- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
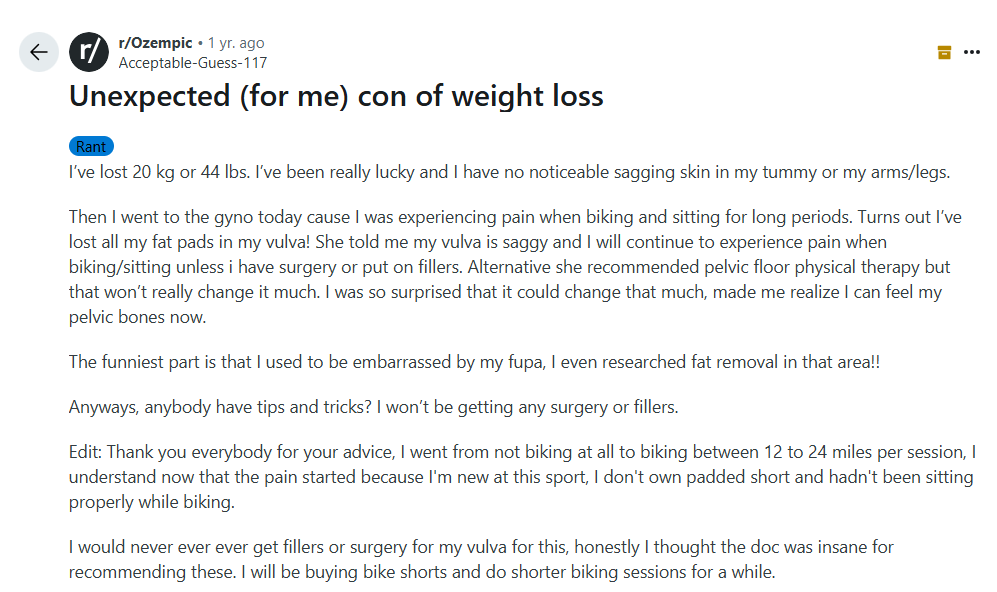
‘Ozempic Vulva’: The Bizarre Side Effect Affecting Women’s Health

Credits: Canva
GLP-1 medications, including the popular brand Ozempic, have made headlines for their dramatic weight loss results. Initially created to treat type 2 diabetes, the medications were a favorite among those wanting to lose weight due to their ability to control hunger. Semaglutide, the active drug found in Ozempic, makes consumers full for extended periods, resulting in significant weight loss in the body. However, with increasing popularity comes an uptick in reports of unusual side effects—some of which are leaving women shocked and bewildered.
Among the most surprising and strange side effects making the rounds among users is what has been colloquially referred to as "Ozempic vulva." The condition involves a reduction of fat in the labia majora, a sagging appearance, pain during routine activities, and alteration of sexual anatomy aesthetics. Although sagging skin and loss of elasticity have long been linked to weight loss, particularly if it occurs rapidly, this particular side effect has only recently emerged.
A Reddit poster posted a first-hand account of experiencing the results for herself. Losing 44 pounds, she at first was jubilant about the outcome. "I've been extremely fortunate and I don't have any sagging skin in my belly or arms/legs that I can notice," she described. But the biggest shock was when she went for a gynecologist appointment. "Turns out I've lost all my fat pads in my vulva! She informed me my vulva is droopy and I will keep on having pain when cycling/sitting unless I undergo surgery or wear fillers," the user posted.
The Redditor also revealed that pelvic floor physical therapy was provided as a substitute for cosmetic intervention, although it would not fully reverse the deflation. Her case highlights the need to be aware of how sudden weight loss, especially from medications such as GLP-1s, can impact lesser-known parts of the body.
Medically, the vulva comprises external female genitalia, mostly the labia minora and labia majora, that act as cushioning protection. Fat loss in this region may cause a greater prominence of the pelvic bones, decrease in cushioning, and pain during exercises like cycling, running, or sitting for extended periods.
What is 'Ozempic Vulva'?
The vulva is the external female genitalia, especially the labia majora covering the inner structures. Redditors and users of internet forums have described decreased fat pads in this region after precipitous weight loss caused by GLP-1 medication. One Redditor summed up her experience thus: after losing 20 kg (44 pounds), she developed pain when she cycled or sat for long hours. A gynecologist described losing much of the natural padding around her vulva, leading to a sagging sensation and discomfort during exercise.
Also Read: Ozempic Vulva To Ozempic Smell – Unexpected Ways Of Weight Loss Jabs Change Your Body
This trend, affectionately but aptly called "Ozempop vulva," highlights a singular and seldom-talked-about side effect of weight loss caused by medications. For most women, it's not just aesthetic; it impacts daily comfort, sex, and self-esteem.
Cosmetic treatments have evolved as a result of this trend. "Labia puffing" is an increasingly sought-after procedure for women who experience vulvar deflation. This treatment either involves the use of dermal fillers or fat transfer to add volume to the labia majora, evening out the texture and alleviating discomfort. Though effective, it is quite expensive, between $2,600 and $6,500 in America.
Healthcare professionals are urging caution. Novo Nordisk, the drug maker of Ozempic, reassured the public that patient safety is of utmost priority and assured that the medicines are to be used only for approved use in a medical setting. They also urge reporting side effects to healthcare professionals or regulatory bodies. "Treatment decisions should be made together with a healthcare provider who can evaluate the appropriateness of using a GLP-1 based on assessment of a patient's individual medical profile," said the company.
The larger context of extreme weight loss makes visible the far-reaching consequences GLP-1 drugs can have. Patients experience a range of side effects, from gastrointestinal distress to loose skin, facial fat redistribution, and effects on sexual anatomy and desire. While the physical changes are something to be admired, these effects are a reminder that extreme weight loss is not risk-free.
Incidentally, online discussions of "Ozempic vulva" have become widespread in private online forums and social media sites. Users freely exchange experiences, coping mechanisms, and aesthetic issues. Many recommend practical measures like padded bike shorts or briefer periods of exercise to alleviate discomfort. Others discuss surgical or nonsurgical treatments, although opinions are highly diverse on whether such a procedure would be desirable or required.
Medical professionals emphasize the need for integrated treatment. Sudden loss of weight must be watched over by medical professionals who can advise on likely risks to both general health and particular aspects such as the vulva. Preservation of muscle tone, padding, and elasticity of skin is essential to avoid long-term complications. For women suffering from discomfort, focused physical therapy, proper protective equipment during exercise, and well-informed consideration of cosmetic interventions may all be part of a successful management plan.
Finally, "Ozempic vulva" highlights an increasing trend on the intersection of weight-loss medication and women's health. While the drug has transformed weight control for millions of people, its unintended side effects serve as a reminder that there are risks associated with every medical intervention and that they need to be closely monitored. Education, research, and transparency with healthcare professionals are critical towards preventing such unintended outcomes.
As GLP-1 drugs become more mainstream, patients and providers alike need to be watchful. New side effects such as "Ozempic vulva" demonstrate the importance of full education on the entire range of possible changes wrought by sudden weight loss. Meanwhile, women dealing with these effects are complying with both medical advice and home remedies, being resilient in the face of an odd but increasingly prevalent health issue.
Why Multiple Sclerosis Increases Emotional Burden Among Women

Credit: iStock
Beyond being a medical challenge, multiple sclerosis (MS), which affects nearly three times as many women as men, raises emotional and physical concerns among women.
MS is a neurological condition that affects cognitive, emotional, motor, sensory, or visual functions. It is also a chronic autoimmune disease that is caused when a person’s immune system attacks their brain and spinal cord.
According to the UK-based MS International Federation, an estimated 2.8 million people live with MS worldwide, with prevalence increasing globally. However, women make up about 75 percent of MS patients globally.
However, women are disproportionately affected. The diagnosis gets more emotionally challenging for women as it often appears during early adulthood -- a key period for women building their careers, relationships, and families.
Estrogen, genetics and a lack of Vitamin D are major reasons for its increased prevalence in women.
Beyond the clinical symptoms, the anxiety, depression, mood changes, and stress, driven by uncertainty about disease progression, impact the daily life of women. Concerns about pregnancy, parenting, work, and long-term independence can further intensify the emotional burden.
“MS is significantly more prevalent in women, often striking during their most pivotal years. For many women, the diagnosis goes beyond a medical challenge; it becomes a profound emotional crossroads centered around family planning. They face daunting questions: Can I safely carry a pregnancy? Is breastfeeding possible? Will I have the physical stamina to care for a child? These are not merely clinical concerns; they are deeply personal anxieties about identity, motherhood, and the future,” Dr. Sudhir Kumar, Sr. Consultant Neurologist, Apollo Hospital, Jubilee Hills, Hyderabad, told HealthandMe.
“Multiple sclerosis is increasingly recognized as a disproportionate neurological burden among women. Globally, women are affected nearly two to three times more often than men, a pattern believed to arise from a complex interaction of immune system behavior, hormonal influences such as estrogen fluctuations, genetic susceptibility, and environmental triggers, including low Vitamin D levels and viral exposures,” added Dr. Manish Gupta, Director – Neurology, Max Super Specialty Hospital, Noida.
Symptoms of multiple sclerosis can be different from person to person. They can come and go or get worse over time. MS can affect any part of the central nervous system.
MS symptoms can worsen with heat or during other infections, such as urinary tract or respiratory infections.
Common symptoms can include:
- vision problems
- difficulty walking or keeping balance
- difficulty thinking clearly
- numbness or weakness, especially in the arms and legs
- muscle stiffness
- depression
- problems with sexual function or urination
- feeling very tired.
“No two patients experience MS in the same way. Symptoms depend on the location of demyelinating lesions in the brain or spinal cord, affecting vision, mobility, cognition, balance, or sensation. This biological variability makes early diagnosis and timely, high-efficacy intervention critical. The goal today is no longer just to manage relapses. It is to limit ongoing subclinical inflammation, prevent silent progression, and delay long-term disability,” Dr. Kumar said.
Why Treating Multiple Sclerosis Is Difficult
MS is an inflammatory condition that results from an autoimmune attack on myelin -- the fatty insulation that surrounds the nerves in the brain and spinal cord.
This disrupts the electrical impulses that are sent through the nerves to the rest of the body and results in scars (plaques or sclerosis).
“Multiple Sclerosis is one of the most complex neurological disorders we encounter in clinical practice, not because it is untreatable, but because it is unpredictable. MS is an immune-mediated disease characterized by inflammation and demyelination — damage to the protective myelin sheath that insulates nerve fibers in the brain and spinal cord. When this insulation is stripped away, nerve signals slow down or become distorted, producing a wide spectrum of symptoms, varying from fatigue, blurred vision, and dizziness to limb weakness, imbalance, or sensory disturbances,” Dr. Subhash Kaul, Consultant Neurologist at KIMS Hospital, Hyderabad, told HealthandMe.
Many of these are invisible, fluctuating, and easily dismissed, both by patients and sometimes even by primary care providers. It is not uncommon for individuals in the early stages of MS to be misdiagnosed.
“This delay in recognising the disease is deeply concerning, because MS strikes people in the prime of their lives — when they are building careers, raising families, and contributing economically. If left untreated, the disease does not remain static; inflammation accumulates silently, relapses leave residual deficits, and disability compounds over time. This is precisely why early and appropriate treatment matters,” said Dr. Kaul.
Yet, experts stated that early diagnosis remains crucial. Regular neurological evaluation for persistent numbness, vision disturbance, or unexplained fatigue allows timely therapy. Disease-modifying treatments, adequate sunlight exposure, physical activity, and stress management help slow progression and preserve long-term neurological function.
“Multiple Sclerosis is not a series of unfortunate episodes; it is a silent, relentless fire. From the moment of onset, MS acts as a chronic, immune-mediated assault on the central nervous system, often causing irreversible damage long before the first visible symptom appears. As one of the leading causes of non-traumatic disability in young adults, we must confront a sobering reality: even when a patient appears clinically stable, “smoldering” inflammation frequently continues beneath the surface, gradually eroding brain volume and neural pathways,” Dr. Kumar said.
“By intervening decisively at the outset, we can suppress smoldering inflammation, preserve long-term neurological function, and give women the confidence to pursue the lives and families they envision,” he added.
Karnataka’s Social Media Ban To Help Children Find Life Beyond Screens

Credit: Canva
Chief Minister Siddaramaiah’s announcement during his presentation of the Karnataka State Budget 2026-27, proposing a ban on social media for children under 16 years of age, has sparked intense interest among parents and professionals alike. As the first state in India to attempt such a sweeping measure, the government has invited us to reflect upon this proposal.
We are in an age where technological advancements have blurred the lines between online and offline worlds, blending them seamlessly. While this is the norm in the world of adults, it has silently reshaped childhood with increased screentime.
Concerns about digital dependency, anxiety disorders in children, and reduced focus in academic and non-academic tasks have already made it to research papers and therapy rooms.
But Karnataka has now shifted the focus from debate to discussion and action. While a ban may reduce certain risks of social media exposure, children’s psychological needs like social connection, belonging, peer group and individual identity, besides guidance, must be nurtured if such protections are to be meaningful.
The Pediatric Perspective: A Medical Minefield
From a psychological perspective, the idea of an age-based social media ban is both promising and complex. On the brighter side, reducing screen usage can help address problems of poor sleep schedules, heightened anxiety, and trouble concentrating in studies or tasks. These problems have become increasingly common among not only adolescents, but very young children too.
However, age alone cannot be used as the single measure of readiness to implement this proposal. Two children of the same age may differ vastly in maturity levels, coping skills, and the ability to use technology responsibly.
The deeper issue is not simply “how much time” children spend online, but “what they do there”. Creative exploration, learning, and connection can be enriching, while endless scrolling reinforces dependency and stress.
A ban can reduce such harmful patterns, but in order to have real impact, such a move should be paired with support for children’s psychological needs to help them combat loneliness, handle peer pressure, and guiding their search for identity. Addressing these issues along with the ban can make the protection well intended, more meaningful and long-lasting.
The Silent Crisis: Nocturnal Anxiety And Doom-scrolling
Late-night scrolling (doom scrolling) is more than just a disruption of sleep. It is a psychological trigger for worry and overthinking. In the quiet of the night, children are left alone with a flood of unfiltered information, which can heighten anxiety, and unwanted exposure to inappropriate content.
An effective way to combat the dangers of unsupervised social media access could be “digital sundowning” i.e. setting clear screen time guidelines for children. Families can create screen-free zones, especially in bedrooms, bathrooms, and at dining tables, or create “phone parking zones” – a specific place in the house to keep all phones so no one is carrying them around all the time. This can encourage children towards healthier routines.
Unlike government-imposed bans, household practices can set healthy and firm boundaries, reinforce self-regulation and reduce the anxiety that comes from constant connectivity and information overload.
Symptoms In The Clinic: Beyond The Screen
In therapy rooms and schools, counsellors are addressing more and more concerns about children and adolescents spending excessive time with their screens. Some of the common ones are highlighted here:
- Social Isolation in Hyper Connectivity: Children may appear socially active online but withdraw from face-to-face interactions, leaving them paradoxically isolated.
- Body Image Concerns: Exposure to curated images on social media can fuel anxiety about appearance among growing children, who are already socially awkward during adolescence. This goes beyond normal teenage insecurity and can spiral into unhealthy self-image or self-criticism.
- Academic Fatigue: Digital content trains the brain to expect constant novelty and quick changes within a short time span of seconds or minutes, which makes textbooks and traditional classroom driven problem-solving feel slow and tiring. This leads to academic fatigue, where children struggle to sustain focus for deeper learning.
- Fear of Missing Out (FOMO): Constant checking of devices reflects a deep-seated need for validation and belonging. FOMO keeps children’s nervous systems on a constant loop of high alert, thus undermining emotional stability.
What Comes Next: The Prioritization Framework
For this ban to have a lasting impact, it needs to draw on psychological principles. Restrictions work best when paired with meaningful alternatives, as children are known to engage positively when they feel supported rather than restricted or scolded. A framework needs to be set up where learning and guidance is prioritized and alternatives offered are strengthened. Some pointers:
Digital Literacy in Schools: Children should be taught not only to limit screen time but also to understand how online platforms work. Lessons on algorithms, advertising, and curated content help them understand and evaluate what they see, so they become more resilient to digital influence.
Parental Guidance Programs: As with other trained behaviors, parents play a central role in shaping healthy digital habits too. Guidance programs can provide resources and strategies for families to showcase balanced device use. When adults demonstrate mindful online usage and behavior, children are likely to follow.
Physical and Social Alternatives: If digital spaces are restricted, offline opportunities must be strengthened. Sports, arts, and community activities help children gain a sense of belonging and enjoyment beyond screens, thus building confidence and social skills in real life.
Collaboration with Tech Companies: Lasting change requires cooperation of technology providers and social media platforms. Stricter age verification systems and design changes at the source are needed, rather than placing usage responsibility on children. By remodeling platforms, risk of unsupervised penetration of digital content can be mitigated so children may still be allowed safe, and age appropriate engagement on social media.
As Karnataka moves into this new territory, one thing is certain – the intention is noble. However, the execution of such a ban will require a fine balance of protection and empowerment, as it attempts to re-imagine childhood experiences in an age where the “virtual” and the “real” are meshed together. Whether this becomes a guiding model for the rest of the country, will depend entirely on how thoughtfully it is carried out.
Karnataka’s proposed ban is a bold first step, but its true impact will depend on how parents, teachers, and policymakers align on this, because healthy childhoods thrive not on restrictions, but through resilience, support, guidance, and strong offline connections that nurture growth and belonging.
Experts Flag Rising Iron Deficiency Among Women; Timely Screening Key

Credit: Canva
Iron deficiency is one of the most common nutritional problems among women, but in the juggle between professional and household responsibilities, a majority of women tend to ignore their health. However, the detecting the mild symptoms in the beginning can help boost treatment and improve quality of life for women, said experts, while stressing the need for timely screening, ahead of International Women's Day.
International Women's Day is observed globally on March 8 every year.
According to health experts, in a month, around 5 out of 10 women between the ages of 30 and 45 visit doctors with complaints such as persistent weakness, headaches, and tiredness. These symptoms are often linked to iron deficiency and put women at risk of developing anemia.
“Iron deficiency is a matter of concern among women, because the symptoms, such as fatigue and weakness, are neglected until the condition becomes serious,” said Dr. Upasana Garg, Regional Technical Chief, Apollo Diagnostic Mumbai.
Dr. Garg said iron deficiency can be detected through simple blood tests that will be advised by the expert and will play a pivotal role in early diagnosis and timely treatment.
These include tests for
- Hemoglobin levels -- are carried out to measure the amount of oxygen-carrying protein in the blood and indicate if a woman has anemia
- Serum ferritin and iron levels -- to gauge the amount of stored iron in the body and help detect iron deficiency even before anemia develops
- A complete blood count (CBC) -- to measure red blood cells, including their size and number, which checks if the body is producing healthy blood cells.
Anemia In Women
Anemia is a major public health concern, mainly affecting young children, pregnant and postpartum women, and menstruating adolescent girls and women.
The World Health Organization (WHO) estimates that 40 percent of all children aged 6–59 months, 37 percent of pregnant women, and 30 percent of women 15–49 years of age worldwide are affected by anemia.
Anemia occurs when there isn’t enough hemoglobin in the body to carry oxygen to the organs and tissues.
In severe cases, anemia can cause poor cognitive and motor development in children. It can also cause problems for pregnant women and their babies. It is often caused by a lack of iron in the blood.
“Iron is a necessary mineral which helps the body to produce hemoglobin, a protein in red blood cells that carries oxygen to different parts of the body. When the body does not have enough iron, it is unable to produce healthy red blood cells. This condition is known as iron deficiency or iron deficiency anemia,” said Dr. Ritu Agrawal, Gynecologist, Zynova Shalby Hospital, Mumbai.
Dr. Agrawal said that women are more likely to experience iron deficiency when compared to men.
The major reason is blood loss during menstruation, and women who have heavy periods are at a higher risk.
During pregnancy, when the body needs extra iron to support the growing baby, the risk of anemia increases in the mother.
Other factors include poor diet, skipping meals, and not eating enough iron-rich foods.
Early Screening And Treatment
The common symptoms of anemia in women include:
constant tiredness,
weakness,
pale skin,
shortness of breath,
dizziness,
headaches,
hair fall
difficulty concentrating
frequent infections due to reduced immunity
Dr. Agrawal said that 50 percent of women tend to ignore early symptoms of anemia.
“In a month, around 5 out of 10 women between the ages of 30–45 visit with complaints such as persistent weakness, headaches, and tiredness, which are often linked to iron deficiency and put them at risk of developing anemia. If iron deficiency is not treated in time, it can lead to several health complications,” she added.
Severe anemia can also lead to heart-related problems, such as irregular heartbeat or shortness of breath.
The experts noted that detecting iron deficiency on time and initiating immediate treatment is necessary for women's better health.
Management of iron deficiency includes
- improving diet and taking iron supplements as advised by any expert
- Have iron-rich foods like spinach, beans, lentils, nuts, and dates
- Vitamin C–rich foods, such as oranges and lemons.
© 2024 Bennett, Coleman & Company Limited

