- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
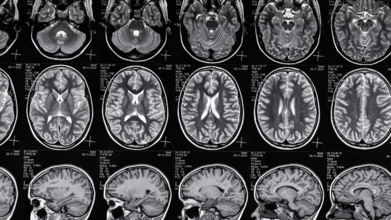
What Causes Epilepsy? 5 Common Reasons Why It Happens
Credits: Canva
Epilepsy affects millions of people worldwide, yet it remains one of the most misunderstood neurological conditions. The disorder is marked by recurring seizures, sudden bursts of electrical activity in the brain , which can cause symptoms ranging from brief confusion and muscle twitches to severe convulsions.
While anyone can have a single seizure for a variety of reasons, epilepsy is diagnosed when a person experiences two or more unprovoked seizures. Experts say understanding the causes can help with both prevention and treatment.
Genetics Can Play a Role
In some cases, epilepsy runs in families, pointing to a genetic connection. Certain gene mutations can disrupt normal brain activity, making seizures more likely.
Genetic epilepsy can be inherited, but the link isn’t always straightforward, says neurologists. Different genes affect the brain in different ways, and researchers are still uncovering exactly how these changes lead to seizures.
Even without a family history, spontaneous mutations in a person’s genes can also result in epilepsy.
Brain Damage Can Lead to Epilepsy
Any structural damage to the brain can disrupt its electrical signalling, triggering seizures over time. This damage might be recent or decades old.
Common structural causes include:
- Birth complications that reduce oxygen supply to the brain
- Head trauma from accidents or falls
- Brain tumors
- Stroke or bleeding in the brain
“Sometimes the injury happened years earlier, such as during birth, but its effects on brain function appear much later,” says Dr Gabriel Martz, MD, FAES, writing for Hartford HealthCare, who is a neurologist and director of the Ayer Neuroscience Institute Epilepsy Center.
Infections and Autoimmune Conditions Can Be Triggers
Infections that cause brain inflammation, such as meningitis or encephalitis, can have long-term consequences. Even after recovery, scarring and other changes in brain tissue can increase the risk of seizures.
In other cases, the immune system mistakenly attacks the brain, a condition known as autoimmune encephalitis, which can also lead to epilepsy.
“These causes highlight why protecting brain health through early diagnosis and treatment of infections is so important,” specialist notes.
4Sometimes, the Cause is Unknown
Despite advances in brain imaging and genetic testing, many people with epilepsy never learn the exact cause.
“We don’t always get a clear answer,” Dr Martz notes. “Not knowing the cause can be frustrating, but it doesn’t make the condition less real or less treatable.”
This uncertainty means that in some cases, treatment focuses entirely on managing seizures rather than addressing an underlying trigger.
Lifestyle and Environment Matter
While lifestyle alone doesn’t cause epilepsy, certain factors can raise the risk by increasing the chances of brain injury or neurological stress. These include:
- Substance misuse
- Dangerous sports without protective gear
- Repeated concussions
“Protecting your brain is one of the best ways to reduce preventable risk,” doctor says. Wearing helmets, avoiding risky behavior, and staying away from drugs can make a real difference.
When to Seek Medical Advice
If you or someone you know experiences a first-time seizure, it’s essential to consult a doctor. Tests such as an MRI, EEG, or bloodwork can help identify potential causes and guide treatment.
Epilepsy affects people in deeply personal ways, not only in how seizures manifest but also in how the condition impacts daily life and emotional well-being. Understanding what lies behind it is the first step toward effective care and fuller, healthier lives.
Pollution Could Be Slowly Eroding Your Cognitive Health: Study Shows Link Between Alzheimer's And Toxic Air Particles

(Credit-Canva)
A few years ago, we were being warned how air pollution may affect our lungs and make us weak. Now, we are facing this reality and much worse! High levels of air pollution may worsen Alzheimer's disease by speeding up the buildup of harmful proteins in the brain.
According to a new study, people with Alzheimer's disease who lived in areas with more air pollution had a greater buildup of these proteins and a faster decline in their thinking and memory skills.
The study, published in the JAMA Neurology from the Perelman School of Medicine at the University of Pennsylvania, showed that small toxins from pollution can damage our brain. The researchers explained that not only does this increase the risk of dementia, but it also makes Alzheimer’s worse. Could this mean pollution ages and damages our brain faster than our biological age? The researchers explored these question as well as how the small particles from pollution cause our brain health to deteriorate.
How Does Air Pollution Raise Risk Of Dementia?
For the first time, researchers studied brain tissue from people who had Alzheimer's. They found that those who lived in areas with higher levels of tiny air particles, even for just one year, had more severe buildup of amyloid plaques and tau tangles. These are two key signs of Alzheimer's in the brain. These individuals also experienced a quicker decline in their mental abilities, including memory loss, poor judgment, and difficulty with daily tasks.
"This study shows that air pollution doesn’t just increase the risk of dementia—it actually makes Alzheimer’s disease worse," said Dr. Edward Lee, a co-director of Penn's Institute on Aging.
What Are Harmful Pollution Particles Called?
Air pollution contains very small particles, often called fine particulate matter or PM2.5. These particles are less than 2.5 micrometers wide—about half the width of a single spider web strand. They come from things like car exhaust, factory smoke, and wildfires. Because they are so small, they can be inhaled and absorbed into the bloodstream, causing health problems. Past studies have already linked PM2.5 to memory loss and cognitive decline.
How Small Pollution Particles Affect Brain
Researchers looked at over 600 brain samples from a brain bank. By using satellite data and local air monitors, they were able to estimate the level of PM2.5 where each person lived. They found that for every small increase in PM2.5, the risk of more severe amyloid and tau buildup increased by 19 percent.
In addition, the study showed that those who lived in highly polluted areas and had more advanced brain damage also had more severe memory loss, speech difficulties, and poor judgment.
While this study focused on air pollution based on where people lived, researchers noted they couldn't account for other personal exposures, like secondhand smoke or exposure to chemicals at work.
According to Dr. Lee, "even just a year living in an area with high levels of pollution can have a big impact on a person’s risk for developing Alzheimer’s disease. It underscores the value of environmental justice efforts that focus on reducing air pollution to improve public health."
Severe Headaches Around Periods Are Not Normal: Neurologist Reveals Real Reason Behind A 35 Y/O Woman's Pain
Periods are different for all women. While some may experience mild pain and discomfort during their periods, others experience extreme pain and a myriad of symptoms. Sharing an instance of the same, in a recent post, Dr Sudhir Kumar, a Hyderabad-based Neurologist shared the story of a young woman struggling with debilitating pain, with real answer for it.
Anita, a 35-year-old school principal from Hyderabad, was full of energy and passion for her work. But for several months, two days a month became a nightmare. Like clockwork, right around her period, she would get terrible, throbbing headaches. These headaches were so bad they would often come with nausea and a strong dislike for light. On these days, it was hard for her to do anything, but she would still force herself to go to work with a fake smile.
At home, her family saw her pain. At school, her staff noticed she was pulling away. The headaches were slowly stealing her confidence at work and her happiness at home.
What Causes Headaches During Periods?
Anita first went to her family doctor and then to a women's health specialist. Some medicines helped for a short time, but they didn't stop the headaches from coming back every month. She was frustrated that no one seemed to understand what she was going through.
Finally, she came to see Dr Sudhir Kumar, a Hyderabad-based neurologist. In the post he explained that after listening carefully to her story the diagnosis was clear: Anita had menstrual migraines. These are headaches that are directly connected to the hormone changes that happen during a woman's menstrual cycle.
With the right treatment, Anita's migraines became less frequent and easier to manage. Her energy and vibrant personality returned. The school principal who once dreaded those two days of the month was now back to her confident self. When she last visited the clinic, she told her doctor, "You gave me my life back," expressing her relief and gratitude for finally being understood and effectively treated.
Why Do I Get Headaches Before Periods?
According to the Migraine Trust, a menstrual migraine is a type of migraine that's specifically linked to a woman's menstrual cycle. These migraines typically occur from about two days before a period begins to the third day of the period, but the timing can vary from person to person.
Menstrual migraines are very common. It's estimated that as many as two-thirds of women who experience migraines have attacks that are related to their periods. This condition can start when a woman first gets her period and can continue until menopause.
How Are Menstrual Migraine Different Than Regular Migraines?
Menstrual migraines often stand out from other types of migraines. They tend to be longer and more severe. Besides head pain, they're more likely to cause nausea, vomiting, and sensitivity to light or sound.
Also, these migraines usually happen without an aura, which is a visual disturbance or other symptom that can come before a migraine. They can also be harder to treat than migraines that occur at other times of the month.
Why Do Menstrual Migraines Happen?
The main reason for menstrual migraines is the link between migraines and hormones. A drop in the hormone estrogen is a well-known migraine trigger. As a woman's period approaches, her estrogen levels naturally fall, which increases the likelihood of a migraine attack.
Hormone-like substances called prostaglandins also play a role. The body releases more prostaglandins during a period, which can cause period cramps and also increase the risk of a migraine.
How To Recognize Menstrual Migraines?
A key factor in this condition is that to identify it no specific test exists. Doctors can't run a lab test to diagnose a menstrual migraine. The Migraine Trust reveals a few key points that can help you identify whether you have menstrual migraines.
Keep a diary to track symptoms
The most accurate way to check for a link is to keep a detailed diary for at least three months. In it, you should record both your migraine attacks and the dates of your menstrual period.
Look for a pattern
Menstrual migraines are defined as attacks that happen between two days before your period and the third day of your period. This pattern must occur during at least two out of three menstrual cycles.
Consult a doctor
Your doctor can review your diary and confirm if you have a menstrual migraine based on the timing and your symptoms.
Ozempic May Not Be Helpful If You Continue Emotional Eating: Study

(Credit-Canva)
Weight loss dependent on Ozempic has increased immensely, however, does Ozempic work for everyone? A new study showed that people who eat due to extreme emotions actually may not lose weight.
Ozempic and Wegovy are powerful drugs that can help people with diabetes manage their blood sugar and lose weight. But they don't work the same for everyone. A recent study from Japan sheds light on why, suggesting that how you eat, whether it's due to external triggers or emotional feelings, can affect how well these drugs work for you.
How Your Eating Habits Affect Weight Loss On Ozempic
Scientists in Japan followed 92 people with type 2 diabetes for a year after they started taking GLP-1 receptor agonists (like Ozempic). They wanted to see if a person's eating habits had any connection to the success of the treatment. They focused on three eating behaviors:
Emotional eating: Eating in response to feelings like sadness or stress, not because you're hungry.
External eating: Eating because of outside cues, like the sight or smell of delicious food, even if you're not hungry.
Restrained eating: Actively trying to control your diet to lose weight.
After a year, the study found that most people on the drugs lost weight and saw improvements in their body fat and cholesterol. However, when they looked at the different eating behaviors, they found some key differences.
How Do You Lose The Most Weight On Ozempic?
The study found that people who were prone to external eating at the start of the study had the best results in terms of weight loss and blood sugar control. The drugs seemed to be most effective for them over the long term.
On the other hand, the drugs were less effective for people who were prone to emotional eating. The researchers believe this is because emotional eating is tied to psychological factors that the medication doesn't directly address. This suggests that people who eat for emotional reasons might need extra support, like counseling, to see the best results from these drugs.
Dr. Daisuke Yabe, the study's senior author, noted that assessing a patient's eating behaviors before treatment could help doctors predict who will benefit most from these medications.
This was an observational study, which means it can't prove that eating habits directly cause the different outcomes. But the findings are promising and suggest a potential link. More research is needed, but if these results are confirmed in larger studies, doctors might one day use simple questions about eating habits to help personalize treatment plans for people taking drugs like Ozempic and Wegovy.
Which Diet Works Best For Ozempic
Your Diet plays a very important role in ensuring how much weight you will lose, even while taking medication like Ozempic. Here is how you maximize the benefits of the same according to American Association of Retired Persons (AARP,
Focus on Nutrient-Rich Foods
Because your appetite will be smaller, every bite counts. Choose whole, unprocessed foods like vegetables, fruits, and lean proteins. This is especially important for older adults who are more prone to vitamin deficiencies.
Don't Skip Meals
The medication can make it easy to forget to eat. To avoid feeling weak or losing muscle, try to schedule your meals or even set an alarm to remind yourself.
Make Protein a Priority
Protein is essential for keeping your muscles strong. Aim for at least 60 grams of protein a day, focusing on sources like chicken, fish, eggs, yogurt, and beans. A good tip is to eat your protein first at every meal.
Stay Hydrated
Drink at least 64 ounces of water or other fluids each day. This helps prevent dehydration and a common side effect: constipation. If you feel tired or get muscle cramps, you might need to add electrolytes to your water.
Avoid Fatty and Sugary Foods
Since the drugs slow down digestion, heavy, greasy foods like French fries and pizza can cause bloating, gas, and an upset stomach. It's also best to limit sugary foods and refined carbs (like white bread) as they can cause blood sugar spikes that make you feel tired and nauseous.
Eat Smaller, More Frequent Meals
Instead of three big meals, try eating smaller portions more often. This gives your body time to properly digest food and can help with nausea and heartburn.
Increase Your Fiber Intake
Constipation affects up to a third of users. To keep things regular, eat plenty of fiber-rich foods like fruits, vegetables, and beans. A fiber supplement can also help, especially in the beginning.
© 2024 Bennett, Coleman & Company Limited

