- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Shubhanshu Shukla Returns From ISS, What All Medical Examinations Are Lined Up

Shubhanshu Shukla, the Indian Air Force Group Captain is back on Earth after spending 18 days aboard the International Space Station (ISS). What now awaits is a long list of medical examination to ensure that Shukla and the other astronauts from Poland and Hungary are in good health.
What Are The Post-flight Medical Examinations For Astronauts?
The journey back from space marks the start of a whole new phase for astronauts. Just after splashdown, Group Captain Shukla and his fellow crewmates were helped out of the capsule by SpaceX recovery teams. Once aboard the recovery vessel, they underwent initial medical checks to assess their vital signs and general health.
These immediate tests are part of a broader post-flight health monitoring protocol aimed at studying how spaceflight affects the human body. Since astronauts’ health parameters are recorded before launch, comparing them with post-landing data helps scientists understand the impact of microgravity on various body systems.
Also Read: After Jannik Sinner, Tara Moore Makes News Failing Her Doping Test, Resulting In A 4-Year Long Ban
As the pilot of the Axiom-4 mission, Shukla will undergo an extensive series of assessments — from cardiovascular and immune system checks to balance, coordination, and psychological evaluations.
Over the coming weeks, both NASA and the Indian Air Force will monitor his physical and mental recovery closely.
Readjusting to Earth’s gravity is not instant. In space, the lack of gravity leads to muscle weakening, bone density loss, and a fluid shift in the body that can affect circulation and organ function. To counter this, astronauts follow a personalized reconditioning plan designed to help their bodies re-adapt. These programmes focus not only on regaining strength but also on retraining the body’s proprioception — the sensory system that allows us to sense our position and movement, which becomes disoriented in space.
Life in Microgravity: What It Feels Like
Speaking from the International Space Station during the mission, Shukla had shared the strange feeling of disorientation he experienced during his initial days in orbit. “It’s the first time for me, so I don’t know what to expect [upon return],” he said. “The only hope is — I did have some symptoms coming up — so I am hoping that I will not have it going down. Unless and until I get the worst of both worlds and I get it both the times.”
Also Read: Veteran Actor Dheeraj Kumar Dies At 79 Due To Acute Pneumonia
Many astronauts deal with “space motion sickness” during the early days of their mission. This occurs when the brain receives mixed signals from the inner ear, which is crucial for balance on Earth. Upon return, the challenge reverses — as the body tries to function under the force of gravity again, simple actions like standing or walking can temporarily become difficult.
According to official reports, Shukla and his team will soon be transported to NASA’s Johnson Space Center in Houston for further recovery and evaluation, either by sea or air.
Post-Flight Rehabilitation
As per Polash Sannigarhi, Chief Instructor, Aeromedical, Training Center, Air Force Station Hindan, Ghaziabad, there are many rounds of medical checks that an astronaut undergoes. Being a flight surgeon himself, he writes in the paper, "Post-flight rehabilitation of an astronaut after long duration mission in space: Through the eyes of a flight surgeon" published in 2023.
Post-flight Medical Evaluation
Medical assessments begin within a day of landing (R+1) and cover a wide range of investigations:
Laboratory Tests: Conducted per NASA’s MEDB guidelines to assess biochemical and physiological parameters.
Physical Examination: Daily systemic check-ups by a flight surgeon to monitor overall health.
Anthropometry: Measurement of height and body mass to assess fluid shift and skeletal changes.
Psychological Assessments: Conducted privately by a mission psychologist on R+1 and R+10.
Sensorimotor and Vestibular Tests: Includes dynamic posturography and mobility assessments to evaluate balance and spatial orientation.
Ophthalmologic and Audiological Tests: Exams such as visual acuity, contrast sensitivity, orbital MRI, and audiometry.
Cardiorespiratory Assessment: ECG post-landing and spiro-ergometry on R+5 to assess VO₂ max.
Nutritional, Radiation, and Sleep Assessments: Involves dietary surveys, urine and blood sampling, dosimeter analysis, and sleep quality tracking.
Radiological Imaging: Targeted MRIs and ultrasounds are performed based on clinical indications.
Post-flight Physical Rehabilitation
This begins as early as the first day post-landing and is tailored to individual needs. A multidisciplinary team — including a Flight Surgeon, Physiotherapist, and Exercise Specialist — oversees it.
Initial Days (R0–R+1): Massage therapy for muscle relaxation.
R+2 to R+7: Structured exercise routines, including warm-ups, back and leg activation exercises, gait training, balance drills, and posture work using equipment like resistance bands.
Hydrotherapy (Following Week): Aquatic activities like aqua jogging and ball games mimic microgravity and help recondition muscles in a low-impact environment.
Core anti-gravity muscles such as the multifidus and transversus abdominis are monitored using ultrasound to track structural recovery. Flexibility and proprioception exercises are gradually reintroduced. Astronauts avoid jumping or high-impact activities until deemed fit by the team.
Each day concludes with team reviews to adapt the next day’s plan based on physical response. The program’s primary goal is to return astronauts to their pre-flight physical condition safely, without overexertion or injury.
Men Lose Their Y Chromosomes As They Age, Here's Why It Matters
Credits: Canva
For decades, scientists believed the gradual loss of the Y chromosome in ageing men did not matter much. But a growing body of research now suggests otherwise. Studies show that losing the Y chromosome in blood and other tissues is linked to heart disease, cancer, Alzheimer’s disease and even shorter lifespan. The crux is simple but striking. As men age, many of their cells quietly lose the Y chromosome, and this loss may be shaping men’s health in ways we are only beginning to understand.
Aging And The Disappearing Y Chromosome
Men are born with one X and one Y chromosome. While the X carries hundreds of important genes, the Y is much smaller and contains just 51 protein coding genes. Because of this, scientists long assumed that losing the Y in some cells would not have serious consequences beyond reproduction.
However, newer genetic detection techniques tell a different story. Research shows that about 40 percent of men aged 60 have some cells that have lost the Y chromosome. By age 90, that number rises to 57 percent. Smoking and exposure to carcinogens appear to increase the likelihood of this loss.
This phenomenon, known as mosaic loss of Y, does not occur in every cell. Instead, it creates a patchwork in the body where some cells carry the Y chromosome and others do not. Once a cell loses the Y, its daughter cells also lack it. Interestingly, Y deficient cells seem to grow faster in laboratory settings, which may give them a competitive edge in tissues and even in tumors.
Why Would Losing The Y Matter?
The Y chromosome has long been viewed as mainly responsible for male sex determination and sperm production. It is also uniquely vulnerable during cell division and can be accidentally left behind and lost. Since cells can survive without it, researchers assumed it had little impact on overall health.
Yet mounting evidence challenges that assumption. Several large studies have found strong associations between loss of the Y chromosome and serious health conditions in older men. A major German study reported that men over 60 with higher levels of Y loss had an increased risk of heart attacks. Other research links Y loss to kidney disease, certain cancers and poorer cancer outcomes.
There is also evidence connecting Y loss with neurodegenerative conditions. Studies have observed a much higher frequency of Y chromosome loss in men with Alzheimer’s disease. During the COVID pandemic, researchers noted that men with Y loss appeared to have worse outcomes, raising questions about its role in immune function.
Is Y Loss Causing Disease?
Association does not automatically mean causation. It is possible that chronic illness or rapid cell turnover contributes to Y loss rather than the other way around. Some genetic studies suggest that susceptibility to losing the Y chromosome is partly inherited and tied to genes involved in cell cycle regulation and cancer risk.
However, animal research offers stronger clues. In one mouse study, scientists transplanted Y deficient blood cells into mice. The animals later developed age related problems, including weakened heart function and heart failure. This suggests the loss itself may directly contribute to disease.
A New Chapter In Men’s Health
So how can such a small chromosome have such wide ranging effects? While the Y carries relatively few genes, several of them are active in many tissues and help regulate gene activity. Some act as tumor suppressors. The Y also contains non coding genetic material that appears to influence how other genes function, including those involved in immune responses and blood cell development.
The full DNA sequence of the human Y chromosome was only completed recently. As researchers continue to decode its functions, the message for men’s health is becoming clearer. Ageing is not just about wrinkles or grey hair. At a microscopic level, the gradual disappearance of the Y chromosome may be quietly influencing heart health, brain health and cancer risk.
Understanding this process could open new doors for early detection, personalized risk assessment and targeted therapies that help men live longer and healthier lives.
Udit Narayan’s First Wife Alleges She Was Forced to Undergo Hysterectomy, Files Police Complaint
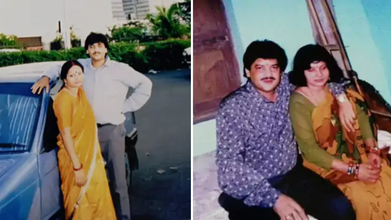
Credits: Facebook
First wife of singer Udit Narayan, Ranjana Narayan Jha made serious allegations against him, claiming that he forced her to get hysterectomy. She filed a police complaint earlier this week at the Women's Police Station in Supaul district, Bihar.
She accused Udit Narayan and his two brothers Sanjay Kumar Jha and Lalit Narayan Jha and his second wife Deepa Narayan of a criminal conspiracy that lead to hysterectomy - the surgical removal of uterus, without her knowledge. As per an NDTV report, "She claimed she became aware of this only years later during medical treatment."
Udit Narayan's First Wife's Allegations
As per the complaint, Udit and Ranjana were married on December 7, 1984, in a traditional Hindu ceremony. Udit then moved to Mumbai in 1985 to pursue his music career. She later learned through media that he had married another woman Deepa. As per the complaint, he continued to mislead her whenever she confronted him.
As per the complaint, in 1996, she was taken to a hospital in Delhi under the pretext of medical treatment, where, she claims that her uterus was removed without her knowledge. She said that she was compelled to file a complaint years after being ignored. "You all know that Udit Narayan ji repeatedly makes promises but does not fulfill them. He has not done anything till now, which is why I have come to the Women's Police Station. I deserve justice," she said.
"Nowadays, I am constantly unwell and need his support. But Udit Narayan is neither saying anything nor doing anything. He came to the village recently and left after making promises once again," she said, as per a Hindustan Times report.
What Is Hysterectomy?
It is the surgical removal of one's uterus and cervix. There are different kinds of hysterectomy available, which depends on the condition of the patients.
Total Hysterectomy
This removes uterus and cervix, but leaves ovaries. This means the person does not enter menopause after the surgery.
Supracervical Hysterectomy
Removing just the upper part of the uterus and leaving the cervix. This could also be when your fallopian tubes and ovaries are removed at the same time. Since, you have a cervix, you will still need Pap smears.
Total Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes and ovaries. This will start menopause immediately after the surgery.
Radical Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes, ovaries, the upper portion of your vagina, and some surrounding tissue and lymph nodes. This is done to people with cancer. Patients who get this enter menopause right after the surgery.
Lorna Luxe's Husband John Dies After Three Year Long Cancer Battle

Credits: Instagram
Lorna Luxe's Husband, 64, John Andrews passed away after a three-year-long cancer battle. On February 11, the British influencer shared a post on her Instagram. The 43-year-old wrote: "My beautiful, brave John died yesterday. I am heartbroken. We were together to the every end, at home, in our own bed and holding hands which is exactly what he wanted."
Lorna Luxe's Husband John Dies: What Happened To Him?
John, a former banker, was diagnosed with stage three cancer in 2023. He had been receiving treatment over the last three years. John's cancer also entered remission and it returned in 2024 and spread to his brain.
He underwent a surgery in 2025, however, he was back in hospital in December after a complication with his chemotherapy treatments. This led to organ failure.
In January this year, Lorna told her followers that she was "looking for a miracle" and shared that his cancer had "progressed to his other organs" and treatment was "no longer an option".
“I think he's possibly the bravest person. And I suppose at this point we're looking for a bit of a miracle and we're going to take each day as it comes,” she wrote on her post.
In her post that announced John's death, she wrote when she asked him how he was feeling, her husband responded, "Rough, but in love".
Read: Catherine O'Hara Cause Of Death Is Pulmonary Embolism; She Also Had Rectal Cancer
Lorna Luxe's Husband John Dies: Can Cancer Spread To Other Organs?
While John's cancer has not been specified, but the reports reveal that his cancer spread to other organs. According to National Institution of Health (NIH), US, the spreading of cancer to other parts of the body is called metastasis.
This happens when cancer cells break away from where they first formed, and travel through the blood or lymph system. This could lead to formation of new tumors in other parts of the body. Cancer can spread to anywhere in the body, however, it is common for cancer to move into your bones, liver, or lungs.
When these new tumors are found, they are made of the same cells from the original tumor. Which means, if someone has lung cancer and it spread to brain, the cells do not look like brain cancer. This means that the cancer cells in the brain is metastatic lung cancer.
Cancer cells could also be sent to lab to know the origin of the cell. Knowing the type of cancer helps in better treatment plan.
Lorna Luxe's Husband John Dies: Could Chemotherapy Lead To Organ Damage?
As per the University of Rochester Medical Center, in some cases, chemotherapy could cause permanent changes or damage to the heart, lungs, nerves, kidneys, and reproductive organs or other organs.
For instance, some anti-cancer drugs cause bladder irritation, it could result in temporary or permanent damage to kidneys or bladder. In other cases, chemotherapy could also have potential effects on nerves and muscles. Chemotherapy could also damage the chromosomes in the sperm, which could also lead to birth defects. In females, it could damage the ovaries and could result in short-term or long-term fertility issues.
Chemotherapy could also induce menopause before the correct age and could cause symptoms like hot flashes, dry vaginal tissues, sweating, and more.
For some, it could also cause a 'chemo-brain', which is a mental fog that many chemotherapy patients face, that could affect memory or concentration.
© 2024 Bennett, Coleman & Company Limited

