- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
John Cena Opens Up About His Skin Cancer Diagnosis, Talks About Why Sunscreen Is Important
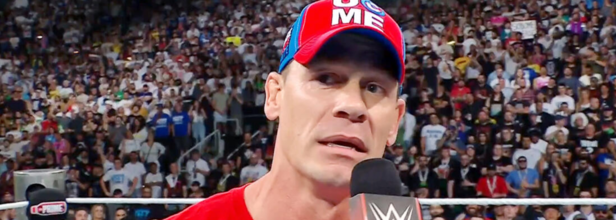
Credits: WWE
We have all heard about the benefits of using sunscreens, but how many of us actually follow it through? Especially among the men, there is a conventional belief that anything on their skin is not manly enough. But, what if I tell you that even someone as strong as John Cena recommends everyone to wear sunscreen? Would you still choose to not use it?
John Cena, actor and the WWE star has recently opened up about a past skin cancer diagnosis in an effort to bring attention to the important of wearing sunscreen. He told People that he grew up in Massachusetts in the 1970s and 80s, and "never" wore sunscreen. It was later in life when he moved to Florida, and there he "fell in love with the sun", but "neglected" to protect his skin and use sunscreen.
“I was stubborn. I didn’t want to have a routine and I also thought the problem would never reach me. And it’s one of those things where I had a ton of exposure with minimal protection and it caught up with me,” said Cena.
How Did The Diagnose Happen?
It was during one of his routine check-ups that made Cena to re-think to use sunscreen. “It wasn’t until I went to a dermatologist and got a skin checkup and had a cancerous spot removed from my right pec,” he said.
Cena is now also the face of a sunscreen brand with SPF 70. He revealed that he was "very lucky" to have a good dermatologist who help him face his fear around his diagnosis.
After the removal of first cancerous spot on Cena's chest, there was another. "A year later, I went back and had another spot removed close to my right shoulder. It shows up like a white polka dot on the side of my chest and on my shoulder. If you watch WWE, you’ll be able to see them," he said.
It was a shock to him, because he never saw being diagnosed with skin cancer coming. "Mind always goes to the worst case scenario," he said. However, it was the diagnosis that allow him to understand the importance of sunscreen that protects one's skin from sun's rays.
“I’m at a great space in my life where that’s now important to me. And I’m so grateful to be able to dodge those two bullets, but I wear them as a reminder of, ‘Hey man, you need to take the extra few seconds to protect yourself every day,’” he said.
ALSO READ: Does Sunscreen Block Your Body's Natural Vitamin D Production?
At What Time Of The Day Should You Apply Sunscreen?
As per the Johns Hopkins Medicine, wearing sunscreen is the easiest and the best ways to protect your skin's appearance and health at any age. It recommends to use it regularly to prevent sunburn, skin cancer, and premature aging.
While everyone needs sun exposure to produce vitamin D, unprotected exposure to the sun's UV rays can cause damage to the eyes, skin, and the immune system.
To protect, apply 1 ounce of sunscreen throughout your body. To protect your face and neck, you will need about half a teaspoon of sunscreen.
Experts also believe that as long as the sunscreen is at least SPF 30 and is water-resistant, it does not matter what order you apply your skin care products. While some people find it is easiest to work with bare skin, some do it at the end.
"If you’re out there and you brush your teeth, at a young age you learned that going to the dentist when your teeth are in bad shape is bad because it’s painful. The same thing will happen if you don’t take care of your skin, and it’s actually easier than brushing your teeth. Because it’s not something you should exercise to just make you look more beautiful,” Cena said.
“It’s something you should exercise to allow you to be who you are for a longer period of time.”
Have We Been Peeing Wrong? Turns Out There Is A Right And Wrong Way To Do It

Credits: Canva
A viral social media video warning against “power peeing”, pushing while urinating, has opened up a surprising discussion: many of us may be using the bathroom in ways that can harm our bodies. Pelvic health experts say there is, in fact, a right and wrong way to pee, and the wrong habits could cause lasting problems.
Why Bathroom Habits Matter
While urination seems automatic, the way you do it can have long-term effects on the bladder and pelvic floor muscles. The pelvic floor acts like a hammock, supporting organs such as the bladder, uterus, and bowels.
For urination to happen, these muscles need to relax so the bladder can squeeze urine out. If the process is disrupted, by straining, holding too long, or going too often, it can weaken muscles, interfere with bladder signals, and contribute to pelvic floor dysfunction.
This dysfunction can lead to urinary leakage, incomplete emptying, urinary tract infections, sexual difficulties, and pelvic organ prolapse, where pelvic organs shift out of their normal position.
Habits That Can Harm Pelvic Health
Experts point to several common but harmful urination habits:
Pushing to Pee: Trying to speed things up by straining actually tightens the pelvic floor instead of relaxing it. Over time, this can result in incomplete emptying, post-void dribbling, and difficulty coordinating the bladder and pelvic muscles.
Hovering Over the Toilet: Often done in public restrooms to avoid contact with surfaces, hovering engages hip and leg muscles, making pelvic relaxation difficult. This can leave urine behind in the bladder and raise the risk of infections.
Peeing “Just in Case”: Going to the bathroom before the bladder is full trains it to signal the need to urinate with smaller volumes, leading to overactive bladder and frequent urges.
Holding It Too Long: Ignoring the urge can overstretch the bladder, reduce elasticity, and make the brain less responsive to bladder signals. This increases the risk of bacterial buildup and infections.
Peeing in the Shower: Standing can make it harder for some people, particularly those with pelvic floor dysfunction or certain prostate issues, to fully empty the bladder. It can also condition the body to associate running water with the urge to urinate.
Why You’ll Never Be Completely “Empty”
The bladder is continuously filling with urine, so it will never be completely empty. Forcing out the last drops by pushing is unnecessary and can cause more harm than good.
How to Pee the Right Way
Experts say healthy urination habits can be learned and practiced:
Belly Breathing: Sit on the toilet, lean forward slightly, and breathe deeply from the belly. This encourages the pelvic floor to relax so urine flows naturally.
Reverse Kegels: Instead of squeezing and lifting, focus on releasing and opening the pelvic muscles as you exhale.
Double Voiding: After finishing, stand up briefly and then sit down again to allow the bladder to finish emptying.
Shift Your Position: Gently moving the hips can help the bladder release more urine without straining.
Track Your Patterns: Keep a three-day “pee diary” to monitor timing, fluid intake, and urges. Ideally, aim to urinate every two to four hours in the day and no more than twice at night.
When to Seek Help
If issues such as leakage, frequent urges, or difficulty emptying persist, consulting a pelvic floor therapist or urologist is recommended. With proper guidance, it is possible to retrain the bladder and muscles for healthier urination.
Ultimately, the simplest advice is to sit, relax, and let the body do its job naturally, no pushing, no rushing, and no multitasking on the phone. Your bladder, it turns out, prefers a calm, unhurried routine.
US Schools Reopen: Here Is Your Guide To The Lifesaving Vaccines Every Child Should Have

National Immunisation Awareness Month: Alongside the excitement of meeting new teachers and friends, the start of the US school year will also bring runny noses, hacking coughs, and bugs that somehow make their way through the entire classroom in a week. If you are sick, it is important to stay home. With a lot of people touching the same thing and germs everywhere, it is just important to watch your child's health and make sure to not spread it to other people.
Of course, handwashing, covering coughs and sneezes with a tissue or elbow, avoiding close contact with sick people, and regularly disinfecting frequently touched surfaces like doorknobs and de the first and necessary steps of everyday disease prevention. But there is another powerful shield that should not be ignored at any cost: vaccines.
Vaccines are not just for babies. They are a long-term health investment that keeps everything from the common flu to life-threatening infections at bay. Vaccines work; they help prevent diseases, and they help prevent infections. When enough people in a community are vaccinated, it creates herd immunity, meaning even those who cannot be vaccinated (due to medical reasons) get indirect protection.
Yes, there are conversations and concerns around vaccines, but the best way to clear the air is to get accurate, up-to-date information from trusted sources.
Here is Centres for Disease Control and Prevention (CDC) age-by-age vaccine cheat sheet
- At birth: The journey starts right away with the first dose of the Hepatitis B (HepB) vaccine, which protects against a serious liver infection.
- At 2 months: It is a busy month for tiny humans. They get doses of DTaP (Diphtheria, tetanus, and Pertussis), Hib (Haemophilus influenzae type b), IPV (Polio), PCV (Pneumococcal), and RV (Rotavirus).
- 4 months: Time for round two of the same five vaccines, because immunity is built gradually.
- 6 months: Another wave of protection with more DTaP, Hib, IPV (if needed), PCV, and RV doses. This is also when flu vaccines can be taken, and they will be recommended annually thereafter.
- 12–15 months: A milestone moment! Toddlers get the MMR (Measles, Mumps, Rubella), Varicella (Chickenpox), and HepA (Hepatitis A) vaccines. Some of the earlier series, like Hib and PCV, are also completed here.
- 15–18 months: The final DTaP dose in this stage rounds out protection against those three bacterial infections.
- 4–6 years: The finale before they head deeper into the school years; boosters for DTaP, IPV, MMR, and Varicella to ensure immunity stays strong.
Why this timing matters
Spacing out vaccines is not about convenience; it is about giving the immune system the right cues at the right time. Too early, and the body might not respond effectively; too late, and there is a risk window where the child is vulnerable. That is why following the schedule is important.What do vaccines do?
Vaccines do not just protect your child; they protect your child’s classmates, teachers, grandparents, and the stranger next to them. With schools reopening, the mix of close contact, shared surfaces, and high-energy kids is a perfect chance for germs to hop from one host to another.
Vaccines are not about fear; they are about freedom. Freedom from the diseases that once claimed far too many young lives. They work quietly so your kids can focus on learning their ABCs, art, and running the school playground without worry. It is time to take a moment to check that your child’s vaccine schedule is up to date.
Explained: An Overview Of How Vaccine Policies Have Changed Under RFK Jr

Credits: AP and Canva
When RF Kennedy Jr took over HHS, he promised he would not “take away” Americans’ vaccines. In practice, though, his office has made a string of moves that reshape who is recommended to get which shots, who decides those recommendations, and where federal vaccine money goes.
The changes so far include replacing the federal vaccine advisory panel, narrowing some COVID vaccine guidance, removing a flu preservative from recommendations, pulling funding for certain mRNA vaccine projects, and ordering new reviews of the childhood shot schedule.
These moves matter because federal recommendations and HHS approvals strongly influence insurance coverage, which vaccines are stocked in clinics and pharmacies, and what doctors tell patients.
New management: what happened to the advisory panel
One of Kennedy’s first major steps was to remove the existing members of the Advisory Committee on Immunization Practices, or ACIP. ACIP is the independent panel that for decades has advised the Centers for Disease Control (CDC) on who should get which vaccines and when.
READ: Top U.S. Medical Associations Ousted from CDC Vaccine Workgroups in Sudden Shake-Up
Kennedy dismissed the 17 sitting members and installed a much smaller, handpicked panel. He said the old committee had conflicts of interest and was not trusted by the public.
Critics say the move breaks long-standing safeguards meant to keep scientific review independent and transparent. The change also shifted which outside experts are invited to brief the committee and who sits on the working groups that prepare the technical evidence.
COVID-19 shots: who is recommended to get them now
Under Kennedy, federal guidance on COVID-19 vaccination has narrowed in key ways:
For healthy children and for people who are pregnant, the government removed the blanket “routine” recommendation and moved to a weaker status.
HHS announced that healthy children and pregnant women are no longer on the routine immunization schedule, saying these groups should make decisions in discussion with their doctors.
READ: CDC No Longer Recommends COVID Vaccine For Kids And Pregnant Women - What Do Experts Think?
That change was public and political, and it happened before ACIP had a formal vote. Medical groups such as the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics criticized the move and warned it would cause confusion.
Separately, the Food and Drug Administration (FDA) has signaled that approval will be focused on older adults and people at high risk for severe disease. The FDA’s guidance narrows the groups for which updated COVID shots can be authorized unless vaccine makers run larger trials or meet new evidence requirements. That means many healthy adults and children may not be covered or prioritized for the updated shots unless ACIP or HHS changes course later.
READ MORE: New Covid-19 Vaccine Policies Are Already Blocking People From Getting Shots—Who Is At Real Risk?
Why this matters: when the CDC labels a vaccine as “recommended,” insurance plans and public programs usually pay for it. Removing routine recommendations or narrowing approvals can make shots harder or more expensive to get, and can change what pharmacies and health centers stock. That creates practical barriers for people who might otherwise want or need protection.
Flu shots and thimerosal: a controversial preservative ban
At an ACIP meeting under Kennedy’s new appointees, the committee voted to recommend that seasonal influenza vaccines used in the U.S. be free of the preservative thimerosal.
READ: RFK Jr. Orders Thimerosal Removed From All US Flu Shots
HHS adopted that recommendation.
Thimerosal contains ethylmercury and has long been a focus of concern among vaccine skeptics even though public health agencies have found no credible evidence that it causes autism or long-term harm at the tiny amounts historically used in multi-dose vials.
In the United States most flu doses are already supplied in single-dose syringes that do not contain thimerosal, but some clinics and global programs still use multi-dose vials because they are cheaper and easier to ship. Removing thimerosal from U.S. recommendations could raise costs and complicate access for settings that rely on multi-dose vials, like some rural clinics and international programs.
READ MORE: Former Anti-Vaccine Leader to Weigh In On CDC Vaccine Strategy
What the agencies said: HHS and the new ACIP members framed the choice as restoring public trust and eliminating a preservative that activists have long criticized. Critics point out that the science does not support that thimerosal at vaccine doses causes harm, and they worry removing it will reduce vaccine availability or increase price without improving safety.
Respiratory syncytial virus, or RSV: more access for some ages, new options for infants
Two big RSV moves happened during this period:
For infants, the CDC advisory group recommended a second long-acting monoclonal antibody product, clesrovimab (brand name Enflonsia), to prevent severe RSV disease in babies under eight months who are not protected by maternal vaccination.
READ: New Recommendations Made On RSV, Meningitis, And Chikungunya Vaccines
The FDA had already approved the product and ACIP voted to include it so it can be used and covered for infants entering their first RSV season. Having a second product helps guard against shortages and can lower costs over time.
For older adults, ACIP recommendations were expanded so that adults in their 50s with high-risk conditions can receive an RSV vaccine. Kennedy signed off on accepting the advisory committee’s recommendation for that broader high-risk group. That change means people in their 50s with specific health problems may now be eligible for RSV shots.
Childhood schedule review
One of the most notable policy shifts is the new panel’s decision to examine the cumulative health effects of the entire childhood immunization schedule. That means ACIP will look again at the timing and combination of routine childhood vaccines that, for decades, have been recommended to protect children against measles, polio, pertussis, hepatitis B, and many other diseases. The committee also signaled possible re-examination of specific items such as the birth dose of hepatitis B and the combined MMRV vaccine that mixes measles, mumps, rubella and varicella.
Supporters of the review say it is a reasonable recheck. Critics say the review is driven by unfounded concerns and risks undermining long-standing, evidence-based prevention.
READ: FDA Approves New Covid Vaccine For Kids With Selective Eligibility
Why people are worried: federal recommendations guide school vaccine rules, insurance coverage, and what pediatricians routinely offer. Even talk about changing the schedule or re-opening decisions that were closed decades ago can trigger parents’ doubts and lead to lower vaccination rates. That is especially concerning during a resurgent measles outbreak in parts of the country. Public health groups and pediatricians have pushed back strongly.
HPV, MMRV, Hepatitis B and other specific vaccines
Several single-vaccine items that were moving through the advisory pipeline have been delayed or placed under further review:
HPV: A planned vote that would have moved the routine recommendation window earlier, to routinely recommend vaccination starting at age 9 instead of 11, was removed from the agenda. That delay left clinicians and program planners uncertain about the future of younger-age recommendations. Kennedy has prior legal involvement in litigation related to the HPV vaccine that adds context to the committee’s caution.
READ: Who Needs HPV Vaccine? Guide For Every Parent, Teen And Adult
MMRV (the combined measles-mumps-rubella-varicella shot): the new panel signaled it would weigh the risks and benefits of the combination vaccine, in part because of data on rare febrile seizures in very young children. Pediatricians say the increased seizure risk is small and generally benign, but the panel’s attention to the issue has stirred fresh debate.
READ: Amid Measles Outbreak, Texas Makes Vaccine Exemption Easier For Kids
Hepatitis B at birth: ACIP said it will review whether the birth dose for infants should remain routine when the mother tests negative. The American Academy of Pediatrics strongly defends the birth dose because it prevents lifelong hepatitis B infections. The review has alarmed many clinicians who see no credible evidence that newborns are at low enough risk to change the practice.
READ: Can A Quick Visit To A Salon Increase Your Risk Of Hepatitis B?
Money and research: mRNA funding pulled or reshaped
HHS under Kennedy announced a large shift in federal investments tied to mRNA vaccine development. The department moved to wind down or restructure a set of BARDA and other contracts that supported mRNA vaccine projects, including high-profile programs aimed at pre-pandemic influenza and other threats. The cited reason was concern about the platform’s effectiveness for upper respiratory infections and a stated desire to invest in what the department calls “broader” or alternative vaccine technologies. Scientists warn that pulling this money risks hampering rapid-response vaccine capacity in future outbreaks. Industry groups and researchers have pushed back, noting that mRNA technology enabled the rapid COVID-19 response and remains a major tool for future pandemics.
Legal fights, professional pushback, and the practical fallout
Several national medical organizations and public health groups have publicly protested or taken legal steps to challenge Kennedy’s changes. In July a coalition led by the American Academy of Pediatrics, along with other large medical societies and public health organizations, filed a lawsuit seeking to reverse the HHS directive that removed COVID-19 vaccines for healthy children and pregnant women from routine recommendations. Other associations were removed from vaccine workgroups, which has raised concerns about sidelining established expert voices. Meanwhile, some pharmacies and clinics began to report confusion about whether to offer COVID shots to pregnant women or healthy kids, and whether insurers would cover them.
Who keeps easy access, who might lose it, and what to watch
Right now access looks most secure for people the new guidance and approvals clearly protect: older adults and people with underlying health conditions are largely still being recommended for key vaccines like COVID boosters and RSV shots. For healthy children and some healthy adults, access has become more uncertain because of narrower recommendations and the potential insurance implications.
© 2024 Bennett, Coleman & Company Limited

