- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Stress Is Affecting Different Parts Of Your Body, Know How
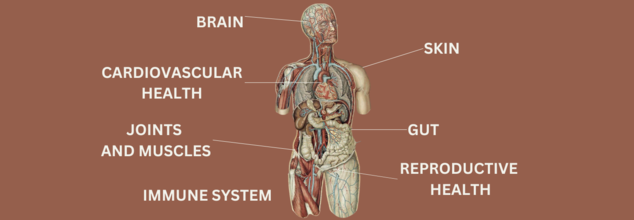
Although stress is a normal component of life, prolonged stress can have negative health repercussions. The infographic shows how extended stress impacts the body's systems, including the mental and physical health systems.
Let's examine the main ways that stress appears in each area of the body:
Mental and Brain Health
The brain is significantly impacted by stress. Cognitive function is among the first areas impacted, resulting in problems focussing and mental fog. High amounts of stress can also lead to mood fluctuations, anger, sadness, and anxiety. These symptoms have the potential to worsen over time and impact general mental health and wellbeing. This is a result of the brain's ongoing effort to adjust to stimuli, which strains its capacity for efficient operation.
Heart and Circulatory System
Stress has a particularly strong effect on the cardiovascular system. Extended periods of stress have been linked to elevated blood pressure, elevated cholesterol, and an increased risk of stroke or heart attack. Stress causes the body to release adrenaline and cortisol, two hormones that narrow blood vessels and increase heart rate. This can put stress on the heart over time and raise the possibility of major cardiovascular problems.
Skin-Related
Stress can also be shown in your skin. Physical symptoms include dull or dry skin, brittle nails, and hair loss. The body's capacity to recover itself can be slowed down by stress, which prolongs the healing process. Furthermore, because stress causes the body to generate more oil in reaction to hormonal fluctuations, disorders like acne can exacerbate under stress.
Stomach
Stress has a profound effect on the digestive system. It is the root cause of many digestive problems, including indigestion, constipation, diarrhoea and bloating. Malnutrition and other health issues may arise from a decline in the gut's capacity to absorb nutrients. Stress can worsen illnesses like irritable bowel syndrome (IBS) and cause more pain and discomfort in addition to these symptoms.
Muscles and Joints
One of the most obvious bodily indicators of stress is tense muscles. Inflammation and pain are frequently the results of this strain, especially in the back, shoulders, and neck. Stress-related muscle tension can eventually lead to decreased flexibility, an increased risk of injury, and chronic pain issues.
Immune System
Because stress impairs immunity, the body is more vulnerable to diseases and infections. It shortens the duration of healing and lessens the potency of immunological responses. This is because long-term stress inhibits the immune system's ability to produce cells that aid the body in warding off infections. Furthermore, the body's capacity for self-healing is hampered, which delays the healing process following an illness or injury.
Reproductive System
Stress can have a direct effect on reproductive health in both men and women. Stress can worsen premenstrual syndrome (PMS) symptoms in women and lead to irregular menstrual cycles. It also has an impact on hormone production, which may cause libido to decline. Stress can impact sperm production, testosterone levels, and sexual function in males.
Why Every Indian Over 30 Needs Kidney Screening Tests

Credit: Pinterest
While once considered an old-age disease, experts are now seeing kidney damage in people in their 30s and 40s. The prevalence of CKD in India has jumped significantly, moving from about 11 percent from 2011-17 to over 16 percent from 2018-23 among those aged 15 and above.
Kidneys are remarkably efficient that they can lose a vast majority of their function without causing any pain or noticeable symptoms. By the time physical warning signs such as foot swelling or fatigue appear, the underlying damage has already reached an advanced stage.
What Factors Are Contributing To Kidney Damage In Younger People
- Obesity: Obesity causes kidney disease by forcing the kidneys to overwork (hyperfiltration) to meet the metabolic demands of increased body mass, leading to structural damage. In addition, excess fat causes chronic inflammation, high blood pressure, and insulin resistance, which together damage kidney filters (glomeruli), resulting in protein leakage (albuminuria) and progressive scarring.
- Diabetes And Hypertension: Diabetes damages small blood vessels, causing hypertension (high blood pressure). High blood pressure then accelerate damages to the kidneys' filtering units, called glomeruli, which further worsens blood pressure and kidney function.
- Smoking: It damages the kidneys by constricting blood vessels, reducing blood flow, raising blood pressure, and introducing toxins like cadmium, causing or worsening diabetes-related kidney disease.
- High Salt Intake: Excess salt (sodium) is harmful to the kidneys because it causes the body to retain water, raising blood pressure, which damages the delicate filtering vessels in the kidneys and increases the risk of chronic kidney disease. Contaminated Water Dehydration: Contaminated water has heavy metals such as lead, arsenic, cadmium, and agrochemicals that directly damage renal tubules of the kidneys. Furthermore, they also trigger chronic inflammation and oxidative stress.
Why Early Screening is Important
- Asymptomatic Nature: CKD often shows no symptoms until the kidneys are severely damaged. Screening (eGFR and urine ACR tests) is the only way to detect early damage.
- Preventive Action And Delayed Progression: Early identification enables managing high-risk factors such as blood pressure and blood sugar, which stops or slows down the progression to kidney failure.
- Reduced Complications & Mortality: Early intervention is associated with a 48 percent drop in major cardiovascular events, reducing the high mortality rate associated with renal dysfunction.
- Cost Management And Quality of Life: Detecting CKD early reduces the burden of disease, allowing patients to avoid dialysis or transplantation and preventing catastrophic medical costs.
- High-Risk Target Groups: Individuals with hypertension, diabetes, obesity, or a family history of kidney disease need to be screened annually to prevent progression
Screenings Options
To catch issues early, the article recommends three standard tests:
- Serum Creatinine: A serum creatinine blood test measures the level of a waste product from muscle metabolism to evaluate kidney function. Healthy kidneys filter creatinine; thus, elevated levels often indicate kidney dysfunction, chronic disease, or acute failure. Normal ranges are typically 0.7–1.3 mg/dL for men and 0.6–1.1 mg/dL for women.
- eGFR (Estimated Glomerular Filtration Rate): Estimated Glomerular Filtration Rate (eGFR) is a blood test that measures how well the kidneys filter waste from the blood, indicating the level of kidney function. A result of 90 or higher is generally normal, while consistently low levels (below 60 for 3+ months) indicate chronic kidney disease or potential failure.
- Urine Albumin Test: The test detects early-stage kidney disease (albuminuria/proteinuria) before significant symptoms appear, allowing for earlier intervention to prevent further kidney damage.
Prevention
- Hydration
- Controlling blood sugar/pressure,
- Maintaining a healthy weight
- No to self-medication
- Control Salt Intake
- Balanced diet:
Experts Reveal The Everyday Habits Ruining Your Kidney Function | World Kidney Day

Credit: Canva
As people across the globe observe World Kidney Day, experts are sounding the alarm over the dangerous everyday habits that are worsening your kidney function and paving the way for the development of chronic conditions.
Dr Neha Bhandari, Senior Consultant, Pediatric Nephrology, Aakash Healthcare exclusively tells Healthandme: "Kidneys are very crucial in ensuring that the body maintains its internal equilibrium by filtering wastes, fluid regulation, electrolytes regulation, and in the process of assisting in blood pressure regulation as well.
"Nevertheless, a number of general living habits that have developed as part of contemporary everyday activity such as high painkiller use, large intake of processed foods and progressively sedentary lifestyles have the potential of slowly damaging the kidney functions. Since the damage of the kidneys frequently happens without any symptoms, and has no symptoms in severe cases, such simple habits can become a serious problem in the long-term, without any treatment."
Dr A K Jayaraj, MBBS, MS (Gen Surgery), MCH (Urology) at Apollo Spectra Hospital, Chennai also told this publication: "From the painkillers people take to relieve pain to the food they eat and the lifestyle they lead, there are a number of factors that can affect the functioning of these small but powerful organs.
"Focusing on these three factors helps keep these internal filters running smoothly by supporting clear blood flow, steady blood pressure, and balanced energy levels."
Here are the habits you need to keep an eye out for to protect your kidneys:
1. The Hidden Danger of Pain Killers
Dr Jayaraj warns that readily-available painkillers meant for headaches and other pains can cause serious damage to the kidneys. He said: "Most individuals have painkillers in their medicine cabinets, ready to be used whenever headaches or muscle aches occur. Painkillers are dangerous to the kidneys, especially when their use is frequent in the long run."Pain killers, such as non-steroidal anti-inflammatory drugs (NSAIDs), are known to constrict the blood vessels that lead to the kidneys. Constricted blood vessels limit the ability of the kidneys to filter blood, and frequent use of painkillers in the long run may lead to scarring or chronic diseases in the kidneys. It is always better to use the lowest
dose possible and look for other alternatives to pain killers, such as physical therapy, bed rest or heat packs."
Moreover, Dr Bhandari added: "In the long run, the continuous intake of these kinds of medicines can cause long-term kidney damage to the person, particularly those who are already predisposed to other conditions like diabetes, high blood pressure, and dehydration or people who already have kidney disease. Overdosing with painkillers may also cause a situation called analgesic nephropathy which involves progressive renal damage and functional weakness of the kidney as a result of constant exposure to the drugs."
2. The Burden of Processed Foods
Multiple studies show that ultra processed foods (UPFs) can be harmful to the heart, brain, liver and overall wellbeing. However, experts also warn that consuming UPFs can be extremely dangerous for kidney health and can cause long-term damage."What a person eats directly affects how hard their kidneys have to work. Modern processed foods are often a "triple threat" because of their high levels of salt, sugar, and chemical additives.
- "High Salt: Processed meats and canned goods are packed with sodium, which raises blood pressure. Since kidneys are filled with delicate blood vessels, high pressure can wear them out quickly.
- "Preservatives: Many packaged snack foods contain preservatives, which are chemicals used to extend the shelf life of the food product. These chemicals are much more difficult for the kidneys to flush out of the system than natural minerals, leading to a buildup of toxins in the blood. Fresh fruits, vegetables, and grains are much better for the kidneys, as they do not contain preservatives," Dr Jayaraj said.
3. The Importance of Fitness
While doctors around the world note that having an active lifestyle can do wonders for both mental and physical health, Dr Bhandari highlights the dangers of not incorporating a workout in your routine.
She tells Healthandme: "Lack of exercise leads to weight gain, poor metabolic health, insulin resistance, and blood pressure all of which are great risk factors of kidney disease. The immobility also impacts circulation and general cardiovascular health, which in turn indirectly impacts on the effectiveness of the kidney functionality needs as adequate blood flow is needed to make the kidney processes effectively.
"Those who work long hours sitting with little physical activity during the time can gradually be a contributor to the disease conditions, which increases the damage to kidneys without thinking of the side effects of the disease in the long term.
"Indirect contribution can also be made by hydration habits. Most people replaced water with sweet drinks or caffeinated ones or soft drinks, which may lead to metabolic disorders and an overload of the kidney. Proper filtration and aiding in the excretion of toxins and metabolic waste into the body is facilitated by the adequate water intake."
"Weight gain and high blood sugar are the primary causes of kidney failure. Daily exercise, such as a 30-minute walk every day, helps the body regulate blood sugar well and maintain healthy blood pressure at all times. This, in turn, does not overwork the kidneys and allows them to perform at optimal capacity," Dr Jayaraj advised.
The Early Warning Signs of Chronic Kidney Disease You Shouldn't Ignore

Credit: Pintrest
Often referred as a "silent killer," Chronic Kidney Disease (CKD) is a progressive and irreversible condition where the kidneys gradually lose their ability to filter waste and excess fluids from the blood. When the kidneys fail, waste builds up to high levels in your blood, potentially leading to complications like heart disease or stroke.
Recent data from The Lancet and the Global Burden of Disease study reveals that out of nearly 14 crore Indians living with CKD, nearly 40 percent of diabetic patients and 40 percent of those with long-standing hypertension are at risk of developing CKD.
As CKD frequently shows no symptoms until nearly 90 percent of kidney function is already gone, Dr. Visweswar Reddy, Senior Consultant in Nephrology at SRM Prime Hospital, shares early signs everyone should look out for.
Early Signs Of Chronic Kidney Disease
He noted that one of the biggest challenges with kidney disease is that symptoms often appear very late said “Unfortunately, most of these symptoms appear only when more than 90 per cent of kidney function has already been lost.”
- Frothy Urine: Foamy urine refers to urine that appears bubbly or frothy in the toilet bowl indicating high concentrations of protein (proteinuria) from kidney stress.
- Frequent Urination: Rapid urination (or increased frequency/nocturia) is important in kidney disease because it often signals that the kidney's filters are damaged and cannot properly concentrate urine. This dysfunction causes the body to produce more dilute urine, requiring more frequent elimination to remove toxins and manage fluid balance.
- Swollen Feet: Swollen feet (edema) are an early indicator of kidney disease, occurring when damaged kidneys fail to remove excess fluid and sodium from the body. This fluid accumulates in tissues, causing swelling in the ankles, feet, legs, and sometimes the face. Early detection is crucial to prevent further kidney damage
- Loss of appetite and Vomiting: Both loss of appetite (anorexia) and vomiting are common symptoms in kidney disease, affecting 30–50 percent of dialysis patients. It is caused by the buildup of waste products (uremia), toxins, fatigue and cytokines, key drivers of chronic inflammation and fibrosis in both acute and chronic kidney diseases
Importance of early screening
- Irreversibility: As it causes permanent damage detecting it early is the only way to stop or slow down the progression before it reaches total kidney failure.
- Avoiding Dialysis: Timely medical care in the initial stages can preserve enough kidney function to prevent a patient from ever needing dialysis or a kidney transplant.
- Managing High-Risk Links: Since nearly 40% of diabetic patients and 40% of those with long-standing hypertension are at risk of developing CKD, screening allows doctors to catch the damage long before it becomes life-threatening.
Screening Option For Early Detection
Dr. Reddy emphasizes that you don't need complex procedures to check your kidney health. He suggests three basic investigations that provide a clear picture of how the organs are performing:- Serum Creatinine Blood Test: A serum creatinine blood test measures the level of waste product from muscle metabolism to evaluate kidney function. Healthy kidneys filter creatinine; thus, elevated levels often indicate kidney dysfunction, chronic disease, or acute failure. Normal ranges are typically 0.7–1.3 mg/dL for men and 0.6–1.1 mg/dL for women.
- Urine Examination: Urinalysis for kidney function evaluates urine for signs of damage, primarily checking for protein (albumin), blood, and waste products like creatinine to assess filtering capability.
- Blood Sugar Test: He said even a small blood test can be used to monitor for diabetes, which is the leading cause of kidney disease in India.
Who Is At Most Risk
- Individuals with Diabetes: Diabetes is the leading cause of chronic kidney disease, affecting roughly one in three adults with diabetes. High blood sugar damages the small blood vessels and filters (nephrons) in the kidneys over time, causing them to leak protein into urine and lose the ability to filter waste, which can eventually lead to kidney failur
- Those with Hypertension (High Blood Pressure): High blood pressure and kidney disease share a two-way relationship, acting as both cause and effect. Uncontrolled high blood pressure damages delicate kidney blood vessels, leading to chronic kidney disease. Conversely, damaged kidneys cannot regulate blood pressure, which causes hypertension to worsen.
- Family History: Family health is closely linked to kidney disease primarily through shared genetics, hereditary conditions, and shared environmental factors like diet and lifestyle. Having a first-degree relative (parent, sibling) with chronic kidney disease (CKD) or kidney failure significantly increases a person's risk.
- Adults Over 18 with Risk Factors: Even younger adults should be screened if they have any of the underlying conditions mentioned above.
© 2024 Bennett, Coleman & Company Limited

