- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
It Took 26 Doctors, 37 Procedures, and 17 Years For New York-Based Journalist To Get Her Diagnosis Right
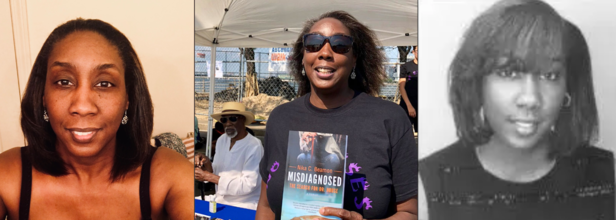
Credits: Patient Wing, Future of Personal Health, Goodreads
For more than 17 years, one woman battled a growing list of unexplained and debilitating symptoms—fatigue, joint pain, spontaneous fevers, and swollen lymph nodes—without a clear diagnosis.
A former college athlete who once thrived on high-impact sports like rugby and ice hockey, she eventually found herself physically debilitated and mentally drained. Despite multiple hospital visits and consultations with specialists, answers remained elusive.
According to USA Today, her health journey began in college, where daily life became a struggle. Tests for common conditions, including mononucleosis and autoimmune disorders, failed to reveal anything conclusive. By her mid-30s, Nika Beamon, a New York-based author and an award winning journalist, had suffered two strokes, and yet, no diagnosis explained the persistent deterioration in her health.
The delay in diagnosis was not for lack of trying—she saw 26 doctors and underwent 37 medical procedures. Every physician agreed something was wrong. What remained unclear was what exactly was wreaking havoc in her body.
“I felt like I was aging rapidly,” she told USA Today. “It was as if you went from 20 to 50 in a day.”
A Long-Awaited Diagnosis
More than a decade and a half after her symptoms began, a rheumatologist finally offered clarity. The mystery illness turned out to be IgG4-related disease (IgG4-RD), a rare immune-mediated condition that can inflame and damage organs if left untreated.
All it took to confirm the diagnosis was a blood test—an infuriatingly simple step that hadn’t been taken earlier because no one had a reason to look for such a rare disorder.
The immune disorder was first widely recognized by Japanese gastroenterologists in 2006, with formal naming and classification happening in 2012. The disease tricks the body’s immune system into producing excess IgG4 antibodies, which can form masses or cause swelling in critical organs such as the liver, lungs, or pancreas.
If these affected organs aren’t treated in time, irreversible damage—like cirrhosis—can occur.
While not fatal if caught early, the disease's real threat lies in its stealth and its ability to mimic other conditions. It’s often misdiagnosed or mistaken for cancer, as the masses caused by excess immune cells closely resemble tumors.
“It’s not cancers or anything,” a medical expert told USA Today. “It’s just that the immune system is confused and reacting to something.”
When Diagnosis Is Delayed
The journey to diagnosis for IgG4-RD is often complicated because the symptoms are both non-specific and widespread. Fatigue, joint pain, fevers, or masses can be attributed to more common conditions. It’s only when these symptoms span multiple organs, or when an aware radiologist spots a distinctive pattern on imaging, that IgG4-RD is even considered.
In this case, it took over 17 years for someone to finally put the pieces together. The woman had no known family history of autoimmune or immune-related conditions, making her case more perplexing. Compounding the delay was a lack of widespread awareness and diagnostic protocols for IgG4-RD at the time her symptoms began.
Treating IgG4-RD: A New Era
Treatment for IgG4-RD typically starts with steroids like prednisone, which can reduce inflammation. However, these drugs aren’t viable long-term due to their significant side effects. More recently, the FDA approved Uplizna, the first drug specifically designed to target IgG4-RD. The monoclonal antibody works by suppressing the B-cells responsible for producing the problematic antibodies.
In clinical trials, Uplizna showed an 87% reduction in flare-ups. Patients can now expect better management of the disease with fewer side effects and a more targeted approach.
“Most patients do well if the disease is diagnosed and treated on time,” USA Today reported, citing clinical experts.
Life After Diagnosis
Now in her 50s, Beamon continues to manage her condition with medications and regular checkups. Although the disease hasn’t disappeared, having a name for it—and a treatment plan—has drastically improved her quality of life.
“There are good days and bad days,” she admitted to USA Today, referring to flares and periods of inflammation.
She also found strength in community support, especially after publicly sharing her story and publishing a memoir documenting her medical journey. Her advice to others still searching for answers: advocate for yourself, keep detailed records, and bring someone to medical appointments.
Most importantly, she urges patients not to give up. “There’s always a doctor out there that can help you,” she said. “You just have to find the right one.”
No Smoking Day: Are There Science-backed Methods To Quit Smoking?

Credits: Canva
On No Smoking Day, we drive our focus to science-backed methods that can help one leave smoking. Smoking is one of the leading causes of preventable deaths worldwide. It also contributed to severe health problems, including cancer, cardiovascular diseases, and respiratory diseases. Even though many people are aware of this harmful consequences, many struggle to quit smoking. Mostly because it is a habit often associated to enjoying a break. Even when someone does not need it, their brain tricks them into believing that smoke is important for the break they are meant to enjoy.
However, there are several studies that have explored science-backed methods that could help one to quit smoke.
A study published in the journal Addiction, emphasizes three primary methods proven effective for quitting smoking: behavioral support, prescription medications, and nicotine replacement therapy (NRT). These strategies have shown varying levels of success in aiding smokers to quit permanently. In addition, alternative methods like e-cigarettes and mindfulness-based techniques have gained traction in helping reduce smoking addiction.
Quitting smoking is more than just a decision; it’s a commitment to significantly improving your health and well-being. Smoking has been directly linked to various cancers, lung diseases, and heart conditions. In the long term, stopping smoking can lower your risk of these life-threatening conditions.
According to the study, individuals looking to quit smoking should consider using Varenicline (sold as Chantix/Champix), Cytisine (a plant-based supplement available in Europe and Canada), or nicotine e-cigarettes.
“Quitting smoking is difficult, and some people find it harder to quit than others, but tobacco is uniquely deadly among legal consumer products, so it’s important to seek help quitting,” said lead investigator Jonathan Livingstone-Banks, a lecturer and researcher in evidence-based health care with the University of Oxford in the U.K.
Read: Does Smoking Affect Women Differently Than Men?
What Happens When You Stop Smoking?
- In just 20 minutes of stopping, your blood pressure and heart rate begin to normalize.
- Within a few weeks, your lung function improves.
- Over time, the risk of heart disease and cancer also decreases dramatically.
Three Science-backed Methods That Could Help You Quit Smoking
Behavioral Support
Quitting smoking isn’t just about resisting cravings. Often, behavioral support through counseling or therapy is crucial for tackling the psychological aspects of addiction. Behavioral therapy involves working with a trained professional to identify triggers, develop coping strategies, and create a tailored quit plan. Research shows that combining counseling with other quit methods can significantly increase success rates.
Prescription Medications
Some medications, such as varenicline (Chantix) and bupropion (Zyban), have been shown to help people quit smoking by reducing cravings and withdrawal symptoms. Experts suggest that varenicline works by blocking the effects of nicotine in the brain, while bupropion is an antidepressant that helps manage withdrawal symptoms. Both medications are generally more effective when combined with behavioral therapy.
Nicotine Replacement Therapy (NRT)
Nicotine replacement products, such as nicotine patches, gums, lozenges, and nasal sprays, deliver controlled amounts of nicotine to ease withdrawal symptoms. According to experts at Harvard Health, NRT can double the chances of quitting by alleviating physical cravings while the person works on overcoming the psychological addiction.
The Silent Rise of Fatty Liver Disease: How India-Specific Guidelines Can Help

Metabolic dysfunction-associated steatotic liver disease (MASLD), previously called fatty liver disease, is becoming extremely common in people with type 2 diabetes in India.
Studies suggest that 50–70 percent of Indians with type 2 diabetes may have fatty liver, and a significant proportion can progress to inflammation, liver fibrosis, cirrhosis, or even liver cancer if the condition is not detected early. Because India already has one of the world’s largest populations with diabetes, MASLD is emerging as a major but under-recognized public health problem.
The recently published consensus guidelines developed by Indian experts aim to provide practical, India-specific recommendations for diagnosing and managing MASLD in people with type 2 diabetes.
In fact, these are the first global guidelines for MASLD and type 2 diabetes, albeit restricted to India. This matters because most existing international guidance—including from organizations such as the American Diabetes Association—is largely based on evidence and healthcare systems in high-income Western countries. These recommendations often assume easy access to expensive diagnostic tests and medications, which may not always be feasible in India.
In India, healthcare costs are frequently paid out-of-pocket by patients. Advanced imaging tests or newer medications can therefore be unaffordable for many people.
The Indian consensus addresses this reality by recommending step-wise and cost-effective screening strategies, beginning with simple clinical risk assessment and basic laboratory tests, followed by non-invasive fibrosis scoring tools and ultrasound when appropriate. This approach helps identify high-risk individuals without overburdening patients or the healthcare system.
Another important reason these guidelines matter is that Asian Indians have a unique metabolic profile. Compared with Western populations, Indians often develop diabetes and fatty liver at younger ages and lower body weight, partly because of higher abdominal fat and insulin resistance. Therefore, early screening for liver disease in people with diabetes becomes particularly important in India.
Dietary recommendations are also adapted to local eating patterns. Instead of focusing on Western dietary models, the guidelines emphasize reducing refined carbohydrates, excess sugars, and unhealthy fats common in Indian diets while promoting traditional, healthier foods, whole grains, legumes, and increased physical activity.
In simple terms, these India-specific guidelines aim to ensure that more patients with diabetes are screened early, treated appropriately, and protected from severe liver complications, using strategies that are practical, affordable, and suited to the realities of the Indian healthcare system.
How These Guidelines Differ From Those In The West
Guidelines for MASLD developed in Western countries provide important scientific guidance, but they are often designed for healthcare systems with greater resources and different patient characteristics. The Indian consensus recommendations differ in several key ways to make them more suitable for local populations and healthcare settings.
First, screening strategies are more pragmatic and cost-conscious. Western guidelines often recommend advanced imaging tests or specialized biomarkers to assess liver fat and fibrosis. However, these tests can be expensive and not widely available in many parts of India.
The Indian recommendations emphasize simple, widely available tools—such as routine blood tests and non-invasive fibrosis scoring systems—before considering more advanced imaging. This stepwise approach ensures that patients who are most at risk are identified while keeping costs manageable.
Second, the guidelines recognize the unique metabolic risk profile of Asian Indians. Compared with Western populations, Indians tend to develop metabolic diseases such as type 2 diabetes and fatty liver at younger ages and lower body mass index (BMI). Abdominal obesity and insulin resistance are particularly common.
Therefore, the Indian recommendations stress earlier and more vigilant screening for MASLD in people with diabetes, even if they are not severely obese.
Third, treatment priorities differ because of affordability and access to medications. Western guidelines may emphasize newer and often expensive drugs that show benefits for fatty liver disease. While these therapies can be effective, they may not be accessible to many patients in low- and middle-income countries.
The Indian consensus places stronger emphasis on lifestyle interventions, weight reduction, improved diet, and physical activity as the foundation of treatment, while suggesting pharmacotherapy selectively based on evidence, availability, and cost.
Fourth, perhaps the most important difference, dietary advice is culturally tailored. Western guidelines typically discuss Mediterranean-style diets.
In contrast, the Indian recommendations translate healthy eating principles into Indian dietary patterns, focusing on reducing refined carbohydrates, sugar-sweetened foods, and excess saturated fats while promoting whole grains, pulses, vegetables, and traditional balanced meals.
Finally, the Indian document highlights the need for public health awareness and primary care involvement, since a large proportion of patients with diabetes are managed outside specialized centers.
Overall, the key difference is that while Western guidelines provide strong scientific foundations, the Indian recommendations adapt those principles to local realities.
Bristol Palin May Turn To Botox Or Surgery To Treat Facial Paralysis

Credits: Wikimedia Commons and Instagram
Bristol Palin, an American real estate agent, who was a former public speaker and reality television personality started experiencing facial paralysis over a tear ago. On March 9, her 35-year-old daughter Sarah Palin posted a video on her Instagram Stories that shared an update on her ongoing health struggles. The story revealed that she is now considering plastic surgery to fix her paralysis.
"I am going to have a consultation today with a plastic surgeon in Austin," she said. "I have read that she specializes in facial paralysis type stuff so we will see what she says."
She also said, "Prayers because maybe she can help mostly with this eye," while pointing to her left eye. "When I smile or when I am expressive, it closes. I don't really care about my crooked mouth but my eye...so embarrassing to me. I feel like I should wear an eyepatch or something."
She went on to say, "It looks crazy and I just feel like I cannot even smile because it just closes. So maybe she can do some Botox or maybe there is some options with surgery. So we will see. Maybe she ca help with this eye or just the overall symmetry."
She also said that she had just returned from Alaska, where she visited another specialist who does her facial nerve blocks to help her paralysis. She also posted another update on her Instagram Stories and said that her consultation went well and that she will be sharing the information with her followers soon.
What Happened To Bristol Palin?
It was in January 2025, when she revealed her facial paralysis on Instagram. "I woke up nine days ago with a little weird sensation in my face. My mouth was pulling this way and it just felt a little off. So I went, looked in the mirror. I'm like 'Wow. This is looking a little weird. I feel like everything is pulling to the left."
She said that hours later her condition got worse and the left side of her face was having a "delayed" reaction.
Read: Why Does Your BBL Smell? Doctor Explains 4 Reasons That Could Cause It
Can Botox Fix Asymmetrical Face?
As per a 2020 study published in the Indian Journal of Plastic Surgery, botulinum toxin (Botox) injections are helpful and are minimally invasive technique to restore facial symmetry. However, the study noted that a "surprisingly small minority of aesthetic injectors treat this condition."

The study also gives a case study of a patient with longstanding facial nerve paralysis after resection of an osteogenic sarcoma, before and after two weeks after first treatment with botulinum toxin. The improvements could be seen in mentalis synkinesis, more symmetrical smile, and improved eye apertures on animation.
What Is Botox?
It is an FDA-approved, injectable neurotoxin derived from Clostridium botulinum bacteria. It temporarily relaxes muscles by blocking nerve signals, commonly used to smooth dynamic wrinkles and treat medical conditions like chronic migraines, excessive sweating, and muscle spasms. Its effects last from three to four months.
Botox prevents the release of a neurotransmitter that signals muscles to contract, causing them to relax and soften wrinkles. Results typically appear in 3 to 14 days.
© 2024 Bennett, Coleman & Company Limited

