Memory Issues In Dementia & Parkinson’s Patients Linked To Natural Mouth & Gut Bacteria
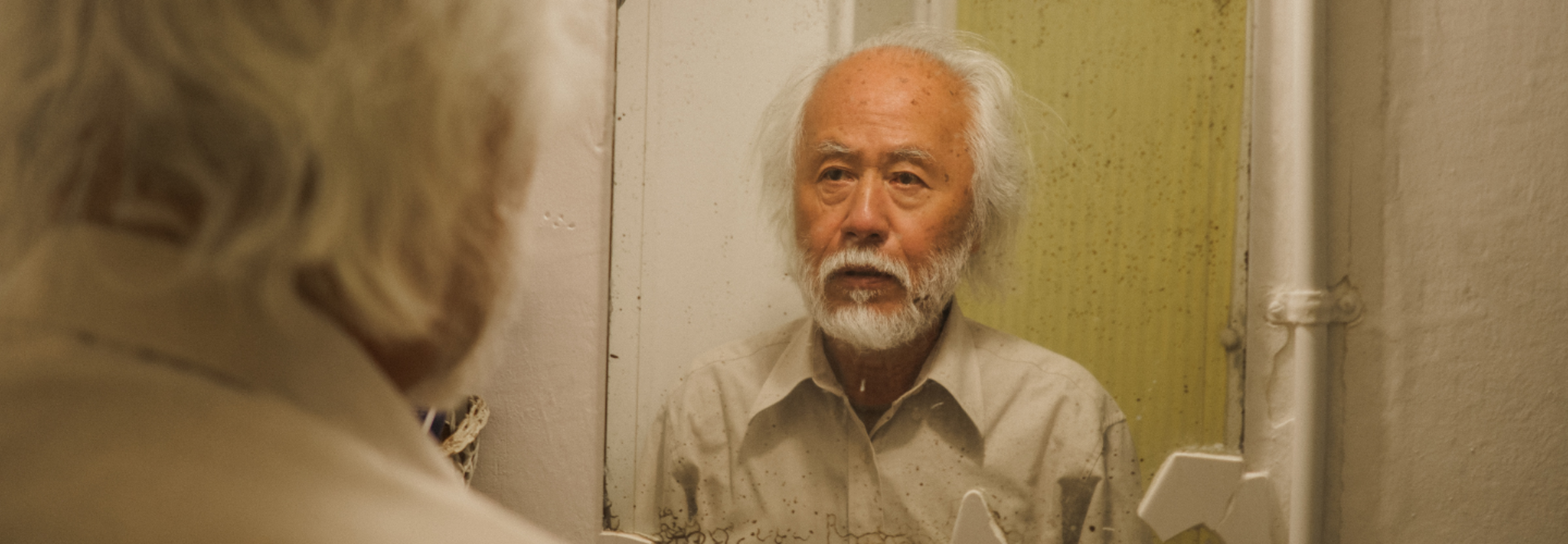
(Credit-Canva)
SummaryDementia affects many people worldwide, and scientists are still looking for ways to cure it, which entails first finding what exactly causes it. A new study has linked dementia to a certain bacteria most of us have.
End of Article
