- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
THIS Test Reveals If You Are Watching 'Too Much' Porn

THIS Test Reveals If You Are Watching 'Too Much' Porn
Pornography has become a pervasive aspect of modern culture, widely consumed across all demographics. Digital media platforms have made accessing adult content easier than ever. The statistics show the unimaginable consumption rates - the largest adult entertainment website, Pornhub, said it had served over 4.6 billion hours of porn in 2016. While many people might use pornography for entertainment or education, the ready availability suggests overuse and addiction.
When viewing habits increase, they may interfere with personal relationships, work commitments, and even mental health, thus making it essential to analyze whether one's consumption is getting into problematic territory.
Porn addiction or Problematic Pornography Use (PPU), is a situation where an individual cannot help but watch pornography despite knowing that it is interfering with their life. Unlike casual use, addiction involves compulsive behaviors that cause harm to the physical and mental well-being. PPU over time leads to conditions like erectile dysfunction, heightened anxiety, depression, and withdrawal symptoms. However, some researchers argue that moderate consumption doesn't inherently cause harm. The challenge lies in identifying the tipping point where usage becomes excessive and detrimental.
Test To Know If You Are Watching 'Too Much' Porn
International psychologists had to realize the necessity of clarity and developed what is known as the Problematic Pornography Consumption Scale, a pioneering tool with which individuals can determine unhealthy habits. This 18-question assessment offers a scientific framework for behavior evaluation that has 98% diagnostic accuracy for PPU, and it looks into the six core elements of problematic pornography use:
1. Salience
This relates to the centrality of pornography in an individual's life. Does it really dominate their thoughts and emotions to the extent that one feels its effects on one's daily life?
2. Mood Modication
This assesses if the porn users utilize the medium in the process of mood control-arousal, relief, or escape from distress.
3. Conflict
This factor examines both internal and external conflicts. Internally, a person may recognize their habits are harmful but feel powerless to change. Externally, it assesses whether pornography use causes friction in relationships or interferes with responsibilities.
4. Tolerance
Over time, users may need to consume more explicit content or increase viewing time to achieve the same emotional effect, signaling a dependency.
5. Relapse
This captures repeated failed attempts to reduce or quit pornography use despite a desire to stop.
6. Withdrawal
Quitters may experience withdrawal symptoms, which can include headaches, irritability, or even nausea.
The increase in PPU follows the increasing accessibility of the internet worldwide. The UK has ranked as the second largest consumer of online pornography with 16.6 million monthly searches. Studies show nine of ten adults have viewed pornography, while two-thirds of young people often view adult content. Notably, many individuals experience pornography at a relatively tender age; by 13, half of these children have already seen it in online platforms. Experts reveal that young people are a bit more vulnerable, given some spend up to 12 hours a week accessing pornography.
Research shows that around 10% of adults have experienced some level of PPU, and more among younger populations. It is observed that men have a more problematic consumption than women but it affects both men and women and all orientations.
Health Consequences of Porn Addiction
PPU is detrimental to health. It can lead to a variety of physical and psychological issues, among which are:
Erectile Dysfunction (ED)
This is because porn use, over time, makes sex in real life less rewarding.Mental Health Issues
High levels of anxiety, depression, and even emotional sensitivity are characteristic.Withdrawal Symptoms
Even like drug or gambling addicts, those trying to give up pornography can feel chilliness, headaches, nausea, and insomnia.Cognitive Impairments
Complaints of "brain fog," inability to focus, and feelings of increased loneliness or restlessness in abstinence are common.Science Behind the Test
The Problematic Pornography Consumption Scale is the fruit of collaboration between experts such as researchers from Nottingham Trent University. After surveying hundreds of users, they were able to come up with a very fine questionnaire that probed into the six dimensions of PPU. Preliminary results indicate that around 4% of the participants fall under the "at risk" category while many others have moderate tendencies.
The study findings indicate the urgent need for addressing PPU as an emerging health issue. More research into the onset and nature of withdrawal symptoms and more in-depth psychological and social consequences of excessive pornography use are in the call of experts.
Watching Porn and Relationships
This influence of PPU is not just at an individual level. It can disrupt intimate relationships, break trust, and create unrealistic expectations about what intimacy is. In workplaces, this excessive consumption of pornography could cause a decrease in productivity, even leading to job loss. As society becomes increasingly dependent on digital platforms, the distinction between healthy use and addiction becomes increasingly ambiguous.
Moreover, early exposure to pornography among youth poses significant risks. Considering a quarter of 16 to 21-year-olds encountering porn during primary school, there is a greater need for education and prevention strategies than ever.
Determine for yourself if your pornography use is a problem by starting with personal reflection. The Problematic Pornography Consumption Scale can be a scientifically validated guide for you to understand your behaviors and their impact on you. Moderate consumption is certainly not harmful, but realizing signs of addiction is helpful in keeping mental, emotional, and relational health well-balanced. If your usage has affected your well-being, seek professional help to re-assert control.
World Misophonia Awareness Day 2025: When Everyday Sounds Feel Like An Attack—Here’s What Misophonia Is

Credits: Health and me
You're at the dinner table and someone slurps soup, another begins tapping a pen, and your heart begins racing, your muscles lock up, and you're filled with fury you can't explain. If this sounds familiar, you're not being "too sensitive." You may be one of millions dealing with misophonia, a little-understood sensory disorder finally receiving long-overdue notice.
On July 9, World Misophonia Awareness Day, experts and advocacy groups are urging for global recognition of this condition that impacts almost 1 in 5 adults, but too often remains misunderstood or undiagnosed. Initiated by non-profit soQuiet, the day is dedicated to advancing discussion, research, and support for those whose lives are deeply affected by what the rest of us tune out—usual, ordinary sounds.
What Is Misophonia?
Misophonia, literally "sound hatred," is more than not liking noise. It's an intense, automatic emotional and physical response to certain sounds, usually created by someone else. Chew, sniffle, heavy breathing, throat clearing, even pen clicking.
These stimuli trigger strong reactions in individuals with misophonia, from annoyance, stress, and revulsion to outright panic or fury. For some, it's a single stimulus. For others, it's multiple. The psychological weight can be overwhelming, so that everyday encounters such as dining at a restaurant or working in an open office become a daily war.
And though most people write it off as being irritable or melodramatic, the science disagrees.
An increasing amount of research is revealing what's actually going on in the brains of individuals with misophonia. A 2022 study published in Frontiers in Neuroscience indicates that misophonia is potentially associated with a specific "neural signature"—unique brain pathways that are more active in perceiving sound and emotion.
In misophonics, increased interconnectivity between the sound-processing auditory cortex and the emotion-regulating limbic system may be what makes some sounds ring alarm bells. It's a brain in overdrive, responding in the same way to a throat clear or chewing noise as it would to a bodily threat.
A reflexive fight-or-flight response—hands sweat, heart throbs, and logical thinking yields to a frantic need to flee or strike out.
Why Misophonia Is Unheard And Misunderstood?
Perhaps one of the most infuriating things for people with misophonia is that others just don't get it. It doesn't help that they are invisible and their reactions are usually termed overreactions, even rudeness.
Worse still, it has the potential to overlap with or be confused with other mental illnesses such as OCD, anxiety, PTSD, or even autism spectrum disorders. That is why diagnosis becomes complicated and many suffer silently, particularly older people who might have spent decades without ever hearing the term "misophonia."
The stigma may result in isolation, strain on relationships, and depression, particularly when individuals are stuck in environments where they cannot escape to be safe from trigger sounds—such as school, work, or home mealtime.
Misophonia is not just about being uncomfortable—it's about survivability. Most with the condition report avoiding parties, leaving jobs, or having trouble with day-to-day activities just to prevent exposure to triggers. Picture wearing noise-canceling headphones just to get through your workplace. Or having every meal in solitude, because even the sound of eating is too much. In a world that's getting noisier, adaptation is a full-time profession.
How Misophonia Affects the Brain?
Misophonia's not so much about what you're hearing—it's about how your brain interprets that sound. New research indicates that individuals with misophonia exhibit heightened activity and connectivity within brain areas that handle sound processing, emotional control, and the body's defense mechanism.
One of the most important regions engaged is the anterior insular cortex, which assists you in assessing the emotional meaning of sensory input. In misophonia, this region seems to hyperreact, sending messages that something harmless—such as someone chewing—is threatening. This activates the limbic system, which controls emotion and survival reactions, placing the individual in a fight-or-flight state very quickly.
Imagine it like a smoke alarm blaring at burnt toast like it is a raging house fire. That exaggeration is what makes misophonia so debilitating. A person with misophonia has a complete body stress response when they hear a trigger sound, even though rationally, they know the sound is not harmful.
Brain imaging studies suggest this is not about overreacting by choice—it’s a neurological mismatch, where emotional and auditory systems are too tightly wired together. That’s why even brief exposure to trigger sounds can feel unbearable and linger long after the sound stops.
Common Trigger Sounds of Misophonia
Misophonia triggers are different for different people but most follow predictable patterns. They're not loud or startling noises—they're typically repetitive, mundane sounds easily tuned out by other people but for the misophonic person, which can trigger an almost immediate adrenaline rush of anger, panic, or disgust. The following are the most typical categories of trigger sounds:
Drinking and eating noises: Smacking lips, slurping, chewing, gulping, crunching, and loud swallowing are the worst. Chewing gum is a very frequent offender.
Sounds associated with breathing: Sniffling, heavy breathing, nose blowing, or snoring are common culprits. Even a faint wheeze can be offending for some.
Sounds of the mouth and throat: Throat clearing, coughing, yawning, or audible kissing sounds.
Repetitive sounds of activity: Tapping on the pen or feet, mouse clicking, typing, drumming fingers, or even paper or plastic bag rustling.
Environmental and ambient sounds: Ticking clock, ringing telephone, dripping water, or sounds of animals such as barking.
Surprisingly, several individuals comment on how the proximity or origin of the noise is important. A TV chewing noise might be mildly annoying—but if it's coming from someone sitting directly next to them, the response can be volcanic. This serves to illustrate that misophonia is not about the sound type or volume but also relationship, context, and physical proximity.
Knowing these triggers can inform treatment and coping mechanisms, particularly when seeing therapists and learning to recognize patterns and decrease emotional reactivity over time.
Is Misphonia Treatable?
Misophonia is finally being studied, understood, and treated. Cognitive Behavioral Therapy (CBT) is showing promising results. A 2020 study published in Depression and Anxiety found that more than a third of patients undergoing CBT saw a meaningful reduction in misophonia symptoms—and these improvements held up a year later.
CBT involves finding individual noise triggers and reframing the emotional response to them. It's training the brain to break the anxiety or anger spiral, not allow it to get the best of you. In extreme cases, therapy is also paired with anti-anxiety medication to decrease reactivity, particularly when CBT alone doesn't work. Other coping strategies are:
- Wearing noise-canceling headphones
- Using white noise machines or soothing background music Deep breathing or muscle relaxation exercises
But most importantly, others' awareness and knowledge is the strongest support of all.
Why is Family and Social Support Important?
For individuals with misophonia, having family members know what the condition is and what it's like makes a huge difference. Family members tend to unwittingly become trigger points—chewing at the dinner table, throat clearing, playing music out loud.
Dismissal and blame only exacerbate the emotional toll. Specialists maintain that education and compassion are essential. Accepting that the response is involuntary—and not a personal affront—is critical. Offering professional assistance and using supportive measures in the home can assist in creating safe, respectful spaces for those affected.
World Misophonia Awareness Day isn't only for patients—it's for everyone. By recognizing that some sensory stimuli can be triggering, offices, schools, and public places can start to make changes that are inclusive.
Misophonia isn't a trait, it's a real, life-changing condition that's worthy of attention and understanding. As the research expands and the stories get out there, we get closer to a world where individuals with misophonia don't merely exist—but thrive.
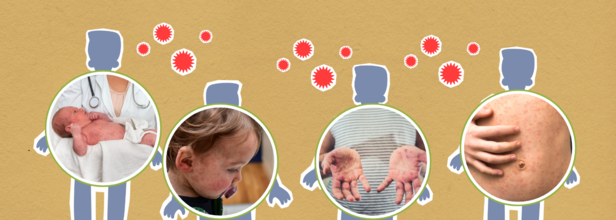
Even After The Elimination Of Measles In 2000, Why Is US Struggling With It Today?
Credits: Canva
The United States is facing its worst measles outbreak in 25 years, with more than 1,270 confirmed cases reported so far this year—surpassing the previous high of 1,274 cases in 2019. The data, compiled by Johns Hopkins University, has raised alarms among health officials, who believe the actual number of infections may be even higher due to underreporting.
Tragically, three people have died from the virus this year—two children in Texas and one adult in New Mexico. All of them were unvaccinated.
“This move will further fuel the spread of vaccine-preventable illnesses,” said Dr. Bruce A. Scott, president of the American Medical Association, referencing ongoing declines in vaccination rates and policy shifts that threaten public health.
From Elimination to Outbreak
Measles is one of the most contagious diseases known and was declared eliminated in the United States in 2000, thanks to the widespread use of the MMR (measles, mumps, rubella) vaccine. However, current outbreaks suggest a reversal of that progress.
The largest outbreak this year began in January in Gaines County, West Texas—a region with one of the lowest vaccination rates in the state. So far, that outbreak alone has led to over 750 confirmed cases and has spread to neighboring areas in New Mexico and Oklahoma, with possible links to Kansas.
Shockingly, nearly one in four kindergartners in Gaines County did not receive their required MMR vaccine during the 2024–25 school year.
Spread Through Travel and Everyday Contact
Measles spreads easily through airborne droplets when an infected person coughs, sneezes, or talks. The virus can also live on surfaces like doorknobs for several hours, making it especially hard to contain.
Air travel has further complicated containment efforts. In Colorado, an out-of-state visitor unknowingly spread the virus while contagious, leading to multiple cases—including individuals who were only at the airport at the same time.
According to the CDC, nearly 1 in 8 people infected this year required hospitalization, and about 30% of all cases have been in children under the age of five. Most of these children were unvaccinated.
The Role of Vaccination
The MMR vaccine remains the most effective tool against measles. One dose offers 93% protection, while two doses provide 97% protection.
In response to the crisis, some states have taken emergency steps to protect infants. Several have lowered the age for the first MMR shot from 12 months to 6 months. The results have been encouraging—early vaccination rates among 6-month-olds in Texas are now eight times higher than in 2019.
New Mexico has also seen a significant rise in vaccination, and both states are working hard to protect their most vulnerable populations.
Still, nationwide vaccination rates remain below targets. The U.S. aims for 95% of kindergartners to receive both doses of the MMR vaccine, but this benchmark has been missed for the past four years. In the 2023–24 school year alone, over 125,000 kindergartners lacked at least one required vaccine.
A Shifting Public Health Landscape
Public health experts are concerned that growing distrust in vaccines and leadership changes at the federal level may further undermine efforts to control the disease.
As of now, the CDC does not have a permanent director in place, and U.S. Health and Human Services Secretary Robert F. Kennedy Jr.—a long-time vaccine skeptic—has made controversial decisions. Though he recently expressed support for vaccines, his previous statements and the removal of key expert panels have left public health officials worried.
If outbreaks linked to the Texas region continue into 2026, the U.S. risks losing its measles elimination status. Experts say rebuilding public trust in vaccines and boosting routine childhood immunizations must become a national priority—before the disease becomes even harder to contain.
Does Seasonal Shift Mess With Digestion? Here’s How To Keep Your Gut Healthy

Credits: Canva
From crisp winters to hot summer and humid rains, each season brings unique joys—and unexpected shifts in our gut health. If you’ve ever found yourself bloated in the summer, constipated in the winter, or randomly battling stomach bugs during monsoon season, you’re not alone. Turns out, your digestive system is just as sensitive to seasonal changes as your skin or mood.
The gut, which contains trillions of bacteria (the gut microbiome), does more than break down food. It maintains immunity, modulates hormones, and even "talks" to the brain. But it's not bulletproof. Temperature, humidity, sunlight, changes in diet, and lifestyle variations throughout the seasons can upend this sensitive balance. Here's how seasons affect your gut—and what you can really do to maintain its equilibrium throughout the year.
Dr. Manoj Kutteri, Ayurvedic wellness expert explains, "Seasonal transitions deeply influence our body’s internal balance, especially gut health. According to Ayurveda, our jatharagni or digestive fire fluctuates with the seasons, impacting how we digest and absorb nutrients. Understanding and adapting to these natural rhythms through seasonal diets can prevent digestive issues and boost overall health."
Why Your Gut Feels the Weather?
1. Shifts in Diet = Shifts in Microbiome
Winter foods are heavy, rich, and warming—really, creamy soups, meat, and baked goods come to mind. Summer, on the other hand, gravitates towards raw salads, chilled smoothies, and hydrating fruits. These changes directly influence the population and diversity of your gut bacteria. A summer diet high in fiber increases good bacteria, whereas high sugar or fat in winter might feed bad bacteria.
2. The Weather Influences Digestion
Severe summer heat can delay digestion and make one more dehydrated, with symptoms such as bloating and fatigue. Cold temperatures, conversely, can decrease fluid consumption and bring about constipation with reduced activity levels.
3. Physical Activity
Warmer weather usually translates to more activity—hiking, swimming, walking—which stimulates digestion. But once winter arrives, many get sedentary. Less activity translates to slower gut motility, and that's where digestive problems begin to accumulate.
4. Mood and Mental Health
Fewer sun rays and shorter days during winter are associated with Seasonal Affective Disorder (SAD), which raises anxiety and stress—two of the biggest factors for gut diseases such as IBS. That "gut feeling" is not just figurative.
5. Immune System and Infections
Fall and winter seasons are usually associated with a peak in viral infections. Some of these, such as stomach flu, are direct attacks on your gut. Even respiratory infections can affect gut bacteria, particularly if antibiotics are prescribed.
Gut Survival Guide for Season-Specific Tips That Work
Dr Kutteri says, "In summer, the digestive fire tends to weaken due to external heat. The body craves more hydration and lighter foods. Eating heavy, oily meals can burden digestion, causing bloating, acidity, or sluggishness. To maintain gut balance, include hydrating foods like cucumbers, melons, coconut water, mint, and fresh buttermilk. Fermented foods and natural probiotics like curd, kanji, and pickled vegetables support gut flora and enhance gut and overall immunity. It’s also essential to stay well-hydrated with clean, filtered water or mild herbal infusions to aid digestion and prevent heat-related gut disturbances."
Spring: Cleanse & Reset Naturally
This is the ideal time to rejuvenate your gut after a rich winter diet. Supplement with seasonal greens such as spinach, asparagus, and peas—high in prebiotic fiber. They feed good gut bacteria and promote natural detoxification.
Summer: Hydration is Digestion's Best Friend
Heat and perspiration cause fluid loss. Dehydration thickens stool and slows down digestion. Drink water regularly during the day. Add hydrating foods such as cucumbers, watermelon, and berries. Eat raw salads sparingly; they may irritate an upset gut.
During monsoons, digestive strength remains low, and the risk of waterborne infections increases and to this Dr Kutteri shares, "This season demands careful food hygiene. Avoid street food, non-seasonal produce, and raw salads. Drink boiled, cooled water to reduce microbial load. Simple fasting or light meals help reset the gut when symptoms like diarrhoea or indigestion arise. Spices like ginger, black pepper, Tulsi, Turmeric and asafoetida support digestion and reduce bloating."
Autumn: Warmth and Spice for Gut Comfort
Begin moving toward cooked, warming foods. Add seasonal vegetables such as pumpkin, carrots, and beets. Spices such as ginger, cinnamon, and turmeric enhance digestion and anti-inflammation. Bone broths and mild spiced lentil soups make excellent winter staples.
Winter: Battle Constipation and Build Immunity
Increase your intake of vitamin C-rich citrus fruits, fatty fish for vitamin D, and fermented foods like kimchi and yogurt to support gut flora. Don’t skip meals and ensure you’re getting enough fiber to offset the natural slowdown in digestion.
"Winter, on the other hand, enhances jatharagni or digestive fire, allowing for the digestion of heavier foods. This is the time to nourish the body with warm, grounding meals rich in good fats, proteins, whole grains, root vegetables, ghee, and seasonal fruits like amla, lemon and guava. Herbal decoctions and warming spices (like cinnamon, cloves, and Tulsi) strengthen respiratory and gut immunity," Dr Kutteri further adds.
Why Seasonal Gut Issues Worsen?
Across all seasons, timely eating, respecting hunger cues, and consuming locally grown, seasonal foods help the body stay aligned with nature. Our ancient wisdom teaches that food is not just fuel, but medicine. Eating with awareness of the seasons ensures optimal digestion, absorption, and a healthy gut.
Waterborne Infections Rise With Temperature Swings
Weather changes may affect municipal water quality. Bacterial or parasitic infections peak during seasonal change. Stay with filtered or bottled water, particularly when traveling.
Food Hygiene Is a Year-round Risk
Street food, undercooked meats, and inadequately refrigerated sauces such as mayonnaise are fertile grounds for dangerous bacteria. Eat home-prepared meals, especially during heat or humidity.
Cravings for Raw Food Can Be Risky
That fresh summer salad might seem cool, but uncooked vegetables and condiments such as sandwich spreads can harbor germs if not cleaned well. Wash fruits extensively and shun street corner juices.
Home Is Where the Health Is
Homemade meals and hot meals minimize exposure to bacteria. Heating food to high temperatures exterminates germs, and scrubbing fruits under running or boiled water eliminates residual contaminants.
Don't Forget the Gut-Immune Connection
A robust immune system is your gut's strongest protection when the seasons change. Back it up with regular sleep, everyday activity, and an eating plan high in zinc, magnesium, vitamin C, and antioxidants. Probiotic foods such as kefir, sauerkraut, and miso restore bacterial equilibrium.
If digestion feels awry during a weather transition, don't dismiss it as stress or travel. Many times, it's your gut attempting to adjust to an environmental change without the assistance it requires.
Seasonal variations totally interfere with your digestion—but you can beat them to the punch. Prioritize foods that are gut-friendly, drink plenty of water, beware of hygiene traps, and keep movement and stress in check during all four seasons. Your gut likes routine and attention even when the weather is far from predictable.
Dr. Manoj Kutteri is a Ayurvedic and wellness expert, Medical Director & CEO, Atmantan Wellness Centre
© 2024 Bennett, Coleman & Company Limited

