- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
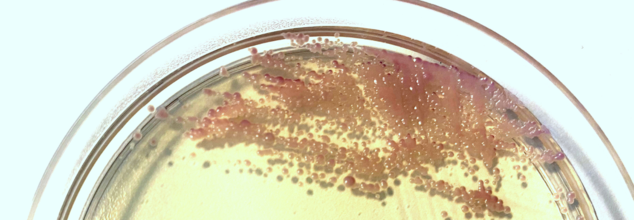
UK Reports A Subtle Surge In Yeast Infections: Report
Credits: Canva
New figures from the UK Health Security Agency (UKHSA) show that bloodstream infections caused by yeast continue to be a growing concern. In 2024, these infections increased by 4% compared to 2023, rising from 2,170 to 2,247 cases. This translates to an infection rate of 3.9 per 100,000 people across England, up from 3.8 the previous year.
How Yeast Enters the Bloodstream
Bloodstream infections caused by yeast often occur in hospital settings. These infections are typically linked to yeasts naturally present on our skin or in the gut. When patients receive prolonged courses of broad-spectrum antibiotics, their normal bacterial flora is suppressed, allowing yeasts to grow unchecked. In some cases, these yeasts can cross the gut wall and enter the bloodstream. Individuals with weakened immune systems—such as cancer patients or those using invasive medical devices—are particularly vulnerable.
Most Common Yeast Species Behind Infections
The leading cause of yeast bloodstream infections remains Candida albicans, followed by Nakaseomyces glabratus (formerly Candida glabrata) and Candida parapsilosis. Interestingly, N. glabratus infections were most common among the elderly, while C. albicans and C. parapsilosis infections were more frequent in children.
Infection Rates Higher in Deprived Areas
The UKHSA report highlights a concerning disparity in infection rates across socioeconomic groups. In 2024, people living in the most deprived parts of the country experienced higher rates of bloodstream yeast infections (5.0 per 100,000) compared to those in the least deprived areas (3.2 per 100,000). UKHSA is currently working with healthcare partners to better understand these differences.
The Rise of Drug-Resistant Candidozyma auris
While resistance to antifungal drugs overall has remained stable, the rise of Candidozyma auris (previously Candida auris) is raising alarm. This drug-resistant fungus has emerged as a significant global health threat. Between 2013 and 2024, England recorded 637 cases of C. auris, with 178 of them reported in 2024 alone. Most notably, cases surged following the end of COVID-related travel restrictions.
To support healthcare providers, UKHSA has issued updated guidance for managing C. auris outbreaks. The fungus is now a notifiable disease, meaning all confirmed cases must be reported to public health authorities.
Ongoing Surveillance and the Need for Vigilance
Professor Andy Borman, Head of the Mycology Reference Laboratory at UKHSA, emphasized the growing impact of serious fungal infections on public health. He noted that increasing numbers of immunocompromised patients and complex medical treatments may be contributing to the rise.
Although antifungal drugs remain effective for now, that could change if resistance grows. “The rise of drug-resistant C. auris in hospitals means we must remain vigilant,” said Borman, stressing the importance of infection control and improved surveillance.
Unlike bacterial infections, fungal infections did not decline during the pandemic, likely due to overwhelmed hospital systems and complications from severe COVID-19. As infection rates continue to climb, rapid diagnostics and better tools for managing these infections remain a public health priority.
One Head Injury Could Be Enough to Trigger Brain Cancer, Shocking Study Finds

(Credit-Canva)
Head injuries are always treated as the top priorities in hospitals and emergency situations. Why? Simply because even the smallest injuries you can be the cause of big consequences. We may not realize it but due to the sensitive nature of our heads, the quietest impacts also leave big marks, and a new study showed that these marks could, in fact, be tumors.
This research, published in JAMA Network Open, comes from a team at Mass General Brigham. They wanted to see if there was a connection between having a traumatic brain injury (TBI) and later developing a malignant brain tumor. To do this, they looked at health data from over 75,000 adults who had a TBI and compared it to a similar group of people who didn't. They carefully removed data from anyone who already had risk factors for tumors, like a history of cancer or exposure to radiation, to make sure their findings were as clear as possible.
What Is Malignant Brain Tumor?
According to the NHS, A malignant brain tumor is a fast-growing cancer that can spread to other parts of the brain and spine. Tumors are typically given a grade from 1 to 4, which indicates how quickly they grow and their likelihood of returning after treatment. Malignant tumors are classified as Grade 3 or 4, while benign, or non-cancerous, tumors are usually Grade 1 or 2.
Most malignant brain tumors are secondary cancers, meaning they originated in another part of the body and then spread to the brain. In contrast, primary brain tumors begin in the brain itself.
How Do Head Injuries Lead To Brain Cancer?
The study found that people who had a moderate to severe TBI were more likely to develop a malignant brain tumor. Specifically, within three to five years after their injury, 0.6% of those with a moderate or severe TBI developed a brain tumor, which was a higher percentage than the control group. Interestingly, the study found no increased risk for people who had a mild TBI, such as a concussion. This suggests that the severity of the head injury plays a crucial role.
Dr. Saef Izzy, one of the lead researchers, described the results as "alarming." He explained that this study adds to a growing body of evidence showing that TBI isn't just a short-term problem; it can have lasting effects on a person's health. The finding that TBI might be linked to brain tumors adds urgency to the idea that TBI patients need long-term medical monitoring. He also mentioned that this new finding, combined with their previous research linking TBI to heart disease, underscores the importance of lifelong care for those who've suffered a brain injury.
What Are Some Signs and Symptoms Malignant Brain Tumor?
The signs of a malignant brain tumor depend on its size and location in the brain. Common symptoms include:
- Severe, ongoing headaches
- Seizures or fits
- Constant nausea, vomiting, and feeling drowsy
- Changes in personality, memory, or behavior
- Vision or speech problems, or growing weakness or paralysis on one side of the body
Why People Should Be More Careful With Head Injuries
The researchers were careful to state that their study found an association, not a direct cause-and-effect relationship. The aim was to open the door for more research. Dr. Sandro Marini, another lead author, noted that while the overall risk of developing a tumor after TBI is still low, this discovery means doctors should monitor TBI patients more closely. The team hopes that future studies will explore the biological reasons behind this link and see if the location of the brain injury is related to where a tumor develops. They also want to study patients who have had multiple head injuries, like from repeated falls.
Why the Inches on Your Neck Are More Dangerous Than Your Waistline?

Credits: Canva
When most people think about weight and health risks, the waistline is the focus. Doctors and researchers often measure body mass index (BMI) or waist-to-hip ratios to estimate whether someone is at risk of conditions like heart disease or diabetes. However, growing body of research indicates a different, often neglected measurement- neck size.
It might come as a shock, but neck size could provide an important insight into your risk for severe health conditions such as heart disease, diabetes, and sleep disturbances. And the part that might raise an eyebrow: even individuals with a healthy BMI are not in the clear. A thicker neck can be dangerous even in those who otherwise appear to be fit and healthy.
Neck size has nothing to do with appearance or clothing fit. Neck size is a reflection of fat distribution in the upper body. Upper-body fat is metabolically active; it releases fatty acids, hormones, and inflammatory factors into the blood more easily than fat elsewhere on the body, such as the hips and thighs.
When such substances overwhelm the system, they upset cholesterol equilibrium, increase insulin resistance, clog blood vessels, and ignite long-term inflammation. Eventually, that chain reaction elevates the risk for several conditions, ranging from cardiovascular disease to type 2 diabetes.
In a sense, neck size serves as a proxy for visceral fat—the unhealthy type that encircles inner organs and speeds up cellular aging.
What Is The Link Between Neck Size And Diseases?
Clinical evidence highlights just how potent this relationship is. Studies reveal that individuals who have thicker necks have a higher chance of developing:
Cardiovascular diseases like hypertension, atrial fibrillation (irregular heart rhythm), and even heart failure. Atrial fibrillation is especially worrying as it raises the risk of stroke and may ultimately lead to heart failure.
Coronary heart disease, where constricted arteries decrease the supply of oxygen-containing blood to the heart.
Type 2 and gestational diabetes, both associated with insulin resistance caused by upper-body fat.
Obstructive sleep apnea, a sleep disorder in which the airway repeatedly collapses, cutting off breathing. This disorder not only induces fatigue but also stresses the cardiovascular system.
The connection is so strong that more and more physicians now add neck size to sleep apnea assessments.
A 2022 study went further, linking a bigger neck to an elevated risk of erectile dysfunction in men, continuing to add another layer to the unseen risks of too much upper-body fat.
What Qualifies as a Risky and Dangerous Neck Size?
Scientists have found thresholds where risks become much higher:
- For men, a 17-inch (43 cm) or larger neck circumference.
- For women, 14 inches (35.5 cm) or larger.
What's surprising is that such risks continue even among individuals with normal BMI or healthy weight. And for each extra centimeter above these thresholds, research indicates increasing hospitalizations and deaths.
This implies you may be "healthy" on paper in terms of BMI, yet your neck circumference may tell a different tale.
Sleep, Stress, and Metabolic Strain
The implications of a thick neck go beyond the development of chronic disease. Obstructive sleep apnea is a perfect case in point. Individuals with larger necks have a higher risk of airway collapse when they sleep, resulting in broken sleep, dips in oxygen, and extreme exhaustion during the day. This then increases risks for accidents, cardiovascular stress, and poorer quality of life.
Aside from apnea, degraded quality sleep exacerbates metabolic control. If the body doesn't receive restorative sleep, blood sugar management, hormone function, and appetite take a hit—propelling the vicious cycle of weight gain and risk of disease.
Neck Size and the Obesity Epidemic
The significance of neck circumference is exacerbated by the trends in obesity in the modern world. In America, close to 2 out of every 5 adults and 1 out of every 5 children are obese, based on the Centers for Disease Control and Prevention. Scholars observe that though the risk factor is in neck circumference across populations, it is most specifically relevant for individuals already with a history of living with obesity.
This makes it a potentially potent agent for determining people most at risk, more than BMI or waistline alone can indicate.
Measuring your neck circumference can be done in less than one minute. With a tape measure, place it around the thinnest area of your neck so that it is snug but not constricting.
If the measurement is over the thresholds, it's not a reason for alarm, but it's a good idea to take it seriously. Neck circumference is just a piece of the health puzzle, but it can be an early warning sign—one you have control over.
What Can You Do To Reduce Neck Circumference?
Yes, your neck size can change. Targeted lifestyle changes can lower fat stored in the upper body, including the neck. Here's how:
- Cardiovascular activity such as walking, swimming, or cycling burns fat and lessens total adiposity.
- Strength training builds muscle and enhances a higher rate of metabolism, making it simpler to maintain fat off in the long run.
- Optimal sleep regulates hormones associated with appetite and fat storage.
- Well-balanced nutrition—prioritizing whole grains, vegetables, fruits, pulses, lean protein, and healthy fats—maintains metabolic health without surplus calories.
The secret is consistency. Regular healthy habits over time shrink visceral fat, which can then lower neck circumference and reduce the risk of associated health issues.
Medical professionals warn against substituting neck circumference for a complete medical evaluation, but it can be used as a simple, underutilized measurement to accompany BMI and waistline checks. For others, it could be the initial indicator that triggers further examination.
Social Connection Isn’t Just Fun: How Socializing Could Literally Add Years To Your Life?

Credits: iStock
Food, water, and oxygen are the obvious essentials for survival but to truly thrive, our brains demand something else: human connection. Social interaction is not a luxury, it is as vital to our wellbeing as exercise or sleep. Whether it’s a quick chat with a neighbor, a phone call with a friend, or a day spent volunteering, the evidence is piling up that socializing does more than lift our spirits. It may actually help us live longer.
A new study published in the Journal of the American Geriatrics Society found that older adults who stay socially active are significantly more likely to live longer compared to those who are socially isolated. That single finding adds weight to decades of research showing that connection is one of the strongest predictors of healthy aging.
Are Humans Wired for Social Connection?
Unlike solitary animals, humans evolved as pack creatures. Our survival has always depended on working together, relying on one another for food, safety, and support. Even in modern life, this wiring hasn’t changed. Whether you thrive in large groups or prefer just a handful of close relationships, your brain still needs meaningful social contact.
Neuroscientists have discovered that interacting with others activates brain regions that remain dormant when we’re alone. These regions are linked to empathy, judgment, and communication. Without stimulation, they weaken over time, contributing to cognitive decline. Research shows that consistent socialization can slow the onset of dementia and preserve memory function. In contrast, chronic isolation can shrink brain volume and accelerate mental decline.
The recent U.S. study followed more than 2,200 adults aged 60 and older. Researchers collected lifestyle data, psychosocial assessments, and blood samples, then tracked the participants for four years. The results were striking: those with high levels of social engagement were 42% less likely to die during that period than those with little or no engagement.
It wasn’t just any kind of interaction that mattered. Certain activities—like volunteering, caring for grandchildren, or joining sports clubs—had particularly strong links to longer life. These activities share a few traits: they provide purpose, involve movement, and encourage ongoing interaction with others.
Lead author Ashraf Abugroun of the University of California, San Francisco, put it plainly: “Staying socially active is more than a lifestyle choice. It is closely linked to healthier aging and longevity.”
What is The Biology Behind 'Socialising'?
Why does socializing influence longevity so strongly? Researchers point to two interconnected factors: biological aging and physical activity.
Social engagement appears to slow down markers of biological aging in the body. People who remain active in community or group settings often show healthier inflammatory profiles, better immune function, and improved cardiovascular health. At the same time, social life encourages movement—whether it’s walking with a friend, dancing at a community event, or gardening with neighbors. Physical activity itself reduces risk of chronic disease and extends lifespan, and social settings make that activity more consistent and enjoyable.
Benefits of Social Connection for Human Beings
The benefits aren’t only physical. Social activity is strongly tied to mental health. Research has consistently shown that loneliness increases the risk of depression, anxiety, and even suicide. On the other hand, maintaining friendships and close relationships boosts self-esteem, lowers stress hormones, and fosters resilience.
For example, group activities such as exercise classes or community clubs provide a natural buffer against daily stress. Conversations and shared experiences remind us we’re not alone in our challenges. A 2016 study in Psychology and Aging found that people who remain socially active into late life report higher satisfaction and happiness than those who withdraw. Happiness itself has been shown to improve health outcomes, creating a reinforcing cycle.
COVID-19 reminded us of the costs of isolation. Lockdowns cut people off from family, friends, coworkers, and community activities. Rates of depression and anxiety surged worldwide. For older adults especially, the sudden withdrawal of social contact proved damaging. Even virtual connection, while better than none, couldn’t replace the benefits of in-person interaction. The lesson was clear: social engagement isn’t optional for wellbeing—it’s essential.
Are Social Needs Same For Everyone?
Not everyone needs the same amount of socializing to feel fulfilled. Extroverts may thrive on daily interaction with large groups, while introverts may prefer only a few hours with close companions. What matters most is not the number of interactions but their quality and consistency. Both groups—introverted and extroverted require some level of social contact to maintain cognitive and emotional health.
Even solitary-seeming activities often include subtle forms of social connection. Watching TV shows or movies involves empathizing with characters. Browsing social media sparks feelings of comparison, judgment, or admiration—all forms of social processing in the brain. Humans are constantly scanning and responding to other humans, whether in person or virtually.
How to Stay Social at Any Age?
For older adults, socializing may take intentional effort. Retirement, loss of loved ones, or health issues can reduce opportunities for connection. But small changes make a big difference. Scheduling regular calls with family, joining local clubs, volunteering, or simply sharing meals with neighbors can reintroduce the richness of human interaction. For younger adults, staying connected is equally important for long-term brain health and resilience.
Even if mobility or geography make in-person gatherings difficult, technology can help. Video chats, online group activities, and community forums provide meaningful interaction. But experts agree that whenever possible, face-to-face connection has the strongest impact.
Think of social activity as preventive medicine. Just as you wouldn’t skip your daily walk or balanced meals, regular interaction should be built into your routine. It keeps the brain active, the body healthier, and the spirit lifted. For older adults in particular, it may even add years of life.
© 2024 Bennett, Coleman & Company Limited

