- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Trachoma Is Finally Eliminated From India
As per the World Health Organisation (WHO), trachoma is a disease of the eye caused by infection with the bacterium Chlamydia trachomatis. It is a public health problem in 38 countries and is responsible for the blindness or visual impairment of about 1.9 million people.
Good News For India
On October 8, the WHO validated India as having eliminated trachoma as a public health problem. "India’s elimination of trachoma as a public health problem is a testimony to the country’s commitment to alleviating the suffering that millions have faced from this debilitating disease,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “WHO has worked closely with India to realize this achievement, and we congratulate the government, health workers and partners who have collaborated to make it possible.”
India has finally joined Nepal and Myanmar in the WHO South-East Asia Region along with 19 other countries that have defeated this disease. Though trachoma is preventable, the blindness caused by this is irreversible and it continues to be a public health problem in 39 countries.
History Of India's Fight Against Trachoma
The Ministry of Health and Family Welfare initiated a trachoma control project which was supported by the WHO and UNICEF. This aimed at community-based interventions to eliminate trachoma. By 2005, trachoma was responsible for 4% of cases of blindness in India and by 2018, the prevalence went down to 0.0008%. A series of impact, pre-validation and trichiasis-only surveys were completed in 2025 and confirmed the elimination of the disease from the nation. This dossier was also reviewed by a Regional Dossier Review Group and upon its recommendation the WHO validated the national elimination of trachoma as a public health problem in India.
How Can It Spread?
It can spread from person to person through contaminated fingers, fomites and flies that could come into contact with discharge from the eyes or nose of an infected person. Environmental risks like poor hygiene, overcrowded households, and inadequate access to water and sanitation facilities can also lead to trachoma.
Who All Are Trachoma Free?
Among the 19 countries validated by WHO as trachoma-free are:
- Benin
- Cambodia
- China
- Gambia
- Ghana
- Iran
- Iraq
- Lao
- Malawi
- Mali
- Mexico
- Morocco
- Myanmar
- Nepal
- Oman
- Pakistan
- Saudi Arabia
- Togo
- Vanuatu
A Routine Sinus Rinse With Tap Water Led To Woman's Death After Brain-Eating Amoeba Infection

Credits: Health and me
A Texas woman of 71 died tragically from a brain infection caused by Naegleria fowleri, commonly referred to as the brain-eating amoeba. The source? A simple sinus rinse using tap water from her RV's potable water system. The woman, as a recent Centers for Disease Control and Prevention (CDC) case report indicates, suffered severe neurological disease shortly after nasal irrigation. She died within eight days of symptom onset.
This incident, although uncommon, has brought with it renewed international debate regarding water safety, sound nasal hygiene habits, and the life-altering risks of ignoring water sterilization protocols.
The case, who was reported to be healthy before the accident, had utilized the tap water from her RV's faucet to fill a nasal irrigation device—frequently employed to alleviate sinus pressure or allergic conditions. Four days thereafter, she showed symptoms of sudden onset of fever, severe headaches, and confusion. Her illness rapidly progressed to seizures and changes in mental status. She died eight days from the onset of symptoms despite immediate medical treatment.
Laboratory examinations diagnosed the Naegleria fowleri in her cerebrospinal fluid—a diagnosis with a mortality rate of more than 97%.
What Is The Brain-Eating Amoeba?
Naegleria fowleri is an amoeba which is free-living and microscopic and occurs naturally in warm freshwater bodies like rivers, lakes, and hot springs, as well as in soil. The organism usually infects humans when contaminated water enters the body via the nostrils—most often during swimming or rinsing of the nasal passages.
After entering the nasal passages, the amoeba moves into the brain through the olfactory nerve and results in Primary Amebic Meningoencephalitis (PAM), a rare and lethal infection of the brain. The infection is not spread by drinking contaminated water, nor is it passed between people.
While very uncommon, PAM is nearly always fatal. As of the CDC, out of 157 U.S. cases from 1962 to 2022, only four individuals have survived.
Risk of Using Tap Water for Nasal Rinses
The CDC's inquiry into the Texas case discovered that the woman had done sinus rinses several times with tap water from the RV's potable water tank. The tank, it turns out, had been refilled three months earlier—prior to the purchase of the RV—and had probably contained stagnant, contaminated water. Moreover, the RV's municipal water system that provided the RV could also have contributed to the contamination.
These results point out an important safety issue: tap water—even considered "potable"—is not necessarily safe for direct nasal application. It may harbor trace amounts of organisms that, when breathed into the nose, lead to serious infections.
Early Warning Signs Of PAM
The symptoms of PAM usually start between one to 12 days after exposure, and the majority of cases develop quickly. Early warning signs are:
- Fever
- Headache
- Nausea or vomiting
- Stiff neck
- Altered mental status
As the disease progresses, signs of neurological impairment like confusion, hallucinations, seizures, and coma ensue. Alas, too often the rapid development of the illness leaves scant opportunity for effective action.
Since early manifestations of PAM are so similar to those of bacterial meningitis, the CDC recommends that individuals—particularly those who have recently been in contact with warm freshwater or have used nasal irrigation—to consult a physician at once if the following symptoms occur.
How to Safely Perform Nasal Irrigation?
Nasal irrigation is a well-known and beneficial technique for easing sinus pressure and controlling allergies. It is only safe if done with water that has no microbial contaminants. According to the CDC, only the following should be used for sinus irrigation:
- Distilled or sterile water
- Boiled tap water (boiled for 3–5 minutes and cooled)
- Water filtered through a filter with an absolute pore size of 1 micron or smaller
- Items such as neti pots, bulb syringes, and sinus rinse bottles need to be properly cleaned after every use and completely air-dried.
This instance serves as a grim reminder that the ease of omitting the use of water treatment can result in deadly consequences, particularly for non-traditional water systems such as those found in RVs, which potentially go without strong maintenance or sterilization.
The disaster also points to weaknesses in water systems—especially in non-traditional dwelling places like RV parks, where drinking water systems may not be subject to the same level of review as urban systems. Lack of maintenance or management of such systems can lead to the introduction of unusual but lethal pathogens into daily life.
In addition, the changing climate might be making the population more vulnerable. While global temperatures are increasing, Naegleria fowleri is moving its habitat into regions not previously thought to be too cold, thus posing new public health threats. Summer season, characterized by warmer water bodies and higher recreational activity, is now particularly dangerous for exposure.
After diagnosis, treatment of PAM includes aggressive administration of antifungal and antibiotics such as amphotericin B, rifampin, azithromycin, and miltefosine—a newer antiparasite found to be effective in a few survivors. With immediate medical treatment, nonetheless, survival is still very low because the amoeba kills brain tissue so quickly.
Early diagnosis is essential but notoriously challenging because initial care is nonspecific and the condition develops at an alarming rate.
Why Does Stretching Sometimes Cause Painful Cramps?

(Credit-Canva)
Have you ever felt a sudden, sharp pain when you stretch? It can be really uncomfortable, whether you're stretching in the morning, during the day, or at night. Muscle cramps are a common occurrence, not just for athletes, but also for others. Sometimes it can be just as simple as stretching your legs or arms, that causes you to have sudden and sharp pain.
So why do these things happen? And how does one prevent this discomfort from taking place? A doctor named Doctor Sood, a Board-Certified MD, practicing Germantown, MD office, who shares health tips on TikTok, explained why this happens. That painful feeling is actually a muscle spasm.
Common Reasons for Muscle Cramps
These involuntary muscle tightening can be quite intense. While they often go away on their own, understanding why they happen can help you prevent them. Doctor Sood points out several common reasons for these muscle spasms.
- Not drinking enough water (dehydration)
- Using your muscles too much
- Tired muscles
- Poor blood flow
- Pinched nerves
- Lack of important minerals like magnesium, calcium, or potassium
When you don't have enough of these minerals, your muscles can't hold onto fluids properly, which makes you more likely to get cramps.
When to Be Concerned About Cramps
While muscle cramps are often harmless and caused by simple things like dehydration or tired muscles, it's really important to pay attention if they become frequent, unusually painful, or seem out of the ordinary for you. In some less common situations, persistent muscle spasms can actually be a clue that your body is experiencing a more serious underlying health problem.
Therefore, if you notice that you're getting cramps very often, or if they're particularly severe, accompanied by other unusual symptoms, or simply don't resolve with typical remedies like stretching and hydration, it's a very good idea to consult with your doctor.
Treating and Preventing Muscle Cramps
To really get rid of cramps, the best thing is to find out why they're happening. This might mean a visit to your doctor to understand the main reason. If you're in pain, you could try a pain reliever like ibuprofen, but always talk to your doctor first before taking any medicine.
Drink plenty of fluids
Make sure to drink lots of water and sports drinks all day long. These help your body get back the fluids and important minerals, like electrolytes, that your muscles need to work properly. Staying hydrated is key to avoiding cramps.
Use heat
Putting heat on the cramped area can really help. A hot shower, a warm bath, or a heating pad can relax tight muscles, get your blood flowing better, and ease the discomfort. This makes your muscles less likely to cramp when you stretch.
Stretch softly
If you feel a cramp, keep stretching gently and slowly. This gentle movement can help the muscle spasm go away by slowly making the muscle longer. Doing regular, gentle stretches also makes your muscles more flexible and improves blood flow, which helps stop future cramps during your day.
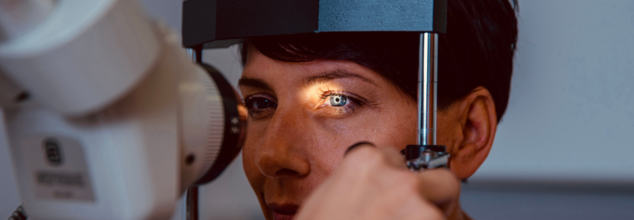
First Sign Of Diabetes Might Show Up In Your Eyes—Here’s What To Look For

Credits: Freepik
Diabetes is known for its impact on blood sugar but one of the first and often overlooked warning signs may appear right in front of your eyes—literally. Changes in vision might be the first sign that there is something amiss, even ahead of the official diagnosis of diabetes.
The Centers for Disease Control and Prevention (CDC) reports that an estimated 30.3 million adults in the United States have diabetes, and nearly 90% of them have Type 2 diabetes—a condition in which your body becomes resistant to insulin and has difficulty regulating normal blood sugar levels. While the disease is usually linked to complications such as neuropathy or kidney disease, your eyes may be the first organ to exhibit signs of suffering.
The eye is a sensitive organ covered in a close network of blood vessels, particularly in the retina—the thin layer of tissue at the back of your eye that facilitates vision. High blood sugar levels over time can hurt these small blood vessels, making them become inflamed, leaky, or clogged. That's called diabetic retinopathy, and it's one of the first—and possibly most destructive—complications of diabetes.
Over one-third of working-age population with diabetes already have signs of diabetic eye disease, and it is still a major cause of blindness among this group. Many are also unaware they have it—until their eyesight is already compromised.
What is Diabetic Retinopathy?
Diabetic retinopathy often progresses painlessly and without any signs, at least in its early stages. That's why regular eye exams are so important—despite your vision appearing completely normal.
If left uncontrolled, diabetic retinopathy may result in impaired or even complete vision loss. Worse, the damage tends to be permanent. Early detection and therapy can slow or even prevent progression, but the secret is to be vigilant and preventive.
Early Warning Signs of Diabetes In Your Eyes You Can't Ignore
Floaters
Tiny specks, cobwebs, or worm-like forms floating in your line of sight are usually harmless. But a sudden proliferation of floaters—particularly if there's blurred or obscured vision—may indicate bleeding into the retina, a symptom of diabetic retinopathy.
Dark Spots
Any dimming of vision or blind spots, especially in the central visual field, are warning signs. These "blockages of vision" can indicate swelling of the retina or hemorrhaging—and need to be seen by an ophthalmologist right away.
Blurred Vision
Changes in blood sugar levels can disrupt your eye's ability to focus, causing fleeting or ongoing blurring. This can make it harder to read, drive, or identify faces and can continue to get worse if left unchecked.
Vision Loss or Shadows
Partial blindness, i.e., reduced peripheral vision or inability to see in dim light, can be a sign of advanced retinopathy or retinal detachment. Vision can even black out for a short time—a warning of extreme vascular damage.
If you have any of these symptoms, even if you don't have diabetes, it is important to consult an eye care professional immediately.
What Causes Diabetic Eye Damage?
Diabetic retinopathy occurs when high blood glucose levels start damaging the tiny blood vessels of the retina—the light-sensitive nerve tissue at the back of the eye. The vessels can become clogged, leak fluid or blood, or cause new and fragile, abnormal vessels to grow through a process known as neovascularization. This cascade can result in swelling, inflammation, scarring, and, eventually, retinal and optic nerve damage. In bad cases, the retina can come loose or fluid will pool in the macula (the retina's center portion), producing a condition called macular edema. These issues can lead to permanent loss of vision if left untreated.
Even though any diabetic is susceptible to developing diabetic retinopathy, there are some populations that are particularly at risk. These include those with Type 1 and Type 2 diabetes, especially those with poorly managed blood glucose levels. Pregnant women who develop gestational diabetes and individuals who have had diabetes for longer than five to ten years have a higher risk of retinal complications. Those with coexisting conditions like high blood pressure or elevated cholesterol are at even greater risk, as these issues can accelerate the damage to blood vessels in the eyes. Research indicates that up to 75% of people with Type 1 diabetes will develop some form of retinopathy, while approximately 50% of individuals with Type 2 diabetes show signs—often within the first decade following diagnosis.
Can Diabetic Retinopathy Be Cured?
Regrettably, diabetic retinopathy has no cure. The condition can be prevented from worsening if intervention is made early. Thanks to the advancements in medical technology, a number of treatment avenues can be employed. Anti-VEGF injections are usually used to prevent abnormal vessels from growing on the retina. Laser therapy is also an effective method that involves destroying leaking vessels and preventing vision loss. In more serious instances, vitrectomy surgery might be necessary to eliminate scarring tissue or blood within the eye. Most importantly, the most important thing is to control diabetes properly—adhering to healthy blood sugar levels, blood pressure, and cholesterol can go a long way in preventing serious eye complications in the long run.
Protect Your Vision with These 3 Non-Negotiable Steps
If you’ve noticed floaters, blurriness, or dark spots, don’t dismiss them. These could be more than visual annoyances—they might be early cries for help from your body. Although it's clear that preventive care, lifestyle changes, and monitoring are your best weapons against diabetes-related blindness.
1. Prioritize Lifestyle Interventions
Exercise, proper diet, and weight control are important. Include low-impact activity such as walking, yoga, or swimming. Follow a diet with high fiber, antioxidants, and whole grains and reduce saturated fats and refined carbohydrates.
2. Monitor Blood Sugar and A1C Levels
Regular blood sugar checks and routine monitoring of A1C levels (which measure average glucose over three months) can help you detect and correct abnormal trends. Aim for an A1C below 7%, or as recommended by your healthcare provider.
3. Don’t Skip Eye Exams
Your diabetes care regimen should include a dilated eye exam once a year. These tests alone can detect early signs of diabetic retinopathy. More frequent examinations may be warranted if risks or symptoms rise.
Your vision is not simply a measure of how well you see—it's literally a window to your overall health. In some cases, eye problems might be the first sign that you have diabetes. That's why receiving regular eye exams—even in the absence of obvious symptoms—is a key component of preventive care.
© 2024 Bennett, Coleman & Company Limited

