- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Ozempic Users Found To Age Back By More Than 3 Years, Finds New Trial; Peer Review Pending

(Credit-Canva)
Scientists have found new evidence suggesting that drugs like Ozempic might have an unexpected benefit: they could help reverse aging. Ozempic has gained a lot of popularity recently. Many celebrities have opened up about using it like Oprah, Meghan Trainor, Elon Musk etc. As more people are using it throughout the world, researchers are studying different effects of it. As the drug is still relatively new, we have heard of Ozempic feet, face, smell etc., researchers have found many different effects these weight loss drugs can have on the human body, however this is a new effect that could change the way we view the phrase 'anti-aging'.
A recent study found that the drug semaglutide, which is in Ozempic and Wegovy, made a person's body biologically younger by an average of about three years.
Also Read: Is Yerba Mate Nature's Answer To Ozempic? Risks And Benefits
This research is still new and hasn't been fully reviewed by other scientists, but it points to a future where these drugs could do more than just treat diabetes and help with weight loss.
What Is Biological Age?
To understand the study, you need to know the difference between your chronological age (how many years you've been alive) and your biological age (how old your body is on the inside). Scientists can measure your biological age by looking at certain chemical changes in your DNA.
For this study, researchers at the TruDiagnostic aging lab in Kentucky measured the biological age of 184 people with a condition linked to rapid aging. They gave a weekly shot of semaglutide to a group of people with a health condition that causes them to age faster. A second group received a placebo shot.
Also Read: Why Ozempic Might Be Making Your Favorite Foods Taste Gross?
How Many Years Does Ozempic Age Us Back?
After 32 weeks, the results were significant:
- The group that took semaglutide saw their biological age go down by an average of 3.1 years.
- The drug also seemed to slow down the aging process in important organs like the brain, heart, and kidneys. In some people, their brain's biological age even appeared to be five years younger.
The study suggests that the drug's ability to improve a person's metabolism and fat distribution might be the reason for these anti-aging effects. While it's too early to use these drugs specifically for anti-aging, these findings are an important first step.
While the study was done on people with a specific health condition, the lead researcher believes the benefits could apply to a wider population. Although it's too early to start using these drugs just for anti-aging, the findings are exciting and point to a potential future where drugs like Ozempic could do more than just treat diabetes and obesity.
This research provides the first real evidence from a clinical trial that semaglutide can actually change the biological signs of aging. It suggests that drugs like Ozempic could be used in the future not just for weight loss and diabetes, but also to help people live longer, healthier lives.
More research is needed, but these findings are a big step forward in understanding the full potential of these drugs. As this research moves forward to be peer-reviewed, one must know what the side-effects of the medicine are.
Side-Effects of Ozempic
Diabetes UK explains that all medications, Ozempic can cause side effects. The most common ones include:
- Nausea
- Diarrhea
- Vomiting
- Risk of worsening eye disease
- Risk of low blood sugar (hypoglycemia)
- Risk of high blood sugar (hyperglycemia)
Not everyone who takes Ozempic will experience these side effects. The likelihood of having them can vary, so it's important to discuss the potential risks with your healthcare provider.
Risks of Ozempic to Watch For
There are a few more serious side effects to be aware of, especially if you have other health conditions:
Risk of Worsening Diabetic Eye Disease (Retinopathy)
If you have diabetic eye disease and also use insulin, there is a risk that your condition could get worse when you start taking Ozempic. This is thought to be caused by a rapid drop in blood sugar. It's crucial to tell your doctor if you have this eye condition or if you notice any changes in your vision after starting Ozempic.
Risk of Low Blood Sugar
When taken alone, Ozempic doesn't usually cause low blood sugar. However, the risk increases if you take it along with other diabetes medications, such as insulin or a sulphonylurea. Your doctor may need to adjust the dose of these other medications to help prevent this from happening.
Also Read: Ozempic Came From A Monster’s Venom-The Creature That Made Weight Loss A Trend
Risk of High Blood Sugar
If you take Ozempic with insulin and your insulin dose is reduced too quickly, it can cause high blood sugar levels. This can lead to a serious condition called diabetic ketoacidosis (DKA). Your healthcare team should explain the signs and symptoms of DKA to you.
Do You Wear Contact Lenses? This Rare Eye Parasite Can Permanently Damage Your Vision

Credits: Canva
Nearly four years ago, Teresa Sanchez was in Mexico for a medical procedure when her right eye began to feel unusually dry and irritated. At first, it seemed minor. She assumed her contact lens might be torn or that the switch from daily lenses to monthly ones was causing dryness. She even wondered if her body was fighting off an infection, as per CNN.
What she did not realize at the time was that a microscopic organism was slowly attacking her cornea. Over the next three months, the parasite caused irreversible damage to her vision and triggered searing pain that spread across her head.
“I couldn’t even keep the blinds open in my room,” said Sanchez, now 33 and living in Las Vegas. “Light would cause unbearable pain. That’s when I knew something was seriously wrong.”
By then, she had already seen multiple optometrists and had been misdiagnosed. Frustrated and desperate for answers, Sanchez began researching her symptoms on her own.
What Is Acanthamoeba Keratitis?
Online searches led Sanchez to a condition she had never heard of: acanthamoeba keratitis. An eye specialist later confirmed it. Keratitis refers to inflammation of the cornea, the clear, dome-shaped layer at the front of the eye that plays a central role in focusing vision. Acanthamoeba is a microscopic, single-celled organism that cannot be seen without a microscope.
According to Dr. Jacob Lorenzo-Morales, a professor of parasitology at the University of La Laguna in Spain, acanthamoeba is commonly found in soil and water. It does not require a host to survive, which makes it especially resilient.
Once the organism comes into contact with the eye, it can attach itself to the cornea. Dr. Paul Barney, an optometric physician and director at the Pacific Cataract and Laser Institute in Alaska, explained that even tiny breaks in the corneal surface can allow the parasite to burrow deeper into the eye.
Why Contact Lens Wearers Face Higher Risk?
Acanthamoeba keratitis is considered rare. Based on data from 20 countries, including the UK, India, the US, Canada and Brazil, there are more than 23,000 cases worldwide each year. Yet a striking pattern stands out. Between 85% and 95% of people who develop the infection wear contact lenses.
Contact lenses can cause microscopic abrasions on the cornea, creating an entry point for the parasite. The organism can also cling to the lens itself or become trapped between the lens and the eye, making it easier to penetrate the corneal tissue.
“If it’s not diagnosed early and treated aggressively, the outcome can be devastating,” Barney said. “The parasite feeds on the cornea, triggering inflammation and tissue damage that can lead to permanent vision loss.”
In some cases, vision can be partially restored with treatment. Others require a corneal transplant.
A Parasite Built To Survive
Treating acanthamoeba keratitis is especially difficult because the organism has strong defense mechanisms. It can sense threats and respond by forming a cyst, allowing it to lie dormant for months or even years.
This resilience means treatment often stretches over long periods and involves intense discomfort. Because the eye is extremely sensitive, patients must work closely with specialists and strictly follow treatment instructions.
Why The Condition Is Often Missed?
Early diagnosis is one of the biggest challenges Because acanthamoeba keratitis is uncommon, many optometrists may not recognize it right away. As a result, many contact lens users only learn about the condition after they develop it or come across viral videos discussing it online.
Many patients have expressed surprise that they were never clearly warned about the risks of wearing contacts while showering or swimming.
The Contact Lens Society of America emphasized that contact lenses are medical devices and require strict hygiene. This includes avoiding water exposure during swimming, showering or sleeping. The organization also stressed the importance of patients asking questions and carefully reviewing care instructions.
Acanthamoeba Keratitis: Symptoms That Mimic Other Eye Infections
In addition to severe pain and light sensitivity, acanthamoeba keratitis can cause redness, blurred vision, dryness, excessive tearing and the sensation that something is stuck in the eye.
Because these symptoms overlap with other conditions, misdiagnosis is common. Barney said the infection is frequently mistaken for herpes simplex keratitis, a major cause of infection-related blindness. In its earliest stages, it can even resemble pink eye.
That was the case for Sanchez. Her first optometrist diagnosed pink eye. The prescribed drops blurred her vision. A second optometrist suspected a bacterial infection, and while antibiotic drops offered brief relief, she soon lost vision in the affected eye.
Acanthamoeba Keratitis: How To Reduce Your Risk?
Experts stress that contact lens hygiene is critical. Always clean and store lenses using approved contact lens solution, never water. The solution in your lens case should be replaced daily. Wash and dry your hands thoroughly before handling lenses.
Sleeping in contact lenses should be avoided, as it increases dryness, irritation and the risk of corneal damage. Daily disposable lenses may lower infection risk compared to monthly lenses.
For water-based activities, glasses or prescription goggles are safer options. Some people may also consider vision correction surgery after discussing risks and suitability with a doctor.
Taking NSAIDs For Osteoarthritis? NHS Shares An Important Warning

Credits: Canva
More than 10 million adults, young people, and children in the UK are currently living with arthritis, according to a 2025 report by Arthritis UK. The NHS says osteoarthritis is the most common form of the condition across the country.
NHS Issues Warning For People Taking NSAIDs For Osteoarthritis
Osteoarthritis develops when joints become stiff and painful over time. Symptoms vary widely depending on the joint involved and the severity of damage. While medication is often used to manage pain and inflammation, the NHS warns that some commonly used treatments can carry risks if not taken correctly.
One of the most widely used options for pain relief is NSAIDs, a group of medicines many people rely on daily.
What Are NSAIDs And Why Are They Prescribed?
NSAIDs, or non-steroidal anti-inflammatory drugs, are commonly prescribed by GPs to relieve pain, swelling, and inflammation. They are available in several forms, including tablets, capsules, suppositories, creams, gels, and injections. Some NSAIDs can be bought over the counter, while stronger versions require a prescription.
Common types of NSAIDs
The most commonly used NSAIDs include:
- ibuprofen
- naproxen
- diclofenac
- celecoxib
- mefenamic acid
- etoricoxib
- indomethacin
- aspirin for pain relief (low-dose aspirin is not usually classed as an NSAID)
Doctors usually advise which NSAID is suitable and explain the potential benefits and risks. However, the NHS stresses that patients should also understand possible side effects and when to seek medical help.
NHS Warning On Who Should Be Cautious With NSAIDs
The NHS advises that NSAIDs may not be suitable for everyone. Extra caution is needed if you have asthma, stomach ulcers, angina, or if you have previously had a heart attack or stroke. People taking low-dose aspirin should always speak to their GP before using an NSAID.
Who Should Avoid Or Seek Advice Before Taking NSAIDs?
You should consult a pharmacist or doctor before using NSAIDs if you:
- are over the age of 65
- are pregnant or trying to conceive
- are breastfeeding
- have asthma
- have had an allergic reaction to NSAIDs in the past
- have a history of stomach ulcers
- have heart, liver, kidney, blood pressure, circulation, or bowel problems
- are taking other medicines
- are buying medicine for a child under 16 (aspirin should never be given to children under 16)
The NHS explains that NSAIDs are not always completely avoided in these cases, but they should only be used with medical advice, as the risk of side effects may be higher.
If NSAIDs are unsuitable, doctors or pharmacists may recommend alternatives such as paracetamol.
Possible Side Effects Of NSAIDs
Over-the-counter NSAIDs generally cause fewer side effects than prescription-strength versions. However, risks increase when they are taken at high doses, used for long periods, or taken by older adults or people with underlying health conditions.
Possible side effects include:
- indigestion, stomach pain, nausea, and diarrhoea
- stomach ulcers, which can lead to internal bleeding and anaemia
- headaches
- drowsiness
- dizziness
- allergic reactions
In rare cases, NSAIDs can affect the liver, kidneys, heart, or circulation, and may increase the risk of heart failure, heart attacks, or strokes.
Taking NSAIDs Alongside Other Medicines
It is essential to seek medical advice before taking NSAIDs if you are already using:
- another NSAID
- low-dose aspirin or warfarin
- ciclosporin
- diuretics for high blood pressure
- lithium
- methotrexate
- selective serotonin reuptake inhibitors (SSRIs) such as citalopram or fluoxetine
Signs And Symptoms Of Osteoarthritis
Common symptoms of osteoarthritis include joint pain, stiffness, and difficulty moving the affected joints. Some people may also experience:
- swelling
- joint tenderness
- a grating or crackling sensation when moving joints
- pain and stiffness after periods of inactivity
- enlarged or knobbly joints
- reduced range of movement
- muscle weakness or muscle loss
The NHS notes that osteoarthritis can affect almost any joint but most commonly involves the knees, hips, and small joints of the hands. Anyone with persistent symptoms should see their GP for diagnosis and treatment advice.
Even people who do not fall into higher-risk groups should only use NSAIDs as directed by a healthcare professional. Side effects can still occur, especially with long-term use. If NSAIDs are not appropriate, safer alternatives may be suggested to manage pain effectively.
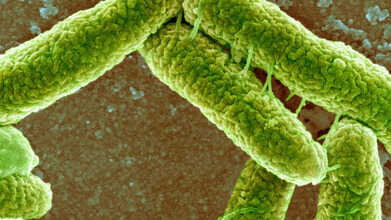
E. Coli Detected In Bhopal Groundwater: Symptoms To Watch And How To Stay Safe
Credits: Canva
Following the water contamination emergency in Indore, similar concerns have now surfaced in Madhya Pradesh’s capital. Groundwater samples collected from four locations in Bhopal have tested positive for E. coli bacteria. In response, the Bhopal Municipal Corporation has barred residents from using groundwater for any purpose.
Officials clarified that the contamination is restricted to underground water sources and has not spread to the treated piped water supplied across the city. According to ANI, civic teams have tested 1,810 water samples so far and inspections are still underway in all zones.
E. coli was the same bacteria responsible for Indore’s recent water crisis, which claimed 20 lives, including that of a five-month-old infant. As per a report by Dainik Bhaskar, fear has gripped several neighbourhoods in Bhopal, with residents hesitant even to touch the water. Locals say the water is unfit not only for drinking but also for washing hands, utensils, or bathing. In some areas, tap water reportedly turns reddish within minutes and emits a strong, foul smell. Adding to the concern, iron levels in the water are said to be nearly 100 times above permissible limits.
Here is what you need to know about E. coli, how it spreads, its symptoms, and ways to stay safe.
What Is E. Coli Bacteria?
Escherichia coli, commonly known as E. coli, refers to a group of bacteria that naturally live in the intestines of humans and animals. Most of these strains are harmless and even play a role in digestion. However, certain types can trigger illness when they enter parts of the body where they do not belong or release harmful toxins.
These disease-causing strains attach themselves to body cells and produce toxins, leading to infection and inflammation.
What Happens During An E. coli Infection?
An E. coli infection occurs when harmful strains of the bacteria enter the body. It most often affects the digestive system, causing symptoms such as watery diarrhoea, abdominal pain, and gastroenteritis. In some cases, the bacteria can also infect the urinary tract.
Certain strains produce Shiga toxin, which can lead to severe complications, including kidney damage, especially in children and older adults.
Why E. coli Infections Occur?
E. coli has many strains. While some support gut health, others can cause serious illness. Experts classify the harmful types based on how they attach to cells and the toxins they release. Several strains are known to cause diarrhoeal diseases, including:
- Shiga toxin-producing E. coli (STEC)
- Enterotoxigenic E. coli (ETEC)
- Enteropathogenic E. coli (EPEC)
- Enteroaggregative E. coli (EAEC)
- Enteroinvasive E. coli (EIEC)
- Diffusely adherent E. coli (DAEC)
Other important strains include uropathogenic E. coli, which is a common cause of urinary tract infections, and E. coli K1, which can lead to meningitis in newborns, according to the Cleveland Clinic.
Common Signs Of E. coli Infection
An infection affecting the gut often begins with digestive symptoms. These may include:
- Diarrhoea that is watery and sometimes blood-stained
- Abdominal pain and cramping
- Reduced appetite
- Mild fever
The Cleveland Clinic notes that watery diarrhoea is usually the earliest symptom when the gastrointestinal tract is involved. Symptoms can vary depending on which part of the body is infected.
How To Protect Yourself From E. Coli?
Preventing E. coli infection largely depends on basic hygiene and safe food practices. Since the bacteria spreads through contaminated food, water, and faecal matter, simple precautions can lower the risk significantly.
Maintain hand hygiene
Wash hands thoroughly with soap and water for at least 20 seconds before eating or cooking, after using the toilet, changing diapers, or handling animals. Proper handwashing removes bacteria and limits its spread.
Practice safe food handling
Use separate cutting boards and utensils for raw meat and ready-to-eat foods. Clean kitchen surfaces and tools with hot, soapy water after each use. Keep raw meat away from fruits and vegetables to avoid cross-contamination.
Cook food completely
Ground meat should be cooked to at least 160°F or 71°C, while poultry needs to reach 165°F or 74°C. Using a food thermometer ensures food is properly cooked and free from harmful bacteria.
Clean fruits and vegetables
Wash all produce under running water just before consumption, even if you plan to peel it. This helps remove bacteria picked up from soil or contaminated irrigation water.
Choose safe drinks
Consume only pasteurised milk and juices, and rely on boiled or treated municipal water. Avoid unpasteurised products and untreated water, as pasteurisation effectively eliminates dangerous E. coli strains.
© 2024 Bennett, Coleman & Company Limited

