- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
New Study Reveals Data On Chronic Psychological Distress And Stroke Risk in U.S. Adults

Credits: Canva
Stroke remains one of the leading causes of death and long-term disability in the United States, with substantial health and economic burdens. While traditional risk factors such as hypertension, diabetes, and smoking are well established, emerging research increasingly highlights the critical role of psychological factors, particularly chronic psychological distress, in stroke risk. A recent study published in journal Cureus, titled Chronic Stress and Stroke Among the Adult Population in the United States, sheds new light on this association by analyzing data from a large, representative sample of U.S. adults over more than a decade.
Why Was The Study Conducted?
The study aimed to examine the relationship between chronic psychological distress and stroke incidence among adults in the United States. Utilizing data from the National Health Interview Survey (NHIS), researchers analyzed responses from 284,497 individuals.
Psychological distress was measured using the K6 scale—a brief, standardized, and validated instrument known for its high specificity and reliability (Cronbach’s alpha 0.89)—making it ideal for large population screenings.
What Did The Study Find?
The analysis revealed that individuals experiencing psychological distress had more than twice the odds of having a stroke compared to those without distress, even after adjusting for demographic and cardiovascular risk factors. This 117% increased risk emphasizes psychological distress as a significant, potentially modifiable stroke risk factor.
These findings align closely with prior international studies. Research from Australia and the United Kingdom has similarly demonstrated that elevated psychological distress predicts higher stroke risk. For example, a large UK prospective cohort found significant links between distress and stroke incidence, while Australian studies identified distress as a predictor of fatal ischemic stroke, particularly in men. Another Australian population study confirmed associations between psychological distress and cardiovascular diseases, including stroke and diabetes, measured by similar validated tools.
Further supporting evidence comes from the Multi-Ethnic Study of Atherosclerosis (MESA), a U.S.-based longitudinal cohort, which showed that chronic stress, depression, hostility, and anger were linked to increased stroke or transient ischemic attack risk in adults free of clinical cardiovascular disease at baseline. Although MESA used different stress measures and focused on clinical stroke outcomes, its results complement the current study, underscoring the broader impact of chronic psychological distress on cerebrovascular health.
Role Of Obesity
An intriguing aspect of this study is its exploration of obesity’s interaction with psychological distress and stroke risk. Initially, obesity appeared to increase stroke risk in models unadjusted for cardiovascular factors. However, after adjusting for hypertension, diabetes, coronary heart disease, cholesterol levels, and smoking, obesity was associated with a 14% decreased stroke risk. This phenomenon echoes the “obesity paradox,” where obesity may confer protective effects in certain diseases, including heart failure and chronic kidney disease.
Previous work by the researchers has shown similar paradoxical trends in cardiovascular interventions and bone health, with notable differences across races and sexes. These findings challenge the simplistic view of obesity as universally harmful and support new obesity classifications that differentiate clinical risks. The World Obesity Federation and other scientific bodies have endorsed this nuanced understanding, emphasizing that not all obesity translates into worse health outcomes.
Public Health Implications and Future Directions
The study’s strengths include its large, nationally representative sample and use of the practical, validated K6 scale. The clear link between psychological distress and stroke risk suggests that addressing mental health could be a crucial strategy in stroke prevention efforts.
Given that stroke ranks fourth among causes of death in the U.S., and that stroke morbidity and healthcare costs are rising despite improved therapies, psychological distress stands out as an actionable target. The K6 tool’s ease of implementation in various clinical settings means healthcare providers can efficiently identify at-risk individuals and intervene.
The study highlights the importance of integrating mental health screening and management into cardiovascular risk reduction strategies. Addressing psychological distress offers a promising path to lower stroke incidence and improve overall public health outcomes.
The Age You Get Your First Period At Can Help Identify Long-Term Health Risks

(Credit-Canva)
The first period is a significant moment in the life of a young girl, however, when it happens, the age, plays a much more important role than we realize. National Health Services UK explains that periods can start as early as 8, however the average age is about 12.
A new study showcased in the ENDO Annual Meeting 2025, Endocrine Society from Brazil has found that the age a woman gets her first period, also known as menarche, could provide important clues about her future health. The study shows that both starting your period very early or very late can lead to different health problems later in life.
Different Risks for Different Ages
The age a woman gets her first period (menarche) and the age she reaches menopause mark the beginning and end of her reproductive life. The study looked at data from over 7,600 women in Brazil. It found a link between the timing of menarche and long-term health risks.
Early Menarche
Women who got their first period before age 10 were more likely to have health issues like obesity, diabetes, high blood pressure, and heart problems. They also had a higher risk of reproductive issues like pre-eclampsia.
Late Menarche
Women who started their period after age 15 were less likely to be obese. However, they faced a greater risk of menstrual problems and some specific heart conditions.
What This Means for Women's Health
According to the study's author, Flávia Rezende Tinano, these findings confirm how the timing of puberty can affect a woman's health over many years. She explains that knowing when a woman had her first period can help doctors identify those who might be at a higher risk for certain diseases. This information can lead to more personalized health screenings and preventative care.
The study is one of the largest of its kind in a developing country. It provides valuable data for populations, like those in Latin America, that have been underrepresented in past research. The researchers believe that these findings highlight the need for early health education for young girls and women.
How Timing Reveals Health Risks For Women
A 2013 study published in the Adolescent Health Medicine and Therapeutics journal explained that the timing of these key events can provide important clues about her long-term health. Both very early and very late timing of menarche or menopause have been linked to a higher risk of health problems. Because of this, understanding the connection between these two events could help with preventing chronic diseases. Scientific studies from various fields, including biology, nutrition, and psychology, have looked at the relationship between menarche and menopause.
Early or Late Timing Matters: A woman's age at menarche and menopause is a key sign of her body's aging and how her ovaries are functioning.
Health Connections: Both starting periods very early or very late are linked to different health and social risks later in life.
While many studies have explored the link between menarche and menopause, the results have been mixed. Out of 36 studies reviewed, ten found a direct link, meaning an earlier first period was connected to an earlier menopause. Two studies found the opposite, and the rest found no connection at all. Researchers believe that many things affect the timing of these events, including:
- Hormones and environment
- Socioeconomic status
- Stress throughout life
- Body size and height
Have You Ever Felt Dizzy, Lightheaded When You Stand Up? Here's What It Means

Credits: Canva
Think about that fleeting moment when you get up after sitting or lying down—your head spins, your heart pounds, maybe you feel lightheaded or nauseated. If this scene has become all too familiar, you might be dealing with postural orthostatic tachycardia syndrome—POTS. It’s rare, but for the 1–3 million people in the U.S. who have it, it’s daily life. Now, a heart failure drug is showing real promise in taming the symptoms.
Ivabradine isn’t new—it’s been used for years to manage chronic heart failure, slowing the heart without dropping blood pressure. But a new pilot study, published in the Journal of Cardiovascular Pharmacology, suggests this drug might be a breakthrough for POTS patients. Researchers from UVA Health and Virginia Commonwealth University treated 10 young adults (average age 28, most of them women) with the drug. Normally, when these patients stood, their heart rates surged by around 40 beats per minute. After ivabradine? The spike shrank to only 15 bpm. And symptoms like faintness dropped by nearly 70%, chest pain by 66%—the difference wasn’t just physiological, it was life-changing.
Dr. Antonio Abbate from UVA Health called the findings compelling: cutting heart rate alone—without affecting blood pressure—appeared to break the chain of symptoms. “The inappropriate increase in heart rate is exactly why patients feel sick,” he said.
UVA Health Newsroom
What Is POTS?
Postural orthostatic tachycardia syndrome may sound technical, but its components describe the experience: "postural" (related to posture), "orthostatic" (standing upright), "tachycardia" (a fast heart rate), and "syndrome" (a bundle of symptoms). When someone with POTS stands, their autonomic system fails to constrict blood vessels effectively. The result? Blood tanks into the legs, the heart overcompensates, and you get hit by symptoms: dizziness, pounding heart, fatigue, brain fog, chest discomfort, sweating, nausea—anything but ordinary.
This isn’t a heart-muscle issue or a brain problem: it’s more like a software glitch in how your body regulates itself. It often affects young women between 15 and 50 and can stem from triggers like infections, trauma, pregnancy, or autoimmune diseases.
The recent UVA pilot study isn’t standalone. Earlier research supports the same direction. A 2017 retrospective study of 49 patients—almost all women—found 88% saw palpitations improve and 76% felt less lightheaded, with heart rates dipping and no significant change in blood pressure.
Then a 2021 randomized, placebo-controlled crossover trial—including 22 adults with hyperadrenergic POTS—took it further. The results showed substantial heart rate drops, improved physical and social quality of life, and even reduced norepinephrine levels (the stress hormone that tends to over-react upon standing). None of the participants developed dangerously low blood pressure.
And even earlier studies, including student-case reports and case series, all support the conclusion: ivabradine reduces heart rate without bringing blood pressure down—and that matters because traditional beta blockers can drop both, making some patients feel worse.
How Ivabradine Interrupts the Vicious Vagus Loop?
Here’s what researchers suspect is happening behind the scenes: when someone with POTS stands, the body overreacts with a surge of norepinephrine—our classic fight-or-flight hormone. The heart races, the brain kicks into panic mode, symptoms amplify, and the loop perpetuates itself. Ivabradine, by slowing the heart without altering blood pressure, effectively breaks that cycle at the source. Patients stop spinning, both literally and metaphorically.
What You Should Know POTS?
It's worth noting that these are still early results. The studies are relatively small, but statistically compelling. There's enough here, though, to encourage more formal trials—and for doctors and patients to take notice.
If POTS symptoms sound familiar—if you get faint when you stand, your heart races, and doctors struggle to pinpoint the cause—ivabradine may be a conversation worth having. It’s not a universal cure, but it’s different from other treatments. Rather than forcing blood vessels to tighten or increasing blood volume, it focuses squarely on the heart rate itself.
POTS has always been a misunderstood syndrome—a tricky physiological dance that leaves patients frustrated and clinicians unsure. But treating the pulse directly, instead of chasing blood pressure or fluid levels, looks like a game changer. Ivabradine isn’t a cure-all, but it's poised to offer relief where little existed before.
For anyone sick of dizzy spells, pounding hearts, or unexplained fatigue whenever they stand, it’s time to explore if this one medication could be the difference between feeling trapped and regaining control.
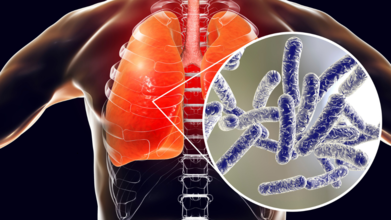
Unique COVID-19 Like Symptoms Of Legionnaires' Disease And How Long Does The Infection Last
Credits: Canva
Legionnaires’ disease, has so far killed 3, and infected around 60 people after the recent outbreak in Central Harlem in the New York City. It is a severe form of pneumonia caused by Legionella pneumophila, and is far more than just a respiratory infection.
Unlike typical bacterial pneumonias, Legionnaires’ disease is increasingly being recognized for its distinct symptoms, both during the acute illness and long after recovery.
Now, a landmark study from Switzerland aims to uncover whether Legionella infections lead to their own version of a “long COVID”-like syndrome, providing crucial insights into the post-acute impact of this underdiagnosed illness.
What Makes Legionnaires’ Disease Different?
Named after a deadly outbreak during an American Legion convention in Philadelphia in 1976, Legionnaires’ disease is spread primarily through contaminated aerosolized water, not person-to-person contact.
The bacteria thrive in warm, stagnant water found in air-conditioning cooling towers, plumbing systems in large buildings, hot tubs, fountains, and even ice machines.
While the respiratory symptoms may initially resemble other types of pneumonia, cough, fever, and shortness of breath, what sets Legionnaires’ disease apart is the constellation of extrapulmonary symptoms that often accompany it.
These include:
- Muscle aches
- Confusion
- Gastrointestinal issues like diarrhea
- Kidney dysfunction
Hyponatremia, or low sodium levels in the blood, a critical and unique marker of this infection
Hyponatremia: A Clue to Legionella
Hyponatremia, one of the hallmark signs of Legionnaires’ disease, is often absent in other pneumonias. This is one of the unique symptoms of Legionnaires' that distinguishes from pneumonia. It results in dangerously low sodium levels, which can trigger symptoms ranging from mild fatigue and nausea to severe complications like confusion, seizures, or coma.
According to the National Institutes of Health (NIH), hyponatremia often appears early in the course of a Legionella infection and should alert clinicians to consider Legionella pneumonia in patients with respiratory symptoms and abnormal lab findings. Its presence can help guide early diagnosis and prompt treatment, which is critical given the disease’s potential severity.
Long-Term Effects: Is There a “Long Legionnaires’”?
Much like long COVID, survivors of Legionnaires’ disease are now reporting symptoms that persist long after the acute infection has cleared.
These post-acute effects, also seen in other forms of pneumonia, include:
- Chronic fatigue
- Brain fog or cognitive dysfunction
- Decreased quality of life
- Ongoing respiratory issues
- Muscle weakness and joint pain
But what if Legionnaires’ disease leaves a unique post-infection footprint?
That’s the central question behind a new prospective cohort study conducted by researchers in Switzerland. Published in Swiss Medical Weekly, the LongLEGIO study is the first of its kind to compare the long-term effects of Legionnaires’ disease to other forms of bacterial community-acquired pneumonia (CAP).
Inside the LongLEGIO Swiss Study
From June 2023 to June 2024, researchers recruited 59 patients with confirmed Legionnaires’ disease and 60 matched patients with Legionella test-negative CAP. Participants were closely matched by age, sex, hospital type, and timing of diagnosis.
Patients were assessed at four key time points:
- During the acute phase (baseline)
- 2 months after treatment
- 6 months after treatment
- 12 months after treatment
The study used patient-reported outcome measures (PROMs), structured questionnaires to capture symptoms often missed in traditional hospital data. These included:
- Health-Related Quality of Life (HRQoL)
- Persistent fatigue
- Need for continued healthcare
- New or lingering symptoms
What the Baseline Data Reveals
Initial findings already highlight striking differences between the two groups. While the median age for both was 69, patients with Legionnaires’ disease were more likely to experience extrapulmonary symptoms. Notably:
- Muscle aches were reported by 51.8% of Legionnaires’ patients, compared to 25.9% of CAP patients.
- Fever was reported in 89.3% of Legionnaires’ cases vs. 76.3% in CAP.
- ICU admissions were higher among Legionnaires’ cases (13.6% vs. 8.3%).
Additionally, Legionnaires’ patients had a higher prevalence of chronic kidney failure (15.3% vs. 10%) and better pre-illness quality of life than their CAP counterparts, who tended to have more comorbidities such as COPD, cancer, and immunosuppression.
These early differences are critical because they suggest that Legionella may cause a distinct form of post-acute infection syndrome, akin to long COVID but possibly rooted in a different biological mechanism.
When Do Symptoms Begin, And How Long Do They Last?
Legionnaires’ disease symptoms typically begin 2 to 10 days after exposure, but the timeline varies based on individual health and level of exposure. Initially, it may mimic the flu:
- Headache
- Chills
- Muscle pain
- High fever (often >104°F)
- Fatigue
As the disease progresses, more severe or unique symptoms may surface, such as:
- Cough (often dry at first)
- Gastrointestinal issues like diarrhea or nausea
- Confusion or disorientation
- Signs of hyponatremia like fatigue, poor concentration, or seizures
For most patients, acute symptoms resolve within 2 to 4 weeks, but that’s not the end of the story.
Based on evidence from pneumonia survivors and early data from the LongLEGIO cohort, recovery can take several months, especially for those who had severe illness requiring ICU care. Lingering fatigue, shortness of breath, cognitive issues, and poor stamina can persist for 6 to 12 months or more.
Some patients, even after a year, may still experience reduced quality of life and ongoing healthcare needs, a pattern increasingly recognized across other infectious diseases but still under-researched in Legionnaires’.
© 2024 Bennett, Coleman & Company Limited

