- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Seeing A Loved One Age Is Difficult, Here Are 8 Signs It's Time For Memory Care

Image Credits: Canva
Aging is a natural yet bittersweet process. Watching a loved one age can be both happy and sad, particularly when the onset of cognitive decline starts impacting their independence. A mother who was a master baker may begin to forget how to make her favorite recipes. A father who loved doing crosswords may no longer be able to write his answers neatly. These little things may initially be manageable, but they can continue to deteriorate, creating major safety issues.
Identifying these signs may be challenging, but moving a loved one to memory care is usually the most sound decision for their safety and well-being. Memory care communities offer tailored care plans, stimulating activities to promote mental function, and a supportive setting where seniors can live with dignity.
If you think it's time for memory care, speak with a healthcare provider for advice. Getting expert opinion and reviewing options for care can aid in making a sound decision to provide the highest quality of life for your loved one.
Dementia illnesses like Alzheimer's disease progressively affect memory, judgment, and activities of daily living. Eventually, family members may struggle to provide the level of support needed, making memory care an inevitable move. But when do you know? These are eight telltale signs that your loved one needs professional memory care.
1. Difficulty with Activities of Daily Living
As the dementia advances, it can become more and more challenging for the person to master simple activities of daily living (ADLs). Dressing, bathing, and cooking may become too much. A few definite signs that your loved one may require memory care are:
- Forgetting meals and drinks and losing weight or becoming dehydrated.
- Failing to dress appropriately for the weather or being unable to manage buttons and zippers.
- Having trouble with personal grooming and bathing.
- Incontinence problems or difficulty using the bathroom alone.
When these challenges become the norm, the structured support given in a memory care community can provide for their needs with dignity and respect.
2. Visible Changes in Behavior
Dementia can cause unpredictable mood swings and personality shifts. If your loved one exhibits increasing agitation, paranoia, or withdrawal from social interactions, it could be a sign that their cognitive condition is worsening. Studies show that up to 50% of Alzheimer’s patients experience agitation, which may stem from brain deterioration or external triggers such as overstimulation.
Common behavioral changes include:
- Paranoia and distrust of family members or caregivers.
- Difficulty concentrating or making decisions.
- Decreased interest in activities once found to be enjoyable.
- Increased combativeness or aggression.
Memory care communities are created to offer structured routines and soothing atmospheres to assist in controlling these emotional and psychological changes.
3. Wandering and Disorientation
One of the most problematic indicators of advanced dementia is wandering. People can go out and get lost, disoriented, or even put themselves in harm's way by crossing into traffic or inclement weather. If wandering is a constant problem, memory care facilities provide a safe setting with specialized design elements like alarmed doors and interiorized outdoor areas to contain risks.
4. Physical Deterioration and Grooming
Alzheimer's and dementia don't just impact memory—they can also affect physical health. If your loved one is losing weight, becoming frail, or not taking care of personal hygiene, it may be a sign that they need professional help.
Some warning signs to watch out for are:
- Unintentional weight loss because they have forgotten to eat.
- Untidy appearance, like wearing dirty clothes or not brushing their hair.
- Sleep disturbances, resulting in fatigue and crankiness.
Memory care centers offer balanced meals, personal care help, and medical monitoring to promote overall health.
5. Ineffective Medication and Health Management
Medication management is essential for older adults, but people with dementia might forget to take their medication or overdose on it inadvertently. Ineffective medication use can cause health issues to worsen, such as cardiovascular disease, infections, and further loss of cognitive function.
In a memory care center, the staff monitors medication routines so that the residents take the correct dose at the right time to avoid complications.
6. Increased Difficulty with Communication
Cognitive impairment tends to interfere with communication abilities. Your loved one might have trouble thinking of the right words, speak repeatedly, or send confusing voicemails and messages. Repetitive speech, disorientation in conversations, and inability to communicate needs may become frustrating for both the person and their caregivers.
Memory care communities employ professionals who are trained in communication strategies to assist residents in effective expression and preservation of self.
7. Caregiver Burnout
Full-time care of a person with dementia is both physically and emotionally draining. Caregiver burnout is a frequent occurrence with signs of stress, anxiety, depression, and exhaustion. If you are overwhelmed, finding it difficult to keep up with duties, or experiencing negative feelings toward caregiving, then it may be time to explore memory care.
Memory care homes not only help seniors but also free up family caregivers, enabling their loved ones to receive high-quality care and providing them with peace of mind.
8. Safety Risks at Home
The home setting can now be unsafe for a person with progressing dementia. Tripping, kitchen accidents, not turning off the stove, or wandering outdoors without supervision are all significant threats. Memory care communities incorporate safety features like secure entryways, fall-preventative protections, and emergency response systems to safeguard residents.
Witnessing a loved one battle dementia is never pleasant. Yet, knowing when professional care is essential can give them a safer, more relaxing setting where they can receive the specific attention that they need. Memory care is created to promote quality of life, providing a structured, compassionate environment that benefits both seniors and families.
World Misophonia Awareness Day 2025: Why Misophonia Makes Everyday Sounds Feel Like An Attack—Here’s What It Does To The Brain

Credits: Health and me
You're at the dinner table and someone slurps soup, another begins tapping a pen, and your heart begins racing, your muscles lock up, and you're filled with fury you can't explain. If this sounds familiar, you're not being "too sensitive." You may be one of millions dealing with misophonia, a little-understood sensory disorder finally receiving long-overdue notice.
On July 9, World Misophonia Awareness Day, experts and advocacy groups are urging for global recognition of this condition that impacts almost 1 in 5 adults, but too often remains misunderstood or undiagnosed. Initiated by non-profit soQuiet, the day is dedicated to advancing discussion, research, and support for those whose lives are deeply affected by what the rest of us tune out—usual, ordinary sounds.
What Is Misophonia?
Misophonia, literally "sound hatred," is more than not liking noise. It's an intense, automatic emotional and physical response to certain sounds, usually created by someone else. Chew, sniffle, heavy breathing, throat clearing, even pen clicking.
These stimuli trigger strong reactions in individuals with misophonia, from annoyance, stress, and revulsion to outright panic or fury. For some, it's a single stimulus. For others, it's multiple. The psychological weight can be overwhelming, so that everyday encounters such as dining at a restaurant or working in an open office become a daily war.
And though most people write it off as being irritable or melodramatic, the science disagrees.
An increasing amount of research is revealing what's actually going on in the brains of individuals with misophonia. A 2022 study published in Frontiers in Neuroscience indicates that misophonia is potentially associated with a specific "neural signature"—unique brain pathways that are more active in perceiving sound and emotion.
In misophonics, increased interconnectivity between the sound-processing auditory cortex and the emotion-regulating limbic system may be what makes some sounds ring alarm bells. It's a brain in overdrive, responding in the same way to a throat clear or chewing noise as it would to a bodily threat.
A reflexive fight-or-flight response—hands sweat, heart throbs, and logical thinking yields to a frantic need to flee or strike out.
Why Misophonia Is Unheard And Misunderstood?
Perhaps one of the most infuriating things for people with misophonia is that others just don't get it. It doesn't help that they are invisible and their reactions are usually termed overreactions, even rudeness.
Worse still, it has the potential to overlap with or be confused with other mental illnesses such as OCD, anxiety, PTSD, or even autism spectrum disorders. That is why diagnosis becomes complicated and many suffer silently, particularly older people who might have spent decades without ever hearing the term "misophonia."
The stigma may result in isolation, strain on relationships, and depression, particularly when individuals are stuck in environments where they cannot escape to be safe from trigger sounds—such as school, work, or home mealtime.
Misophonia is not just about being uncomfortable—it's about survivability. Most with the condition report avoiding parties, leaving jobs, or having trouble with day-to-day activities just to prevent exposure to triggers. Picture wearing noise-canceling headphones just to get through your workplace. Or having every meal in solitude, because even the sound of eating is too much. In a world that's getting noisier, adaptation is a full-time profession.
How Misophonia Affects the Brain?
Misophonia's not so much about what you're hearing—it's about how your brain interprets that sound. New research indicates that individuals with misophonia exhibit heightened activity and connectivity within brain areas that handle sound processing, emotional control, and the body's defense mechanism.
One of the most important regions engaged is the anterior insular cortex, which assists you in assessing the emotional meaning of sensory input. In misophonia, this region seems to hyperreact, sending messages that something harmless—such as someone chewing—is threatening. This activates the limbic system, which controls emotion and survival reactions, placing the individual in a fight-or-flight state very quickly.
Imagine it like a smoke alarm blaring at burnt toast like it is a raging house fire. That exaggeration is what makes misophonia so debilitating. A person with misophonia has a complete body stress response when they hear a trigger sound, even though rationally, they know the sound is not harmful.
Brain imaging studies suggest this is not about overreacting by choice—it’s a neurological mismatch, where emotional and auditory systems are too tightly wired together. That’s why even brief exposure to trigger sounds can feel unbearable and linger long after the sound stops.
Common Trigger Sounds of Misophonia
Misophonia triggers are different for different people but most follow predictable patterns. They're not loud or startling noises—they're typically repetitive, mundane sounds easily tuned out by other people but for the misophonic person, which can trigger an almost immediate adrenaline rush of anger, panic, or disgust. The following are the most typical categories of trigger sounds:
Drinking and eating noises: Smacking lips, slurping, chewing, gulping, crunching, and loud swallowing are the worst. Chewing gum is a very frequent offender.
Sounds associated with breathing: Sniffling, heavy breathing, nose blowing, or snoring are common culprits. Even a faint wheeze can be offending for some.
Sounds of the mouth and throat: Throat clearing, coughing, yawning, or audible kissing sounds.
Repetitive sounds of activity: Tapping on the pen or feet, mouse clicking, typing, drumming fingers, or even paper or plastic bag rustling.
Environmental and ambient sounds: Ticking clock, ringing telephone, dripping water, or sounds of animals such as barking.
Surprisingly, several individuals comment on how the proximity or origin of the noise is important. A TV chewing noise might be mildly annoying—but if it's coming from someone sitting directly next to them, the response can be volcanic. This serves to illustrate that misophonia is not about the sound type or volume but also relationship, context, and physical proximity.
Knowing these triggers can inform treatment and coping mechanisms, particularly when seeing therapists and learning to recognize patterns and decrease emotional reactivity over time.
Is Misphonia Treatable?
Misophonia is finally being studied, understood, and treated. Cognitive Behavioral Therapy (CBT) is showing promising results. A 2020 study published in Depression and Anxiety found that more than a third of patients undergoing CBT saw a meaningful reduction in misophonia symptoms—and these improvements held up a year later.
CBT involves finding individual noise triggers and reframing the emotional response to them. It's training the brain to break the anxiety or anger spiral, not allow it to get the best of you. In extreme cases, therapy is also paired with anti-anxiety medication to decrease reactivity, particularly when CBT alone doesn't work. Other coping strategies are:
- Wearing noise-canceling headphones
- Using white noise machines or soothing background music
- Deep breathing or muscle relaxation exercises
Why is Family and Social Support Important?
For individuals with misophonia, having family members know what the condition is and what it's like makes a huge difference. Family members tend to unwittingly become trigger points—chewing at the dinner table, throat clearing, playing music out loud.
Dismissal and blame only exacerbate the emotional toll. Specialists maintain that education and compassion are essential. Accepting that the response is involuntary—and not a personal affront—is critical. Offering professional assistance and using supportive measures in the home can assist in creating safe, respectful spaces for those affected.
World Misophonia Awareness Day isn't only for patients—it's for everyone. By recognizing that some sensory stimuli can be triggering, offices, schools, and public places can start to make changes that are inclusive.
Misophonia isn't a trait, it's a real, life-changing condition that's worthy of attention and understanding. As the research expands and the stories get out there, we get closer to a world where individuals with misophonia don't merely exist—but thrive.
UK Health Officials Issue A Public Warning And Safety Guidelines Against These Bugs That Cause Lyme Disease

(Credit-Canva)
As an unexpected wave of heat hits the UK, many people have been concerned regarding not just heat-illnesses, but also other issues that arise mostly in the summer season.
The UK Health Security Agency (UKHSA) has issued a public warning against a small, almost invisible threat that could send you to the hospital. Taking simple steps can help you avoid these bugs that could leave you with flu-like symptoms lasting for weeks.
The Hidden Danger: Ticks
Ticks are small bugs often found in woods, grassy areas, and moorlands. The reason why the volume of these bugs is more prevalent in these grassy areas is because it is easier to find and feed off other creatures there. These bugs are known to spread Lyme disease, a bacterial infection. You get it when a tick bites you and feeds on your blood, which can lead to flu-like symptoms. Not all ticks carry Lyme disease, though. It's usually easier to treat if caught early, but if it goes unnoticed, problems can worsen, causing joint pain, nerve issues, and memory problems.
Lyme Disease Treatment
The chances of getting sick are fairly low, as not all ticks carry the bacteria that cause Lyme disease. If you've been bitten, keep a close eye on the bite area for symptoms, especially the well-known "bullseye" rash. This rash can appear up to three months after a bite, but usually shows up within one to four weeks.
If a doctor thinks you might have Lyme disease, they'll prescribe antibiotics. The type you get depends on your symptoms, and you might need to take them for up to 28 days. It's very important to finish the entire course, even if you start feeling better. For severe symptoms, you might be sent to a hospital specialist to receive antibiotics directly into a vein.
A small number of people who are treated for Lyme disease continue to have symptoms like tiredness, aches, and low energy for years. These symptoms are often compared to conditions like fibromyalgia and chronic fatigue syndrome.
What to Do If You're Bitten
Tick bites might not hurt at first because ticks put a numbing substance into your skin, so you might not even notice you've been bitten. If you do find a tick, it's important to take it out the right way: use fine-tipped tweezers or a special tick-removal tool, grasp the tick as close to your skin as you can, and pull it slowly upwards without squeezing it. Never try to pull it out with your fingers, as this can leave part of the tick in your skin and cause an infection. After removing the tick, clean the bite area with antiseptic or soap and water.
Simple Prevention Tips
Health officials recently shared advice on how to protect yourself from these tiny parasites. They suggest simple actions are best to prevent tick bites:
- Regular checks are your best defense. While you're outside, brush off any ticks you spot right away.
- Do another check when you get home. Focus on exposed skin and any clothes where these bugs might be clinging.
- Don't forget to check children and pets, as they can't check themselves.
- Use an insect repellent that specifically prevents ticks.
- Wear long sleeves and long trousers when outdoors to reduce direct skin contact.
- When possible, stick to clearly marked paths and avoid brushing against plants where ticks might be hiding.
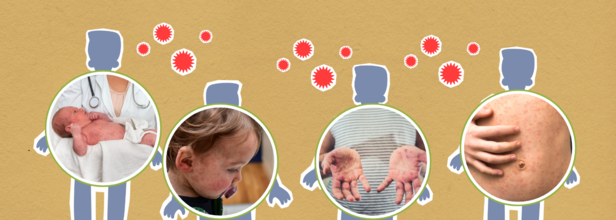
Even After The Elimination Of Measles In 2000, Why Is US Struggling With It Today?
Credits: Canva
The United States is facing its worst measles outbreak in 25 years, with more than 1,270 confirmed cases reported so far this year—surpassing the previous high of 1,274 cases in 2019. The data, compiled by Johns Hopkins University, has raised alarms among health officials, who believe the actual number of infections may be even higher due to underreporting.
Tragically, three people have died from the virus this year—two children in Texas and one adult in New Mexico. All of them were unvaccinated.
“This move will further fuel the spread of vaccine-preventable illnesses,” said Dr. Bruce A. Scott, president of the American Medical Association, referencing ongoing declines in vaccination rates and policy shifts that threaten public health.
From Elimination to Outbreak
Measles is one of the most contagious diseases known and was declared eliminated in the United States in 2000, thanks to the widespread use of the MMR (measles, mumps, rubella) vaccine. However, current outbreaks suggest a reversal of that progress.
The largest outbreak this year began in January in Gaines County, West Texas—a region with one of the lowest vaccination rates in the state. So far, that outbreak alone has led to over 750 confirmed cases and has spread to neighboring areas in New Mexico and Oklahoma, with possible links to Kansas.
Shockingly, nearly one in four kindergartners in Gaines County did not receive their required MMR vaccine during the 2024–25 school year.
Spread Through Travel and Everyday Contact
Measles spreads easily through airborne droplets when an infected person coughs, sneezes, or talks. The virus can also live on surfaces like doorknobs for several hours, making it especially hard to contain.
Air travel has further complicated containment efforts. In Colorado, an out-of-state visitor unknowingly spread the virus while contagious, leading to multiple cases—including individuals who were only at the airport at the same time.
According to the CDC, nearly 1 in 8 people infected this year required hospitalization, and about 30% of all cases have been in children under the age of five. Most of these children were unvaccinated.
The Role of Vaccination
The MMR vaccine remains the most effective tool against measles. One dose offers 93% protection, while two doses provide 97% protection.
In response to the crisis, some states have taken emergency steps to protect infants. Several have lowered the age for the first MMR shot from 12 months to 6 months. The results have been encouraging—early vaccination rates among 6-month-olds in Texas are now eight times higher than in 2019.
New Mexico has also seen a significant rise in vaccination, and both states are working hard to protect their most vulnerable populations.
Still, nationwide vaccination rates remain below targets. The U.S. aims for 95% of kindergartners to receive both doses of the MMR vaccine, but this benchmark has been missed for the past four years. In the 2023–24 school year alone, over 125,000 kindergartners lacked at least one required vaccine.
A Shifting Public Health Landscape
Public health experts are concerned that growing distrust in vaccines and leadership changes at the federal level may further undermine efforts to control the disease.
As of now, the CDC does not have a permanent director in place, and U.S. Health and Human Services Secretary Robert F. Kennedy Jr.—a long-time vaccine skeptic—has made controversial decisions. Though he recently expressed support for vaccines, his previous statements and the removal of key expert panels have left public health officials worried.
If outbreaks linked to the Texas region continue into 2026, the U.S. risks losing its measles elimination status. Experts say rebuilding public trust in vaccines and boosting routine childhood immunizations must become a national priority—before the disease becomes even harder to contain.
© 2024 Bennett, Coleman & Company Limited

