- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Parkinson’s Patients May Soon Walk Better With This New Personalized Brain Therapy

(Credit-Canva)
Being a retired accountant, Mr. John Smith only had a history of high cholesterol and high blood pressure in this health history. Although he never smoked and only had alcohol occasionally, Mr. Smith didn’t know what the future held for his health. After being evaluated by a neurologist, Mr. Smith was faced with a Parkinson’s diagnosis. He first began experiencing symptoms of tremors, stiffness, and difficulty with balance and co-ordination about five years before his diagnosis. He had been treated with a combination of medication however, he saw no improvement.
This 2023 case study is just one of many that shows the realities of dealing with Parkinson’s. Despite years of treatment, many times people see no improvement. Will this change? Study shows that it might. A new study shows that a customized treatment could help Parkinson’s patients improve their movement.
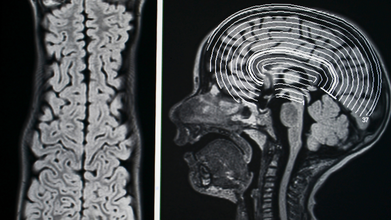
Parkinson's disease often makes it really hard for people to walk well. They might develop a shuffling walk, often called "Parkinson's gait," which makes them more likely to fall and harder to move around on their own. But new research points to an exciting solution: a treatment called deep brain stimulation (DBS) that's custom-made for each patient's brain and walking style.
Personalized Deep Brain Stimulation
The study found that by carefully changing the brain stimulation based on things like how long someone's steps are, how fast they walk, and even how much their arms swing, their overall movement got much better. Researchers reported these findings in the journal npj Parkinson’s Disease.
However, medical research shows that ‘one-size-fit-all’ solutions are not always helpful, especially when it comes to neurological issues. The reason why this is a big step is because this treament means doctors can tailor the treatment to fit each person perfectly. The scientists hope this personalized approach will lead to smarter and more effective treatments not just for Parkinson's, but for other brain conditions too. It's all about making the technology work just right for each individual.
How Deep Brain Stimulation Works
Deep brain stimulation (DBS) uses a small device placed inside the body. It sends gentle electrical signals directly to specific parts of the brain. These signals essentially give the brain a "jump start," helping it control movements better. DBS has been very good at easing common Parkinson's symptoms like shaking, stiffness, and slow movements. However, it hasn't always been as consistent in helping with walking problems, which is why this new research is so important.
Parkinson's disease is a condition that slowly gets worse over time, affecting how people move. It causes symptoms like shaking, stiff muscles, and trouble with balance and coordination. These issues happen because certain brain cells that make a chemical called dopamine either die or get damaged. Dopamine is essential for smooth and controlled movements.
Creating a "Walking Scorecard"
For this study, researchers worked closely with three Parkinson's patients to figure out how to make DBS better at helping with walking. During clinic visits, patients walked in a loop while scientists carefully changed their DBS settings. At the same time, they recorded the patients' brain activity and how they moved.
Using all this information, the researchers created something called a "walking performance index" (WPI). It is a detailed score that shows exactly how Parkinson's is affecting a person's movement. Using this the team also found specific patterns of brain activity, especially in a brain area called the globus pallidus, that were linked to better walking. This part of the brain is known to be involved when muscle control is lost in Parkinson's. The WPI proved to be a reliable way to measure and improve walking, helping them find the best personalized DBS settings for each patient.
Automated and Smarter DBS
Looking ahead, the researchers are working on creating automated systems. These systems would be able to capture details about how a person walks in real-time, even during their daily life. This information would then be sent directly to the software that controls the DBS device. By using the WPI, these smart systems could automatically make exact adjustments to the brain stimulation. This could lead to even better and more consistent improvements in walking for people with Parkinson's, making the technology even more responsive and personalized.
THIS Seizure Could Make You Dance Without Warning
Credits: Canva
Dr Sermed Mezher, a UK-based General Practitioner, best known for his educational medical content on social media shared a video on his Instagram of a seizure that could leave you dancing.
"Wakeful seizures like that are more common than you think," he says. "But how are they different to the dancing plague?"
He explains that dancing plague happened around 1518, when a woman named Frau Toffer started dancing uncontrollable on the streets and then eventually hundreds also joined her. They danced for days, and some of them actually died of exhaustion. There are multiple theories to it, including ergot poisoning. However, he says, "We need to remember that this population was riddled with starvation and diseases. They had seen multiple outbreaks of the black plague, so the most likely diagnoses is stress-induced mass hysteria or a type of stress-induced psychosis."
However, he notes that the video he is referring to is different. "What this person in the first video was experiencing were temporary abnormal movements while conscious, that might be classed as a non-epileptic seizure."
What Is A Non-Epileptic Seizure?
It is also known as functional seizures, which are episodes that look and feel like seizures caused by epilepsy However, they are not caused by abnormal electrical activity in your brain, but are a physical reaction of your nervous system to:
- Physical triggers like injury or pain
- Stressors in your environment
- Past traumatic event
While the dramatic dancing may seem like you are "faking" it, but the seizures are real and the person who is experiencing do not have any voluntary control over these episodes.
What A Non-Epileptic Seizure May Look Like?
The common symptoms of non epileptic seizure are:
- Loss of consciousness
- Seizures over 10 minutes long
- Retained awareness
- Out of phase limb movements
- Pelvic thrusting
- Changing patterns of movement
- Rapid side to side head movements
- Eyes closed unresponsiveness
This can also affect your emotional state, including your anxiety, depression and even your panic attacks.
What Might Cause Non Epileptic Seizure?
These are caused by a mix of stress that affects your body, mind, and relationships. This is known as the biopsychosocial model.
Other things that may contribute include:
- Difficulty understanding and expressing emotions
- Trouble processing information from your senses to turn it into movement
- Unhelpful response to stressors
Furthermore there could be underlying mental health conditions that could trigger these seizures. The conditions include:
- Mood disorder
- Personality disorder
- Post Traumatic Stress Disorder (PTSD)
- Anxiety disorders with panic attacks
- Depressive disorder
- Dissociative disorder
- Somatic symptom disorder
- Substance use disorder
People who undergo these seizures may be more at risk of experiencing physical, sexual or emotional abuse or neglect, especially in their early years. They may have lived through a difficult or traumatic event, and may have or develop a chronic condition like chronic pain or fibromyalgia.
Does Anyone In Your Family Hoard? It Might Be More Than Just Keeping Too Much Stuff, According To Expert

Credits: Canva and Instagram
A video that is making rounds on social media, shared by stand-up comedian Hasan Minhaj is a conversation between him and behavioral change expert Mel Robbins. The two dove deep into something that many families may also deal with but do not ever say : hoarding.
What started as a funny story about Minhaj's mother holding onto old VHS tapes turned into an emotional discussion about memory, loss, and the human need for control.
Minhaj said that his mom still has "VHS cassette tapes stacked up in the guest room", including the 1996 movie Dunston Checks In, which he loved as a child. "We don't even have a VHS player. My children won't watch VHS, I loved that movie in 1996, but I am 39 now, we gotta move on."
However, he shares that when he tried to throw it away, it led to what he described as "nuclear war". Robbins immediately pointed out why: "She has transferred her own emotional attachment to physical objects. It is not a cassette tape, it represents something else."
Robbins explained that hoarding often is not about the objects themselves, but the about being emotionally stuck on it. She noted that "there's a very close connection between depression, OCD, and hoarding. You're dealing with a mental issue that manifests in things." This is why clutter becomes a coping mechanism, this is a way to stay in control, when other areas of life feel uncertain.
When Minhaj mentioned that his mom keeps even outdated software like Windows XP CDs, she said that the reason she is holding on to all these is because he does not call her enough. "If you do not call enough, the things remind her of you... it might remind her of a time when you lived at home, when you were younger. If she holds on to it, she stays in control."
Robbins also told Minhaj, that the habit of his mother hoarding "is not driving her crazy", but it is driving him "crazy".
Why Someone May Hoard
As per the NHS UK, the reason why someone begins hoarding could be a symptom for another condition. It could be well associated with severe depression, psychotic disorders, such as schizophrenia, or obsessive compulsive disorder (OCD).
As per a 2015 study published in the Journal of Clinical Psychiatry, hoarding behaviors occur in a variety of neuropsychiatric disorders, including OCD, schizophrenia and dementia. The act of hoarding is defined as a pattern of persistent difficulties with discarding personal possessions, even those with no clear value. In Minhaj's mother case, it is the VHS cassettes, and software CDs.
Who Is At Risk?
As per Harvard Health, it affects approximately 2 to 6% of the adult population, across genders. However, hoarding is more common in an individual who live alone. Hoarding also occurs three times as often in older adults as in the general population.
What Can Be Done?
Cognitive behavioral therapy or CBT is an option that can be considered. It focuses on addressing cognitive distortions related to fear of discarding and urges to acquire, while the behavioral component focuses on sorting through and discarding materials in a systematic and structured way.
New Study Suggests Targeting Belly Fat Can Prevent Prediabetes

Credits: Canva
Where fat accumulates in the body can be far more important than simply shedding pounds when it comes to lowering diabetes risk, a new study published in Nature suggests. For people with prediabetes, which is when blood sugar is higher than normal but not yet at diabetes levels, targeting belly fat specifically may have a greater impact than losing weight overall through lifestyle changes.
Halting prediabetes is critical, as nearly 70 percent of individuals in this category eventually develop diabetes. Reversing prediabetes also protects against complications like heart disease, kidney problems, and nerve damage.
What About Study Findings?
In the study, two groups of participants had similar overall fat levels but differed in how fat was stored. Those who lost more belly fat, or visceral fat, over a year were able to reverse prediabetes, while those who didn’t reduce abdominal fat did not reach healthy blood sugar levels.
Researchers from the University Hospital Tübingen in Germany found that focused lifestyle changes could bring prediabetic individuals into remission even without major weight loss. This remission was associated with a roughly 70 percent reduction in the risk of developing Type 2 diabetes over the following decade.
Among 1,105 participants with prediabetes, the study examined 234 individuals who did not lose overall weight. Of these, 51 achieved prediabetes remission after a year of targeted lifestyle interventions, while the remaining 183 did not reach healthy glucose levels.
Does This Study Hold Lessons for Indians?
“Weight loss remains the primary goal for people who are obese. However, reversing prediabetes can also happen without major weight loss, especially when lifestyle interventions focus on improving diet quality, increasing physical activity, and building muscle while reducing fat,” says Dr. Anoop Misra, chairman at Fortis C-Doc Hospital for Diabetes and Allied Sciences.
He adds that for Indians, reducing both subcutaneous abdominal fat and visceral fat is key for better metabolism. These changes, paired with increased muscle mass and improved functional capacity, enhance insulin sensitivity and help maintain long-term blood sugar control.
Why Abdominal Obesity Is a Priority
Belly fat, or visceral fat, releases inflammatory substances that interfere with insulin, the hormone that moves sugar from the blood into cells. To compensate, the body produces more insulin, which can overwhelm the pancreas and raise blood sugar. Excess sugar is often stored as fat around the abdomen, which is why even individuals of normal weight with a protruding stomach are at higher risk of diabetes.
What Lifestyle Interventions Help Reduce Belly Fat?
“Diet composition matters most lower carbs, higher protein, and healthy fats, all within a controlled calorie range, can help reverse prediabetes even without significant weight loss,” says Dr. Misra. Good carbohydrate sources include whole grains, fruits, legumes, and non-starchy vegetables, while healthy fats come from nuts, seeds, olive oil, and fatty fish.
Physical activity also plays a crucial role. Combining resistance training, such as weightlifting at least twice a week, with aerobic exercises like walking, running, or swimming, is effective at reducing visceral fat. Adequate sleep around seven hours per night is also essential to keep blood sugar levels under control.
© 2024 Bennett, Coleman & Company Limited

