- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Most Women Do Not Know This One Neurological Risk Of Menopause, According To Neurosurgeon

(Credit-Canva)
Symptoms of menopause vary a lot, and many people do not know just how many ways menopause can affect a woman’s health. To explain it, Dr Jay Jagannathan, board-certified neurosurgeon pointed out how menopause can also neurologically affect women as well.
Menopause is the natural end to the reproductive years of a woman. However, what most people are not aware of is the way menopause can affect a woman’s health. In fact, even women are not as informed about it. In a 2022 study published in the Women’s Health journal, in their survey of 738 women showed that over 80% of them had no knowledge or some knowledge of menopause. This revealed that most women under 40 have limited education of menopause.
To tackle this, a lot of doctors like Dr Jagannathan take to social media and help educate more people about it.
Does Menopause Affect The Brain?
In the video caption, Dr. Jagannathan explained that when people talk about menopause, they usually focus on hot flashes, changes in mood, or concerns about bone thinning. But what's often missed is the major effect hormonal changes have on your brain. He further explained how estrogen is more than just a reproductive hormone—it functions as a neuroprotective shield for the brain.
- It plays a key role in regulating blood flow.
- It helps reduce inflammation.
- It actively protects brain cells from stress and damage.
When estrogen levels decline significantly during and after menopause, this vital protection weakens, leaving the brain more vulnerable.
How Does Hormone Decline Put Women At Neurological Risk?
When estrogen levels fall sharply during the menopausal transition, this vital protection is lost, which is why we see a rise in specific brain issues:
Increased Risk of Silent Strokes
A silent stroke is a tiny blockage in the brain's blood vessels that you usually don't notice. Over time, these small blockages add up and quietly damage areas of the brain, leading to problems with memory and thinking. Without estrogen's help to keep vessels healthy, these silent strokes become more common.
Accelerated Memory Decline
Memory is often the first thing affected. Women may notice they are more forgetful, have trouble finding the right words, or feel mentally "slow." This is partly because the areas of the brain responsible for memory are very sensitive to the drop in estrogen.
Risk of Alzheimer’s Disease and Persistent Cognitive Fog
Cognitive fog is that temporary feeling of being mentally fuzzy or unable to concentrate. Alzheimer's is a serious disease that causes severe memory loss. The loss of estrogen's protection is a major risk factor that increases the chances of developing Alzheimer's and experiencing chronic brain fog decades later.
How Can You Protect Your Brain During Menopause?
Dr Jagannath assures that it can be controlled. We can proactively manage this biological reality. Based on my clinical guidance, here are essential steps to safeguard your brain health:
- Control blood pressure and cholesterol, the health of the brain's vessels relies on it.
- Maintain consistent physical and mental activity.
- Focus on achieving restorative, high-quality sleep.
- Talk to your doctor about your hormone levels and overall vascular health; early monitoring is crucial.
He concluded the post by warning not to wait until problems start. Discussing your menopausal symptoms, hormone levels, and risk factors (like a family history of heart disease or dementia) with your doctor allows for early intervention, which might include hormone therapy or other medications to protect your vessels and brain.
Doctors Said She Wouldn't Live Past 4: Woman Born Without A Brain Celebrates 20th Birthday

(Credit-WABI)
Born without a brain, Alex Simpson of Nebraska defied all odds by celebrating her 20th birthday recently; doctors said she wouldn’t live past age four. Alex’s remarkable milestone made the news headlines; her parents Shawn and Lorena Simpson, shared her inspiring story with local news outlet KETV.
Hydranencephaly is very rare, affecting an estimated 1 in 5,000 to 1 in 10,000 pregnancies.
Alex was born with a condition where most of her brain is missing. As her father, Shawn, explained, "Hydranencephaly means that her brain is not there." He noted that she only has a small portion of her cerebellum, about "half the size of my pinky finger"—in the back of her head, but little else.
Tragically, doctors initially told the family that Alex was not expected to live past the age of four.
Can A Person Live Without A Brain?
Hydranencephaly, according to the Cleveland Clinic, is most often fatal within the first year of life, making Alex’s 20th birthday an exceptional medical outlier and a true testament to her strength and her family's devotion.
Hydranencephaly is a very rare birth defect that affects the central nervous system. A baby born with this condition is missing a significant part of the brain called the cerebral hemispheres.
Missing Parts
The cerebral hemispheres are the two large, front halves of the brain (the cerebrum). These parts are responsible for higher functions like thinking, memory, and movement control.
Fluid-Filled Sacs
Instead of the actual brain tissue, there are large sacs filled with cerebrospinal fluid (CSF). This is the fluid that normally acts as a cushion for the brain and spinal cord.
Outlook
Because so much of the brain is missing, the condition is usually fatal either before birth or shortly afterward. Babies who survive often develop an enlarged head and have severe symptoms.
What Causes A Baby To Be Born Without A Brain?
The Cleveland Clinic explains that abnormal brain formation happens during early pregnancy and it can be caused by a birth defect, injury, or illness. The exact cause is unknown. Scientists suspect it might be inherited, but they don't fully understand the pattern. Some cases have been linked to exposure to harmful substances during pregnancy.
Does Hydranencephaly Have Symptoms?
A baby born with hydranencephaly might seem normal at first. Symptoms usually appear within the first few weeks or months:
Head Size: The head gets larger than normal.
Growth Problems: Failure to gain weight or grow well ("failure to thrive").
Muscle Issues: Muscles might be too stiff (rigid arms/legs) or have increased or decreased tone and twitching.
Basic Senses: Problems with seeing and hearing.
Breathing: Difficulty breathing.
How is Hydranencephaly Diagnosed and Treated?
It can be spotted during a prenatal ultrasound, which uses sound waves to check the baby. If hydranencephaly is suspected, an MRI might be used for clearer pictures of the missing brain tissue.
If it wasn't seen before birth, a doctor will make the diagnosis based on the baby's symptoms and a detailed brain MRI. Other tests like a CT scan, angiography, which is an X-ray of blood vessels, or genetic testing may also be used.
There is no cure for hydranencephaly. So, the treatment focuses on making the baby as comfortable as possible and managing the symptoms:
Fluid Management
Surgery to place a shunt, which is a thin tube, can drain excess fluid from the skull to reduce pressure, which helps manage the enlarging head, though its effectiveness is limited compared to hydrocephalus.
Medication
Antiseizure medications may be given to control twitching or spasms.
Supportive Care
This includes nutritional support (feeding), physical therapy to help with muscle problems, and sometimes a tracheostomy or ventilator if the baby has trouble breathing.
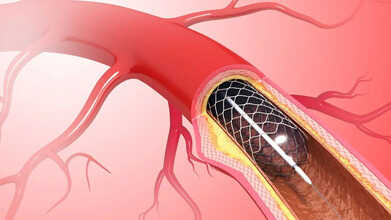
What Is Laser Angioplasty And How Can It Clear Blocked Arteries Faster?
Credits: Canva
In the past, heart problems were often seen as frightening and potentially fatal. While cardiac conditions remain serious, advances in heart medicine over recent years have dramatically improved treatment success and reduced risks. Among these modern options, lasers are proving to be highly effective. Laser angioplasty is one such procedure that allows cardiologists and vascular surgeons to remove plaque, a major cause of coronary artery disease and peripheral artery disease.
What Is Laser Angioplasty?
Laser angioplasty is a minimally invasive procedure where a laser is used to break down plaque inside arteries. Unlike traditional angioplasty, which uses a balloon to widen arteries, this method targets difficult or stubborn blockages that are hard to treat otherwise. A thin catheter carrying the laser is guided to the blocked area, where the laser vaporizes the plaque and restores blood flow. This technique can help patients avoid open-heart surgery and often leads to shorter hospital stays and quicker recovery, according to Stanford Health Care.
Laser Angioplasty Procedure
Before the procedure, a specialist—either an interventional cardiologist or vascular surgeon—evaluates the patient’s overall health and determines whether laser angioplasty is appropriate. As per NIH, Once approved, the process generally follows these steps:
- The patient is placed under general anesthesia.
- A small incision is made in the groin.
- Using X-ray imaging, a guide wire is inserted through the femoral artery to reach the blockage.
- A catheter is threaded over the wire to the site of the plaque.
- The laser is passed through the catheter to the blockage, where it vaporizes the fatty deposits. X-ray imaging and contrast dye are used to monitor the process.
- Once the plaque is cleared, the laser, catheter, and wire are removed, and the incision is closed.
- Patients are monitored afterward and, depending on their condition, may be able to go home the next day.
Advantages of Laser Angioplasty Over Traditional Methods
Laser angioplasty offers several benefits compared with conventional balloon angioplasty or bypass surgery. The laser can precisely vaporize plaque and thrombus, allowing treatment of chronic or heavily calcified blockages. This precision often results in shorter hospital stays and faster recovery, helping patients get back to normal life sooner.
For patients with in-stent restenosis or total occlusions, laser angioplasty can achieve results that might otherwise require multiple procedures or open-heart surgery. Its ability to target tough blockages makes it an invaluable tool in modern cardiac care.
Risks and Considerations
While laser angioplasty is generally safe when performed by experienced specialists, it does carry some risks. Similar to standard angioplasty, complications like hematoma at the catheter site, arterial perforation, or acute thrombosis can occur. Specific to the laser procedure, there may also be vessel injury, spasm, embolism, or bleeding
Patient selection is very important. The procedure may not be suitable for arteries that are extremely curved, tortuous, or involve the left main coronary artery. There is also a chance the artery may narrow again, requiring repeat procedures or bypass surgery. Despite these considerations, the benefits of laser angioplasty—including precise targeting and faster recovery—make it a promising option for many patients.
Hormone Replacement Therapy: When Is The Right Time To Start HRT After Menopause?

Credits: Canva
FDA menopause hormone therapy: The U.S. Food and Drug Administration announced on Monday that it will remove the strictest “black box” warnings from hormone therapies used to manage menopause symptoms. The move could make these treatments more accessible to women and healthcare providers, who have long avoided them due to safety concerns.
FDA Commissioner Marty Makary said the decision comes after a thorough review of scientific research, feedback from an expert panel in July, and a public comment period.
"After 23 years of outdated caution, the FDA is now stepping back from the fear-based messaging that has kept women from this life-changing—and sometimes,life-saving—treatment," Makary said at a press briefing.
"We are responding to women who have been challenging the paternalistic approach in medicine, and to female medical students calling for better menopause education in medical training," he added.
The agency is also greenlighting two new treatments for menopausal symptoms. This includes a generic version of Pfizer’s Premarin and a non-hormonal option for moderate to severe vasomotor symptoms, like hot flashes.
What Is Hormone Replacement Therapy?
Hormone replacement therapy (HRT) is a treatment for people experiencing menopause symptoms. Doctors may also call it hormone therapy (HT), especially when prescribed after age 50. Generally, “HRT” is used for people starting treatment at a younger age, often before 40.
During menopause, the ovaries produce less estrogen, which can lead to uncomfortable symptoms, including:
- Hot flashes
- Night sweats
- Vaginal dryness and painful intercourse
- Mood swings, irritability, or depression
- Insomnia
- Urinary incontinence
HRT works by replacing the hormones your body is no longer making enough of, helping to relieve these symptoms. It can also help prevent bone loss, such as osteoporosis and osteopenia, which can occur when estrogen levels drop.
Hormone Replacement Therapy: When Should You Start Hormone Therapy?
Dr. Joann Pinkerton, a menopause specialist at the University of Virginia Health, recommends starting estrogen therapy before age 60 or within ten years of the onset of menopause, which begins one year after your last period. Many women continue taking birth control through perimenopause, which can help manage hot flashes and night sweats as hormone levels fluctuate.
Once menopause is complete and pregnancy prevention is no longer a concern, continuing birth control may not make sense. “Birth control usually contains more estrogen than is used in menopause hormone therapy,” Pinkerton says, “so that’s a good time to discuss hormone therapy options with your provider.”
Menopause Hormone Therapy FDA: How Long Should You Be on Hormone Therapy?
Typically, women use hormone therapy for three to five years, though this is not a strict rule. “For those with ongoing symptoms or bone loss—which can be addressed with hormone therapy—we continue treatment,” Pinkerton explains. She emphasizes the importance of reviewing treatment annually. “It’s about working with each patient to find the safest and most effective approach.”
Lauren Streicher from Northwestern University, as per NPR, adds, “We don’t stop hormone therapy simply because three to five years have passed.” She notes that menopause symptoms can last longer for some women, with Black and Hispanic women often experiencing extended periods of discomfort.
HRT Therapy: Who Should Avoid Hormone Therapy?
Certain medical conditions can make hormone therapy risky. Women with estrogen-sensitive breast or uterine cancers, or those who have had, or are at high risk for heart attack, stroke, blood clots, or pulmonary embolism, should avoid HRT.
“Women need to have a detailed discussion with a knowledgeable healthcare provider,” Pinkerton says. “It’s crucial to understand what benefits and risks apply to you personally.”
Whether HRT is right for you is a conversation to have with your healthcare provider. While hormone therapy can ease menopausal symptoms, it carries potential risks. Discussing these benefits and risks with your doctor will help determine if HRT is suitable for your needs.
© 2024 Bennett, Coleman & Company Limited

