- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Migraines In Women: How Hormones Influence Neurological Health

Migraines In Women: How Hormones Influence Neurological Health
For those who have not experienced a migraine, perhaps it would seem just another headache. But for someone like me who has suffered through migraines that will last over a week even with medication, I can definitely tell you that it's much more. The ache is not confined to the head; it's the whole experience. Nausea, sensitivity to light, and throbs so bad it makes simple tasks unbearable. It also comes with an emotional burden—the loneliness and frustration are pretty unbearable. Through the years, realizing how hormones are also implicated in triggering and exacerbating my migraines has helped change the game in my dealing with these episodes.
What are Hormonal Migraines?
Hormonal migraines are caused by fluctuations in estrogen and progesterone, the two main female hormones. These hormones are essential for the reproductive system, regulating menstrual cycles and pregnancy. They also have an effect on brain chemicals, such as serotonin and dopamine, which affect mood and pain perception. When hormone levels fluctuate, such as during menstruation, pregnancy, or menopause, they can destabilize the pathways in the brain, causing migraines.
According to Dr. Shivananda Pai, Consultant Neurology, migraines are more than a neurological disorder. "Migraines represent a complex interplay of genetic, environmental, and hormonal factors. In women, hormonal fluctuations are a critical trigger that amplifies sensitivity to pain," he explains. Hormonal headaches are particularly challenging because they are influenced by multiple life stages, from puberty to post-menopause. Common causes include:
- Menstrual periods: Estrogen levels significantly drop just before menstruation often triggers a migraine.
- Pregnancy: Hormones can act to relieve symptoms or aggravate them during different times of pregnancy.
- Menopause: The hormonal fluctuation during menopause can intensify a migraine, while some women tend to find relief.
- Hormonal therapies: Birth control and HRT tend to level off hormone balances in some individuals but will exacerbate a migraine in others.
Complex Role of Hormones in Women’s Neurological Health
Estrogen and Neurological Health
Estrogen, often called the "hormone of femininity", does more than regulate reproductive functions. It is a powerful influencer of brain health. Estrogen modulates the activity of neurotransmitters like serotonin, which regulates mood and pain perception, and dopamine, associated with reward and pleasure.
During stages of hormonal stability, like in pregnancy's latter months, women may have fewer migraines because of the steady elevation of estrogen. However, a sudden downfall in estrogen destabilizes these chemicals in the brain, sending a heightened sensitivity for migraine triggers.
Menstrual Migraines
The most common form of hormonal migraines is menstrual migraines, which occur in response to the steep decline in estrogen levels just before menstruation. These are typically more intense and less responsive to standard treatment. The timing of these migraines provides clear evidence of the role hormones play in neurological health.
Pregnancy and Hormonal Shifts
Pregnancy is a rollercoaster of hormones. Although many women experience relief from migraines as a result of the constantly elevated levels of estrogen, some women, particularly in the first trimester, worsen. This individual variability is a characteristic of hormonal migraine triggers.
Hormonal Therapies and Management of Migraine
Hormonal treatments, such as oral contraceptives and HRT, have had mixed reviews regarding their use in managing migraine. Some women fare better with the stabilization the treatment provides, whereas others suffer worsening symptoms. This will depend on the nature and dose of the hormones used.
Post-Menopause: Migraine Remission or Continued Struggles?
For most women, menopause brings relief from their migraines. The decline in frequency and severity often accompanies stability in hormone levels. Even so, the susceptibility remains with some towards other forms of triggers including stress and sleep deprivation, not to forget diet-related factors and continues the saga of migraines well after the menopausal stages.
Effect on Neurological Health Due to Hormonal Changes
The relationship of hormones to neurological health goes beyond migraines. Hormonal changes have profound effects on a woman's brain in general.
Mood Disorders: Estrogen helps stabilize mood by regulating serotonin. Its decline at menopause increases the risk of mood swings and depression.
Neurodegenerative Diseases: Estrogen is neuroprotective, stimulating the growth and repair of brain cells. Its absence in post-menopausal women has been associated with an increased risk of Alzheimer's disease and cognitive decline.
Multiple Sclerosis (MS): Hormonal cycles may affect the course of MS, a disease that occurs more frequently in women than in men. Estrogen's anti-inflammatory effects provide transient protection during pregnancy, reducing relapse rates in women with MS.
"The intricate interplay between hormones and neurological health underscores the need for gender-specific treatment approaches," says Dr. Pai.
Managing Hormonal Migraines: Practical Strategies
While hormonal changes are inevitable, several strategies can help manage migraines effectively:
1. Tracking Your Cycle
Understanding your menstrual cycle can help identify patterns and predict when migraines might occur. This knowledge allows for preventive measures, such as scheduling medications or adjusting lifestyle habits.
2. Consulting Specialists
Working with a neurologist or gynecologist can help develop a personalized treatment plan. Options might include hormonal therapies, triptans, or preventive medications tailored to your specific needs.
3. Adopting a Healthy Lifestyle
A well-balanced diet, regular exercise, and stress management are all integral parts of managing migraines. For instance, magnesium-rich foods and hydration can help reduce the frequency and severity of attacks.
4. Exploring Preventive Therapies
For people with severe or frequent migraines, preventive medications, such as beta-blockers or CGRP inhibitors, may be prescribed. These medications stabilize brain activity and therefore reduce the chances of migraine during hormonal fluctuations.
5. Mind-Body Techniques
Techniques like yoga, meditation, and biofeedback can enhance wellness and reduce the debilitating effects of stress-one of the most common migraine triggers.
Research that was once in its embryonic stage continues to shed more light on the role of hormones in migraines and other neurological conditions. Further breakthroughs in genetic testing might enable doctors to predict, at least in a way, how an individual would react to hormonal therapies. The importance of gender-specific approaches is gradually being realized, which involves differentiating between the plight of women with migraines from others.
As Dr. Pai puts it, "Empowering women with knowledge about the hormonal underpinnings of migraines can lead to better, more personalized care. With the right strategies, migraines can be effectively managed, allowing women to lead fuller, healthier lives.
Migraines are not headaches; they are a complex neurological condition that deeply impacts the lives of millions of women. Understanding the role of hormones in triggering and exacerbating migraines is a vital step toward better management and relief.
Awareness, proactive care, and advances in medical research can help women regain their lives from the grip of hormonal migraines. Whether tracking cycles, adopting healthier habits, or seeking tailored medical care, every step taken toward understanding and managing migraines is a step toward empowerment.
Dr Shivananda Pai is a Consultant Neurology at KMC Hospital Dr B R Ambedkar Circle in Mangalore, India.
Brandes JL. The Influence of Estrogen on Migraine: A Systematic Review. JAMA. 2006;295(15):1824–1830. doi:10.1001/jama.295.15.1824
Sacco S, Ricci S, Degan D, Carolei A. Migraine in women: the role of hormones and their impact on vascular diseases. J Headache Pain. 2012 Apr;13(3):177-89. doi: 10.1007/s10194-012-0424-y. Epub 2012 Feb 26. PMID: 22367631; PMCID: PMC3311830.
Unique Symptoms Of Vitamin D Deficiency

Credits: Canva
Long winters and lack of sunlight has renewed attention on vitamin D deficiency, a condition closely linked to bone health and overall well-being. Health data show that the problem is far more widespread than many realize, with potential consequences that range from brittle bones to mood changes.
Vitamin D and Its Role in the Body
Vitamin D plays a crucial role in helping the body absorb calcium, an essential mineral for strong bones and teeth. Without enough vitamin D, calcium absorption drops, weakening bone structure over time. This increases the risk of fractures, particularly among older adults.
Beyond bone metabolism, vitamin D also supports muscle function and contributes to a healthy immune response. Researchers have also explored its influence on mental well-being, as vitamin D receptors are present in several areas of the brain.
Deficiency Affects a Large Section of Adults
According to figures from the Robert Koch Institute, around 30 percent of adults in Germany have insufficient vitamin D levels. This is striking, given that the vitamin is produced by the body when skin is exposed to sunlight.
Experts point to modern lifestyles as a key reason. Many people spend most of their day indoors, often working in offices with little exposure to natural light. Seasonal factors also play a role, as sunlight is weaker and less frequent during autumn and winter months. In such conditions, relying on sunlight alone is often not enough to maintain healthy vitamin D levels.
Can Diet Help Fill the Gap?
Food can support vitamin D intake, although it usually provides smaller amounts compared to sunlight. Fatty fish are among the best dietary sources. Salmon, herring, eel, tuna, and pike perch contain relatively high levels of the vitamin and are often recommended for people at risk of deficiency.
Other animal-based options include eggs, liver, beef, and butter. For those who avoid animal products, plant-based sources can contribute modest amounts. Mushrooms, spinach, kale, broccoli, and Brussels sprouts are commonly mentioned. Some fruits such as avocados, kiwis, oranges, bananas, and figs are also included in vitamin D-friendly diets, though their contribution is limited.
Read: Vitamin D Supplements Under Scrutiny As It Fails Safety Test
Because many of these foods are eaten infrequently, especially fish, diet alone often fails to correct a deficiency.
Symptoms Linked to Low Vitamin D Levels
Vitamin D deficiency can show up in different ways. Many people report persistent fatigue, low mood, or depressive symptoms. While studies support a connection, researchers note that the exact biological pathways are still being studied.
Physical signs are often related to bone health. Weakened bones can increase the risk of fractures and cause general bone pain. Digestive issues and reduced tolerance to certain foods have also been reported in some cases. A deficiency is usually confirmed through a blood test ordered by a doctor.
When Too Much Becomes Harmful
While deficiency is common, excessive vitamin D intake can also pose risks. Health experts stress that overdoses do not occur through sunlight or normal diets, but through high-dose supplements taken over time.
Too much vitamin D can raise calcium levels in the blood, a condition known as hypercalcemia. This may lead to kidney damage, heart rhythm problems, and calcification of blood vessels. Individual risk varies depending on factors such as body weight, metabolism, and alcohol consumption, making medical guidance essential before supplement use.
Breast Cancer Signs That Do Not Feel Like Cancer, Explain Doctors

Credits: iStock
On World Cancer Day 2026, we at Health and Me is focussing on the most common cancer among women in India. Breast Cancer, which accounts for over 216,000 new cases every year, as per the 2022 data. This means, 28.2 per cent of female cancers are attributed to breast cancer. What is more tragic is that one woman is diagnosed with breast cancer every four minutes, and one dies every eight minutes in the country.
While, we all know that finding a lump is the red flag, there are other signs that women often miss that delays their detection. Health experts are increasingly warning that this narrow understanding may be delaying early diagnosis for many patients. New medical insights suggest that several lesser-known changes in breast tissue, skin and nipple appearance may signal cancer but often go unnoticed or get dismissed as harmless hormonal changes.
Read: More Than A Diagnosis: Cancer Survivors Share The Small Wins That Helped Them Heal
Breast Cancer Is Not Just A Lump
Data from a consumer survey commissioned by The Ohio State University Comprehensive Cancer Center shows that 93 percent of adults identify a lump as a symptom of breast cancer. But fewer than half are aware of several other warning signs that could appear much earlier.

Experts warn that this knowledge gap can be risky because not all breast cancers form lumps that are easily felt. Breast medical oncologist Ashley Pariser explains that screening mammography remains the most effective tool for detecting breast cancer at its earliest and most treatable stages. She adds that being familiar with the normal look and feel of one’s breast tissue helps people detect subtle changes faster and seek timely medical care.
Pariser notes that many breast changes can occur due to aging or childbirth. Still, she stresses that breast cancer can present in multiple ways, making it important for individuals to report unusual symptoms without delay.
Signs That Should Not Be Ignored
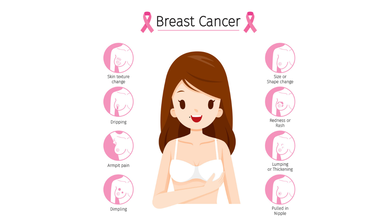
According to Dr Kanchan Kaur, Oncoplastic Breast Surgery Specialist, structural changes in the breast are among the most overlooked early warning signs. She highlights that while lumps are common indicators, deformations in breast shape such as flattening, indentation or dimpling should not be ignored.
Read: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Dr Kaur also points out that an unusual increase or decrease in breast size, particularly when it affects only one breast, and sudden changes in breast symmetry may signal an underlying issue. She advises that these signs warrant clinical evaluation even if they appear painless or gradual.
Another concerning sign is skin texture change. She explains that a reddish, pitted texture resembling the surface of an orange or a marble-like area under the skin can indicate deeper tissue abnormalities. Any area of the breast that looks or feels noticeably different from surrounding tissue should be assessed by a doctor.
Nipple Changes Can Be Early Red Flags
Both research findings and clinical observations highlight nipple changes as key indicators that are often missed. Survey results from Ohio State University show that only about one-third of respondents recognized nipple inversion or retraction as a symptom of breast cancer.
Dr Kaur notes that nipples can provide early clues about breast disease. Symptoms such as newly inverted nipples, dimpling around the nipple, scaly red rashes, burning or itching, and ulceration should prompt medical attention.
Read: Oncologists Warns Of The Cancer Rising Among Women in India
Clear or bloody nipple discharge that is unrelated to pregnancy or breastfeeding is another warning sign. While discharge can occur due to benign causes, experts recommend prompt evaluation to rule out cancer.
Specialists at Moffitt Cancer Center caution that symptoms such as breast tenderness, swelling or changes in fullness are often mistaken for routine hormonal fluctuations. Because these symptoms frequently overlap with premenstrual changes, many women delay consulting a specialist.
Experts from the center advise that persistent breast pain, swelling or unusual fullness that does not resolve within a few days should be medically evaluated. They emphasize that sudden nipple inversion, discharge or skin texture changes require immediate attention.
World Cancer Day 2026: India’s 10 Most Common Cancers, Explains Doctor
Credits: Canva
Cancer trends in India are changing rapidly, driven by lifestyle patterns, environmental exposure, infections, and limited access to early healthcare in some regions. According to Dr Puneet Gupta, Chairman of Oncology Services at Asian Hospital, understanding early warning signs and adopting preventive habits can significantly improve survival outcomes.
“Cancer patterns in India are the results of multiple factors ranging from lifestyle, environmental exposure, infections and access to timely care,” Dr Gupta explained, adding that early symptoms can appear months or even years before the disease reaches advanced stages.
Breast Cancer: The Most Common Cancer In Women
Dr Gupta noted that breast cancer is frequently seen in women, especially after the age of 40. He highlighted that the disease often develops silently and without pain.
He explained that warning signs may include lumps in the breast or under the arm, changes in breast shape, skin dimpling, inward turning of the nipple, or unusual discharge. “Do not ignore these changes,” he cautioned. Regular self-examination, along with timely imaging tests such as mammography, ultrasound, or MRI, can help detect breast cancer early.
Cervical Cancer: Strongly Linked To HPV Infection
Cervical cancer mainly affects women between 30 and 60 years. Dr Gupta emphasised that HPV infection remains the leading risk factor. Early symptoms can include abnormal vaginal bleeding, bleeding after intercourse, or persistent pelvic pain, although early stages often remain symptom-free.
He stressed that routine Pap smear screening and HPV vaccination play a crucial role in prevention and early diagnosis.
Lung Cancer: Rising Risk Beyond Smoking
While lung cancer remains more common in men, Dr Gupta pointed out that cases among women are rising as well. Smoking is the primary cause, but exposure to fine particulate air pollution (PM2.5) also contributes to the risk.
He warned that persistent cough, chest pain, breathing difficulty, unexplained weight loss, or coughing blood require immediate medical evaluation, particularly in people with a history of tobacco use.
Oral Cancer: A Major Concern In India
Oral cancer remains widespread due to tobacco, gutka, areca nut consumption, and HPV infection. Dr Gupta explained that long-lasting mouth ulcers, red or white patches inside the mouth, jaw stiffness, or swallowing difficulty are early red flags. Regular dental and oral examinations can help detect early cancerous changes.
Colorectal Cancer: Lifestyle-Linked Risks
According to Dr Gupta, colorectal cancer is increasingly being diagnosed in adults around 40 years of age. Sedentary lifestyles, low-fiber diets, and excessive red meat intake are major contributing factors.
He said symptoms such as blood in stool, persistent bowel habit changes, abdominal pain, or unexplained anaemia should not be overlooked. Early screening and genetic testing in high-risk individuals can significantly improve outcomes.
Stomach Cancer: Often Shows Subtle Symptoms
Dr Gupta explained that stomach cancer may initially present as indigestion, early fullness, nausea, or unexplained weight loss. It is often associated with long-term Helicobacter pylori infection, smoking, and salt-heavy diets. Persistent digestive discomfort warrants medical attention.
Prostate Cancer: Common But Often Slow Growing
Prostate cancer typically affects men above 50 and usually progresses gradually. Dr Gupta noted that difficulty urinating and frequent nighttime urination are common early symptoms. Regular check-ups help detect the disease before complications arise.
Esophageal Cancer: Linked To Lifestyle And Nutrition
Tobacco use, alcohol consumption, poor nutrition, and iron deficiency increase the risk of esophageal cancer. Dr Gupta advised that swallowing difficulty, chest discomfort, or unexplained weight loss should prompt evaluation through tests like endoscopy or barium swallow.
Ovarian Cancer: Often Missed Due To Vague Symptoms
Dr Gupta explained that ovarian cancer frequently goes undetected due to non-specific symptoms such as bloating, abdominal discomfort, or early satiety. Women with persistent symptoms, particularly those with a family history of breast or ovarian cancer, should seek medical evaluation.
Liver Cancer: Screening Is Crucial For High-Risk Groups
Liver cancer often develops in individuals with chronic liver disease. Symptoms such as jaundice, abdominal swelling, or persistent pain usually appear late. Dr Gupta stressed that hepatitis vaccination and screening among high-risk groups are vital for prevention.
Lifestyle Changes And Screening Can Reduce Risk
Dr Gupta emphasized that although cancer cannot be completely prevented, a significant proportion of cases are linked to modifiable risk factors. Avoiding tobacco, maintaining a healthy weight, consuming balanced nutrition, managing stress, and staying physically active can lower risk.
He added that vaccinations against HPV and hepatitis further reduce cancer risk, while regular screening helps detect cancers at pre-cancer or early stages. “Education, prevention and early detection make the difference between late-stage disease and long-term survival,” Dr Gupta concluded.
© 2024 Bennett, Coleman & Company Limited

