- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
NASA Astronaut Sunita Williams’ Health Deteriorates During Extended Mission: Experts Raise Concerns

There is a rising concern about NASA astronaut Sunita William's health after her eight-day mission to the International Space Station (ISS) was extended for six months. The delay was due to a Starliner spacecraft problem that prevented her and fellow astronaut Barry Wilmore from reaching home on time. Doctors are concerned about the effect of her extended vacation on her physical condition, as her return date is set for February.
Weight Loss and Nutritional Deficiencies in Space
Recent photos of Williams reveal significant weight loss. What is most visible are her sunken cheekbones, raising worries about her eating habits. There are speculations of her being on a calorie-deficit diet. This could mean that she ate less than her body required to sustain the high energy needs of space travel.
Astronauts in microgravity must exercise for 2.5 hours daily to maintain muscle and bone health, but the challenging environment can still lead to weight loss, as their bodies expend extra energy adapting to the lack of gravity and maintaining body heat.
Long Wait for Return with the Dragon Capsule
The predicament is exacerbated by a delay in the return car. The crew is now likely to be rescued by Elon Musk's Dragon capsule in February, some months later than anticipated. While experts do not see any immediate risk, they doubt if Williams' current physical state can be sustained for a lengthy term. The lack of fresh food and limited calorie-dense options aboard the ISS may jeopardise her capacity to maintain proper nutrition.
Long Wait for Return with the Dragon Capsule
The predicament is exacerbated by a delay in the return car. The crew is now likely to be rescued by Elon Musk's Dragon capsule in February, some months later than anticipated. While doctors do not believe Williams is in imminent danger, they are unconvinced that his current physical state can be sustained in the long run. The lack of fresh food and limited calorie-dense options on the ISS may jeopardise her capacity to maintain appropriate nutrition.
Health Concerns Highlighted by Crew-8 Hospitalisation
Williams' condition follows another health worry for long-duration astronauts. On November 5, four Crew-8 astronauts—Matthew Dominick, Michael Barratt, Jeanette Epps, and Alexander Grebenkin—were sent for medical review after more than 200 days on the International Space Station. They arrived in Florida on October 25 via the SpaceX Dragon spaceship and appeared to be in good health. However, as a precaution, NASA chose to hospitalize one crew member overnight, while all astronauts received extensive health screenings.
Keep track of the health concerns associated with long-duration spaceflight
NASA suppressed precise details of the Crew-8 medical tests because of privacy concerns, but stated that the procedures were undertaken "out of an abundance of caution." The health concerns connected with long-duration space missions are well established, with difficulties such as muscular atrophy, bone density loss, and potential dietary deficiencies jeopardising astronauts' health upon return. These preventive approaches highlight the importance of ongoing research and careful health monitoring for astronauts on long-term missions.
Ongoing Health Monitoring in space Exploration
As longer missions become the norm, organizations such as NASA prioritise health concerns in order to mitigate the risks associated with prolonged space exposure. Regular exercise, limited meals, and post-mission medical checks are critical for astronauts' health. As space exploration progresses, astronauts' safety on these risky flights becomes more critical for future space missions.
This Common Vaccine Is Linked To Slower Biological Ageing, Researchers Find

Credits: Canva
Scientists have found that a single dose of the shingles vaccine may do more than protect against the painful viral infection. It may also help slow biological ageing in older adults. Researchers from the University of Southern California say the vaccine, commonly given to seniors, could have benefits beyond shingles prevention. The findings come from a study involving over 3,800 people, which showed that vaccinated individuals had fewer signs of biological ageing and lower inflammation levels than those who had not received the shot.
What Is Shingles?
Shingles is a viral condition known for causing a painful, blistering rash. It can appear on different parts of the body but usually shows up as a band of blisters running along one side of the torso. The infection is caused by the varicella-zoster virus, the same virus responsible for chickenpox. Even after recovery from chickenpox, the virus remains dormant in the body and can reactivate years later as shingles, according to the Cleveland Clinic.
While shingles is not usually life-threatening, it can be extremely uncomfortable. Vaccination significantly reduces the risk of developing shingles. Starting treatment early can shorten the duration of the illness and lower the risk of complications. One of the most common complications is postherpetic neuralgia, a condition where nerve pain continues long after the rash has healed.
Shingles Vaccine May Slow Biological Aging In Older Adults
A recent study by the University of Southern California suggests that the shingles vaccine recommended for older adults may help slow down ageing at a biological level, in addition to preventing infection. “While more research is needed to confirm and expand on these results … our findings add to growing evidence that vaccines may support healthy ageing, not just prevent short-term illness,” said Eileen Crimmins, a co-author of the study, in a statement. To explore this further, Crimmins and her team focused on people who had received the shingles vaccine.
Shingles Virus Reactivates Later in Life
Although chickenpox is now uncommon in children, with cases dropping by over 97 percent since the vaccine became part of routine childhood immunisation in 1995, more than 95 percent of adults in the US were infected before that change, according to the CDC. At present, around one million Americans develop shingles every year.
Health authorities recommend that adults aged 50 and above receive two doses of the shingles vaccine. This not only lowers the risk of infection but also reduces the chances of postherpetic neuralgia, a lingering nerve pain that can persist for months or even years after the rash disappears.
Why Biological Age Matters More Than Your Actual Age
The researchers analysed data from more than 3,800 adults aged 70 and older, using information from the nationally representative US Health and Retirement Study. Blood samples were examined to assess seven different indicators of biological ageing.
Unlike chronological age, which simply counts years lived, biological ageing reflects how well the body’s organs and systems are functioning over time.
Shingles Vaccine: Lower Inflammation, Healthier Ageing
Results showed that vaccinated participants had noticeably lower levels of inflammation, a key factor linked to age-related conditions such as heart disease, frailty, and cognitive decline.
“By reducing this ongoing inflammation, possibly by stopping reactivation of the shingles virus, the vaccine may help support healthier ageing,” explained Jung Ki Kim, the study’s lead author.
“Although the exact biological processes are still unclear, the vaccine’s ability to lower inflammation makes it a promising tool in broader efforts to slow age-related decline and improve resilience,” she added.
Shingles Vaccine: What The Blood Markers Reveal About Ageing
The study also found that vaccinated individuals experienced slower changes in how genes are switched on and off, and in how genetic instructions are translated into proteins. These processes are known as epigenetic and transcriptomic ageing and are considered important markers of biological ageing.
When all seven ageing measures were combined into a single biological ageing score, those who had received the vaccine showed slower ageing overall compared with people who had not been vaccinated.
An image collage containing three visuals shows a gloved hand drawing blood into a tube, a longevity test kit with a swab and vial placed on an orange surface, and a screenshot of longevity test results displaying a bar chart of 117 biomarkers and a biological age of 29.3 years, which is 13.5 years younger than the actual age.
I gave lots of blood for six longevity tests — here’s how long I can expect to live
Can Vaccines Protect More Than Just Against Infection?
The findings build on earlier research that has linked adult vaccinations, including shingles and flu shots, to a lower risk of dementia and other neurodegenerative conditions such as Parkinson’s disease.
“This research strengthens the idea that vaccines may help promote healthy ageing by influencing biological systems beyond infection control,” said Kim, who is also a research associate professor of gerontology at USC.
Shingles Vaccine: Long-Term Benefits Seen Years After Vaccination
Importantly, the benefits appeared to last. Even participants who had received the shingles vaccine four or more years before their blood samples were taken still showed slower epigenetic, transcriptomic, and overall biological ageing compared to those who had not been vaccinated.
“These results suggest that shingles vaccination affects key processes associated with ageing,” said Crimmins, who is a USC University Professor and AARP Professor of Gerontology.
If future research confirms these findings, it could offer Americans another reason to get vaccinated and help improve vaccination rates, which remain low. Despite a rise during the pandemic period, only 30.1 percent of eligible Americans had received the shingles vaccine as of 2022.
The study highlights the potential for common vaccines to do more than prevent disease. They could play a significant role in promoting resilience, lowering inflammation, and supporting healthier ageing, especially in older adults.
Fingernail Colour Changes Can Reveal Underlying Disease: What Each Shade May Indicate

Credits: AI Generated
Experts have urged people to keep an eye on their fingernails, as unusual changes might point to underlying health problems. According to specialists, certain nail colours could indicate the risk of severe illnesses. While some changes may be harmless, specific colour alterations could require medical attention. The American Academy of Dermatology Association (AAD) has outlined concerning nail symptoms on its website.
The organisation stated: "Have you noticed a change to any of your nails lately? A change in colour, texture, or shape can be harmless, but it can also be a sign of disease. If you notice any of the following changes to a fingernail or toenail, it's time to see a board-certified dermatologist."
Fingernails Colour Change: What Changes Could Signal Serious Health Conditions
Based on this advice, AAD specialists recommend watching for these nail colours:
- White
- Half pink, half white
- Yellow
- Dusky red half-moons
- A dark streak
They explained: "Nail colour changes can sometimes reflect conditions inside the body. Certain shades may serve as warning signs for specific diseases."
White Nails: Could Indicate Liver Problems or Diabetes
The AAD points out that nails turning white may be a sign of liver disease or diabetes. In liver disease, this is particularly likely in people with cirrhosis, the most advanced stage of the condition.
However, nails can naturally become whiter with age. Still, it is recommended to have any noticeable changes checked by a healthcare professional.
Half Pink, Half White Nails: Possible Sign of Kidney Disease
Nails that appear half pink and half white may indicate kidney problems. The AAD describes this pattern as “a white colour on the upper part of one or more nails and a normal to reddish-brown colour below.”
Yellow Nails: Could Signal Lung or Circulatory Issues
Yellowing of the nails may be linked to lung disease and could reflect problems in the circulatory or lymphatic systems.
"When these systems don’t function properly, fluid can accumulate in the soft tissues beneath the skin, causing nails to turn yellow," explains the Cleveland Clinic. That said, yellow nails can also result from fungal infections or smoking.
Dusky Red Half-Moons: Potential Early Sign of Cancer
The AAD warns that a new or changing dark streak under a nail could indicate cancer, particularly melanoma, which is the most dangerous form of skin cancer. The NHS also advises seeing a GP if “you have a dark area under a nail that has not been caused by an injury.”
Dark Patches Under the Nails: When to Seek Immediate Care
Noticing a dark patch beneath your nail may point to skin cancer. Experts recommend visiting a GP as soon as possible if this occurs.
Other Nail Colours To Watch
Additional nail colours that may indicate health issues, according to the AAD, include:
- Blue nails: Could indicate insufficient oxygen in the blood.
- Pale nails: Might point to anaemia.
- Blue half-moons: Could suggest exposure to toxins or poisoning.
Perimenopause Isn’t Just Hot Flashes, Doctors Explain the Lesser-Known Signs

Credits: iStock
Many in their late 30s and early 40s find themselves Googling weird stuff, including 'why am I having a tingling feelin in my arm?' 'why do I feel like something is brushing across my arm?', and more. This is what many call a phantom feeling arm, which means there is nothing actually tickling, but you feel it anyway. Medically, it is known as paresthesia, a tingling feeling or numb sensation, usually what people refer to as the pins and needles sensation. This is caused by temporary pressure on a nerve or any underlying nerve damage issue.
If you look up anything like that, many women claimed, it instantly shows: perimenopause.
Despite an increased awareness around it, perimenopause and menopause still remain a taboo. In a survey, it was found that 54 per cent of women were concerned about the uncertainty they are about to face in their perimenopause and menopause period.
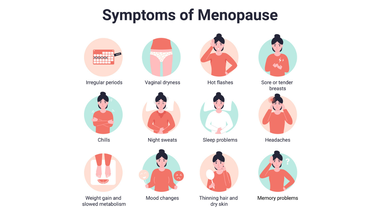
Menopause is not just hot flashes, it is much more than that. Dr Mahima Gulati, an endocrinologist at UConn Health points out symptoms like gaining weight despite "doing everything right", brain fog, aching joints, sleepless nights, exhausting days, and depleted energy. She says "These symptoms are real. This is not something women are imagining, and it is not just aging. There are real biological changes happening, and women deserve evidence based care and support as they move through them."
What Can Help Women Dealing With Menopause and Perimenopause?
Before going into the solution, let us first understand what these term really mean.
Perimenopause: It is the period when a menstruator transitions to menopause, or when the period stops permanently. This phase is characterized by fluctuating hormone levels, irregular periods, which could be shorter, longer, heavier, or lighter, hot flashes, sleep problems and mood changes.
Menopause: This is the natural, permanent end of menstruation defined as 12 consecutive months without a period. This typically occurs between ages 45 to 55.
What Can Help In Menopause And Perimenopause?
Form Connections
“For women to sit in a room and realize they are not alone is incredibly therapeutic. Connection itself reduces the burden of chronic conditions,” points out Dr Gulati.
The doctor points out that women often learn from each others’ experience and this is why social connections are extremely important in this time.
Pay Attention On Sleep
Sleep problems are one of the most common and exhausting symptoms of perimenopause and menopause. Hormonal changes can disrupt deep sleep, causing women to wake up in the early hours, deal with night sweats, and struggle to fall back asleep. When this happens regularly, it leads to severe energy drain, not just tiredness.
To improve sleep, Gulati focuses on simple, practical habits. These include keeping a regular sleep schedule, avoiding caffeine and alcohol in the evening, reducing screen time after 7 p.m., keeping phones out of the bedroom, and practicing calming activities like yoga or meditation. Drinking enough water during the day can also help regulate body temperature at night and reduce hot flashes.
Managing Stress Differently
Instead of trying to eliminate stress, which is often unrealistic, Gulati encourages women to change how they respond to it. Stress is treated as a signal to reassess priorities, set boundaries, and ask for support when needed. This shift helps build resilience and prevents burnout.
Movement Beyond Exercise
Physical activity becomes especially important in midlife, but it’s not just about workouts. Strength training helps protect muscles and bones, while regular movement throughout the day, balance exercises, and flexibility work support long-term health. Reducing long sitting hours is just as important as planned exercise.
Reducing Harmful Habits
Gulati also advises cutting back on alcohol and avoiding tobacco. After menopause, alcohol can worsen sleep, increase belly fat, and raise the risk of conditions like breast cancer and osteoporosis. Limiting late-night screen use can further improve sleep quality.
Eating to Support the Body
Nutrition is another key focus. Rather than aiming for perfection, Gulati encourages small, steady improvements like eating more vegetables and protein, staying hydrated, and choosing foods that may ease menopausal symptoms. The goal is better energy, sleep, and overall health, not just weight loss.
© 2024 Bennett, Coleman & Company Limited

