozempic can make alcohol feel stronger not because it increases alcohol levels directly, but because it changes how the body processes and reacts to alcohol. Being aware of this interaction can help people make safer, more informed choices while using this medication.
Can A Cyst Grow Teeth And Hair Inside The Body? Everything You Need To Know About Dermoid Cysts

Credits: canva
A woman experiencing abdominal discomfort went to her gynecologist for an ultrasound, only to discover something far more startling than a baby. The mom, who shares her story on TikTok under the handle @sandwitchbread, revealed her medical surprise in a video that has now amassed over 1.9 million views. She said she had been struggling with pain and unusual bleeding since giving birth to her two-year-old son and decided to see a gynecologist fearing she might be pregnant again.
During the ultrasound, she noticed something on the screen, but the doctor quickly reassured her it wasn’t a baby. “When my doctor came in to share the results,” the TikToker recalled, “she looked me in the eyes and told me I had a seven-centimeter cyst, about the size of a chicken egg, called a dermoid cyst.”
What Is A Dermoid Cyst?
A dermoid cyst is a pocket of tissue growth that can contain normal body tissues, sometimes including hair, fluid, teeth, or skin. While this TikToker’s cyst was in her uterus, dermoid cysts are most commonly found in the ovaries. They are generally harmless but often require surgical removal. According to the National Cancer Institute, dermoid cysts are present from birth but may not be detected until later in life. These benign tumors originate from embryonic cells that become “trapped” and develop into tissues in the wrong location. Teeth and hair are frequent components, and surgery is usually recommended if the cyst causes symptoms or complications.
Why Do Dermoid Cysts Have Hair and Teeth?
Dermoid cysts develop hair and teeth because they arise from trapped embryonic cells (ectoderm) that can grow into skin, hair follicles, sweat glands, and even teeth, instead of forming the tissues normally found in the ovary or skin. Essentially, they are benign tumors made up of mature but misplaced body tissues from the outer layer of the embryo, which normally forms skin and related structures.
Dermoid Cysts: Symptoms
Most ovarian dermoid cysts remain symptom-free unless complications occur. When symptoms do appear, the most common one reported is lower abdominal pain.
As the cyst enlarges, it can cause noticeable abdominal swelling and problems with the urinary or digestive system.
In more severe cases, individuals might also experience:
- Fever
- Intense abdominal pain
- Unusual vaginal bleeding
- Unexplained weight loss
The Office on Women’s Health notes that cysts on the ovaries can also cause:
- Pressure in the abdomen
- Bloating
- Abdominal swelling
- Pain in the lower abdomen
Dermoid Cysts: Possible Complications
Some potential complications include:
Rupturing of the cyst: Though rare, ovarian dermoid cysts can burst. If the cyst’s contents leak into the abdominal cavity, it may lead to chronic inflammation of the abdominal lining (peritonitis). In some cases, leakage into the intestines or rectum can result in the material being expelled through the anus.
Ovarian torsion: This occurs when the cyst twists the ligaments holding the ovary in place, which can cut off blood supply to the ovary and fallopian tube.
Infection: The risk of infection is around 1–4%. Severe infections may lead to cyst rupture.
Malignant transformation: Dermoid cysts are almost always benign, but in rare instances, they can become cancerous.
Is Retatrutide The Next Weight-Loss Breakthrough After Ozempic And Mounjaro? Here’s How It Works Differently
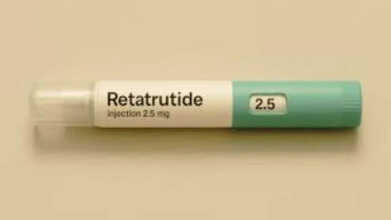
Credits: Canva
A new weight-loss drug often described as the “triple G” treatment because it mimics three hormones linked to hunger and metabolism has delivered striking results in fresh data shared Thursday by its developer, Eli Lilly. In a clinical study involving more than 400 people living with obesity and knee osteoarthritis, the experimental drug retatrutide led to an average weight reduction of 71 pounds, or close to 29% of total body weight, over a period of 16 months, according to figures released by the company. Participants who received retatrutide also reported a 76% drop in knee pain by the end of the study period, based on the same data. So is
What Is Retatrutide?
Retatrutide is an experimental weight-loss drug developed by Eli Lilly and is widely seen as a next-step advancement beyond current GLP-1-based medications such as semaglutide and tirzepatide. While semaglutide acts on a single hormone pathway and tirzepatide works on two, retatrutide targets three.
It activates GLP-1 and GIP, along with an added glucagon pathway, which is why it is sometimes informally referred to as a “GLP-3” drug. Researchers believe this third pathway could explain the greater weight-loss effects seen so far, although retatrutide remains under investigation and has not yet received FDA approval.
Why Is Retatrutide Trending?
Even without regulatory approval, retatrutide has gained attention among gym enthusiasts, fitness creators, and online weight-loss communities. On platforms like TikTok, where direct searches for #reta or #retatrutide are restricted, users often refer to it using coded terms such as “ratatouille.”
At the same time, the drug has been in the news due to growing concerns about counterfeit versions. Reports from the UK recently revealed that authorities seized more than £250,000 worth of fake weight-loss injection pens labelled as tirzepatide and retatrutide from a hidden factory in Northampton. These products are especially concerning because retatrutide is still in clinical trials and has not been approved for use anywhere in the world.
How Is Retatrutide Different Than Other Weight-Loss Drugs?
Retatrutide works by mimicking three hormones that play a role in appetite and metabolism: GLP-1, GIP, and glucagon. In contrast, most weight-loss drugs currently available target only one or two of these pathways. Ozempic and Wegovy, made by Novo Nordisk, copy the effects of GLP-1, a hormone that influences the brain, pancreas, stomach, liver, and muscles, according to the National Institutes of Health.
Mounjaro and Zepbound, on the other hand, act on both GLP-1 and GIP, a hormone involved in blood sugar regulation through insulin stimulation. Retatrutide’s added glucagon effect is key, as glucagon is known to support fat burning, even when the body is at rest. Ozempic and Mounjaro are approved by the FDA for treating Type 2 diabetes, while Wegovy and Zepbound are approved for people with overweight or obesity. As with any prescription drug, it is important for individuals to consult a healthcare professional to determine whether these treatments are appropriate for them.
When Is Retatrutide Expected To Be Available To Consumers?
There is currently no confirmed timeline for when retatrutide might become available by prescription. Its launch will depend on the FDA’s detailed evaluation of clinical trial data once it is formally submitted. Based on current expectations, approval is unlikely before late 2026 and could potentially extend into 2027 or even 2028.
Nicotine Pouches: Are They Really A Safer Alternative To Smoking, Or Just Another Health Risk?

Credits: Canva
The use of nicotine pouches is rising sharply across the UK, especially among young adults, recent research suggests. These small pouches sit between the lip and gum and release nicotine gradually into the body. Available in many flavours, they often include sweeteners and plant-based fibres. But are they truly a better option than smoking, or could nicotine pouches still pose health risks? We take a closer look below.
What Are Nicotine Pouches?
Nicotine pouches are small, tobacco-free sachets that contain nicotine powder along with flavourings and fillers. They are placed between the lip and gum, similar to snus, allowing nicotine to be absorbed without smoke, vapour, or spitting. Marketed as a discreet way to consume nicotine, they still deliver a highly addictive substance and expose users to certain chemicals. Health experts have raised concerns, particularly for young people, despite these products often being promoted as a “safer” choice than cigarettes.
Popular brands such as Zyn, On!, and Velo now dominate a fast-growing market, according to the CDC. Like vaping, they do not contain tobacco and are generally viewed as less harmful than smoking.
A recent study led by researchers at University College London (UCL) found that over the past five years, about 522,000 additional people in the UK have started using nicotine pouches, with usage rising from 0.1% to 1% of the adult population.
This has raised an important question: are nicotine pouches actually safer than smoking, and what is driving their sudden popularity?
Nicotine Pouches: Is Using Them Safer Than Smoking?
Speaking on *Mornings with Ridge and Frost*, lead study author Dr Harry Tattan-Birch from UCL’s Institute of Epidemiology and Health Care told Sky News that the risks linked to nicotine pouches are much lower than those associated with smoking. “There’s no tobacco and no combustion,” he explained. “And we know it’s the burning of tobacco that causes most smoking-related diseases.”
That said, Dr Tattan-Birch and his colleagues stressed that these products are not harmless and should never be accessible to children. The NHS notes that while nicotine itself does not cause serious diseases in the way tobacco does, young people’s developing brains and lungs are more vulnerable to its effects, and dependency can form quickly.
UCL research fellow Eve Taylor also told Sky News that nicotine pouches are “far less harmful than smoking,” but cautioned that they are still relatively new. Because of this, their long-term effects are not yet fully understood. “We can look at what’s in them to estimate potential risks,” she said. “They’re not risk-free. Users are still exposed to some toxic substances, even if the levels are much lower.”
Nicotine Pouches: Are Pouches Helping People Quit Smoking?
According to UCL’s findings, among participants surveyed between January 2022 and March 2025, 69% of nicotine pouch users were also using other nicotine products. More than half of them, 56%, were still smoking cigarettes. Around one in six users, or 16%, reported that they had never been regular smokers, suggesting the habit was not linked to quitting cigarettes.
As quoted by Sky News, Dr Tattan-Birch said the public health impact of nicotine pouches depends largely on who is using them. “If a young person who might otherwise smoke switches to pouches, that could reduce harm,” he said. “But if someone who wouldn’t have used nicotine at all starts using them, the risk of harm goes up.”
Researchers added that more studies are needed to understand whether nicotine pouches genuinely help people stop smoking in the long run.
Are Nicotine Patches Harmful For Health?
Nicotine patches are widely regarded as safer than smoking and are a well-established aid for quitting. They provide a steady dose of nicotine to reduce cravings without exposing users to tar or cancer-causing chemicals found in cigarettes. However, they are not completely without side effects. Common issues include skin irritation, headaches, and sleep disturbances. People with serious heart conditions or those who are pregnant are advised to speak with a doctor before using them, as nicotine can still affect heart rate and blood pressure, though far less dangerously than smoking, according to the CDC.
© 2024 Bennett, Coleman & Company Limited

