- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Is Adenomyosis? The Condition That's Often Mistaken For Endometriosis

Image Credits: Canva
Adenomyosis is a lesser-known but significantly debilitating gynecological disorder that is commonly mistaken for endometriosis. Commonly referred to as the 'evil twin sister' of endometriosis, adenomyosis occurs in millions of women across the globe and has symptoms such as intense pain and heavy menstrual bleeding, and also spells fertility issues. Though it is a common disorder, adenomyosis is underdiagnosed, and many women languish in silence. Knowing its causes, symptoms, and treatments can help increase awareness and provide timely medical care.
Adenomyosis is when endometrial cells—typically restricted to the lining of the uterus—break through the myometrium, the muscular wall of the uterus. In contrast to endometriosis, in which the same tissue develops outside the uterus, adenomyosis is inside the uterus but produces serious complications. These out-of-place endometrial cells continue to act as they would in a regular menstrual cycle, becoming thick and shedding, which leads to internal bleeding, inflammation, and intense pain.
How Common Is Adenomyosis?
Adenomyosis is more common than most individuals understand. Research indicates that as many as one in three women have the condition, although many of them are symptom-free or mistakenly attribute their symptoms to normal menstrual pain. Adenomyosis mostly occurs among women aged between 30s, 40s, and 50s, with the symptoms usually worsening as they draw closer to menopause.
Symptoms of Adenomyosis
The signs of adenomyosis are mild to severe and tend to overlap with the signs of endometriosis, which can make diagnosis complicated. The most frequent signs are:
Severe menstrual cramping: Women who have adenomyosis tend to have severe, debilitating pain that occurs during menstruation.
Heavy or prolonged menstrual bleeding: A lot of bleeding can cause anemia, fatigue, and weakness.
Pelvic pain and pressure: As the uterus expands as a result of the condition, it may create discomfort and bloating.
Painful intercourse: Dyspareunia (painful sex) is another quality-of-life-impacting distressing symptom.
Bleeding between menstrual periods: Some women have irregular spotting or bleeding outside of their menstrual period.
Adenomyosis and Fertility: Is There a Connection?
The relationship between adenomyosis and fertility continues to be the subject of research. Adenomyosis does not cause infertility, but it does provide an environment that is not conducive to implantation and pregnancy. The displaced endometrial tissue has the potential to cause irregular blood flow, persistent inflammation, and interference with normal uterine structure, all of which may complicate conception and successful pregnancy. In 2005, a study indicated that 79% of infertile women had both endometriosis and adenomyosis, reinforcing the possible role in reproductive illness.
Diagnosing Adenomyosis
Historically, adenomyosis could be diagnosed only microscopically from uterine tissue after a hysterectomy. Today, however, developments in imaging technologies have greatly enhanced early diagnosis. Doctors now can utilize:
Transvaginal ultrasound: An imaging test that is not invasive and may demonstrate uterine thickening and abnormal tissue growth.
MRI scans: Magnetic resonance imaging shows more detailed visualization of the uterus and is used to distinguish adenomyosis from related conditions such as fibroids or endometriosis.
Unfortunately, most women say that their symptoms are frequently dismissed or misdiagnosed because healthcare providers lack specialized knowledge. Increased awareness and better diagnostic methods are needed for early detection and proper management.
Treatment Options for Adenomyosis
No absolute cure for adenomyosis exists except for a hysterectomy, which involves the removal of the uterus. Nevertheless, several treatment options can alleviate symptoms and enhance quality of life. These include:
1. Pain Relief
Ibuprofen and naproxen, over-the-counter pain medications, are usually prescribed to relieve menstrual cramps and pain. Prescription pain medication may be required in more serious cases.
2. Hormonal Treatment
Birth control pills: Although effective in controlling periods and minimizing bleeding, birth control does not cure adenomyosis; it only suppresses symptoms.
Hormonal IUD (Intrauterine Device): The Mirena IUD, for example, releases progesterone to assist in lessening heavy bleeding and pain.
Progesterone therapy: High-dose progesterone treatments can help shrink endometrial tissue and lessen symptoms.
3. Lupron Injections (GnRH Agonists)
GnRH agonists, such as Lupron, induce temporary menopause by suppressing estrogen production, thereby reducing adenomyosis symptoms. However, these injections can cause severe side effects, including mood swings, hot flashes, and bone density loss, making them unsuitable for long-term use.
4. Surgical Intervention
Endometrial Ablation: This involves the removal of the uterine lining to manage heavy bleeding but is not a permanent solution and is not suitable for women who want to become pregnant.
Uterine Artery Embolization (UAE): A non-surgical procedure that cuts off blood supply to the affected areas, reducing the size of the adenomyotic tissue.
Hysterectomy: The only permanent solution for adenomyosis, a hysterectomy is usually considered as a last option for women who have finished their childbearing years.
Psychological Effects of Adenomyosis
Adenomyosis can have a physically and emotionally draining effect on a woman's life. Ongoing pain, tiredness, and excessive bleeding can affect daily activities greatly, triggering anxiety, depression, and decreased general well-being. Women with the condition tend to experience trouble in their workplaces, relationships, and social settings. Getting support from doctors, therapists, or support groups can help alleviate much-needed emotional comfort and coping skills.
Adenomyosis is still an under-talked-about and frequently misdiagnosed disorder, with many women not even knowing they are suffering. Greater education, better diagnostic techniques, and more treatment choices are needed to offer improved care. If you think you have adenomyosis, see a gynecologist to talk about symptoms, have appropriate diagnostic tests, and consider treatment. With the proper support and management, it is achievable to live a complete and pain-free life despite adenomyosis challenges.
Is Retatrutide The Next Weight-Loss Breakthrough After Ozempic And Mounjaro? Here’s How It Works Differently
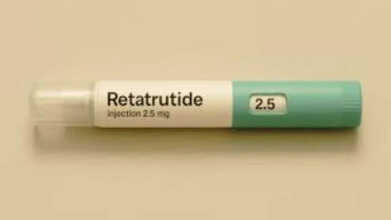
Credits: Canva
A new weight-loss drug often described as the “triple G” treatment because it mimics three hormones linked to hunger and metabolism has delivered striking results in fresh data shared Thursday by its developer, Eli Lilly. In a clinical study involving more than 400 people living with obesity and knee osteoarthritis, the experimental drug retatrutide led to an average weight reduction of 71 pounds, or close to 29% of total body weight, over a period of 16 months, according to figures released by the company. Participants who received retatrutide also reported a 76% drop in knee pain by the end of the study period, based on the same data. So is
What Is Retatrutide?
Retatrutide is an experimental weight-loss drug developed by Eli Lilly and is widely seen as a next-step advancement beyond current GLP-1-based medications such as semaglutide and tirzepatide. While semaglutide acts on a single hormone pathway and tirzepatide works on two, retatrutide targets three.
It activates GLP-1 and GIP, along with an added glucagon pathway, which is why it is sometimes informally referred to as a “GLP-3” drug. Researchers believe this third pathway could explain the greater weight-loss effects seen so far, although retatrutide remains under investigation and has not yet received FDA approval.
Why Is Retatrutide Trending?
Even without regulatory approval, retatrutide has gained attention among gym enthusiasts, fitness creators, and online weight-loss communities. On platforms like TikTok, where direct searches for #reta or #retatrutide are restricted, users often refer to it using coded terms such as “ratatouille.”
At the same time, the drug has been in the news due to growing concerns about counterfeit versions. Reports from the UK recently revealed that authorities seized more than £250,000 worth of fake weight-loss injection pens labelled as tirzepatide and retatrutide from a hidden factory in Northampton. These products are especially concerning because retatrutide is still in clinical trials and has not been approved for use anywhere in the world.
How Is Retatrutide Different Than Other Weight-Loss Drugs?
Retatrutide works by mimicking three hormones that play a role in appetite and metabolism: GLP-1, GIP, and glucagon. In contrast, most weight-loss drugs currently available target only one or two of these pathways. Ozempic and Wegovy, made by Novo Nordisk, copy the effects of GLP-1, a hormone that influences the brain, pancreas, stomach, liver, and muscles, according to the National Institutes of Health.
Mounjaro and Zepbound, on the other hand, act on both GLP-1 and GIP, a hormone involved in blood sugar regulation through insulin stimulation. Retatrutide’s added glucagon effect is key, as glucagon is known to support fat burning, even when the body is at rest. Ozempic and Mounjaro are approved by the FDA for treating Type 2 diabetes, while Wegovy and Zepbound are approved for people with overweight or obesity. As with any prescription drug, it is important for individuals to consult a healthcare professional to determine whether these treatments are appropriate for them.
When Is Retatrutide Expected To Be Available To Consumers?
There is currently no confirmed timeline for when retatrutide might become available by prescription. Its launch will depend on the FDA’s detailed evaluation of clinical trial data once it is formally submitted. Based on current expectations, approval is unlikely before late 2026 and could potentially extend into 2027 or even 2028.
Nicotine Pouches: Are They Really A Safer Alternative To Smoking, Or Just Another Health Risk?

Credits: Canva
The use of nicotine pouches is rising sharply across the UK, especially among young adults, recent research suggests. These small pouches sit between the lip and gum and release nicotine gradually into the body. Available in many flavours, they often include sweeteners and plant-based fibres. But are they truly a better option than smoking, or could nicotine pouches still pose health risks? We take a closer look below.
What Are Nicotine Pouches?
Nicotine pouches are small, tobacco-free sachets that contain nicotine powder along with flavourings and fillers. They are placed between the lip and gum, similar to snus, allowing nicotine to be absorbed without smoke, vapour, or spitting. Marketed as a discreet way to consume nicotine, they still deliver a highly addictive substance and expose users to certain chemicals. Health experts have raised concerns, particularly for young people, despite these products often being promoted as a “safer” choice than cigarettes.
Popular brands such as Zyn, On!, and Velo now dominate a fast-growing market, according to the CDC. Like vaping, they do not contain tobacco and are generally viewed as less harmful than smoking.
A recent study led by researchers at University College London (UCL) found that over the past five years, about 522,000 additional people in the UK have started using nicotine pouches, with usage rising from 0.1% to 1% of the adult population.
This has raised an important question: are nicotine pouches actually safer than smoking, and what is driving their sudden popularity?
Nicotine Pouches: Is Using Them Safer Than Smoking?
Speaking on *Mornings with Ridge and Frost*, lead study author Dr Harry Tattan-Birch from UCL’s Institute of Epidemiology and Health Care told Sky News that the risks linked to nicotine pouches are much lower than those associated with smoking. “There’s no tobacco and no combustion,” he explained. “And we know it’s the burning of tobacco that causes most smoking-related diseases.”
That said, Dr Tattan-Birch and his colleagues stressed that these products are not harmless and should never be accessible to children. The NHS notes that while nicotine itself does not cause serious diseases in the way tobacco does, young people’s developing brains and lungs are more vulnerable to its effects, and dependency can form quickly.
UCL research fellow Eve Taylor also told Sky News that nicotine pouches are “far less harmful than smoking,” but cautioned that they are still relatively new. Because of this, their long-term effects are not yet fully understood. “We can look at what’s in them to estimate potential risks,” she said. “They’re not risk-free. Users are still exposed to some toxic substances, even if the levels are much lower.”
Nicotine Pouches: Are Pouches Helping People Quit Smoking?
According to UCL’s findings, among participants surveyed between January 2022 and March 2025, 69% of nicotine pouch users were also using other nicotine products. More than half of them, 56%, were still smoking cigarettes. Around one in six users, or 16%, reported that they had never been regular smokers, suggesting the habit was not linked to quitting cigarettes.
As quoted by Sky News, Dr Tattan-Birch said the public health impact of nicotine pouches depends largely on who is using them. “If a young person who might otherwise smoke switches to pouches, that could reduce harm,” he said. “But if someone who wouldn’t have used nicotine at all starts using them, the risk of harm goes up.”
Researchers added that more studies are needed to understand whether nicotine pouches genuinely help people stop smoking in the long run.
Are Nicotine Patches Harmful For Health?
Nicotine patches are widely regarded as safer than smoking and are a well-established aid for quitting. They provide a steady dose of nicotine to reduce cravings without exposing users to tar or cancer-causing chemicals found in cigarettes. However, they are not completely without side effects. Common issues include skin irritation, headaches, and sleep disturbances. People with serious heart conditions or those who are pregnant are advised to speak with a doctor before using them, as nicotine can still affect heart rate and blood pressure, though far less dangerously than smoking, according to the CDC.
Taking This Everyday Pill During Flu Could Be Risky, UKHSA Warns

Credits: Canva
People have been advised not to rely on a commonly used medicine when dealing with flu or cold symptoms. The UK Health Security Agency (UKHSA) has released an important warning about the use of antibiotics. Antibiotics are drugs designed to treat bacterial infections. They work by killing bacteria or stopping them from growing and multiplying. But why are health authorities urging caution against antibiotics during the current rise in flu cases?
Flu Influenza: Super Flu Cases Rising In UK And US
This year, a new strain of influenza, known as influenza A H3N2 or the subclade K variant, is spreading quickly across several countries, including the United States, according to Fox News. This week, the Centers for Disease Control and Prevention reported an 8.1% increase in positive flu tests across the country.
The UK is facing a similar situation. The NHS has warned that hospitals in England are dealing with a “worst case scenario” this December due to a surge in so-called “super flu” cases. An average of 2,660 patients per day were hospitalised with flu during the first week of December, the highest number ever recorded for this time of year and a 55% jump from the previous week.
Flu Influenza: Why Is UKHSA Warning Against Taking Antibiotics During Super Flu?
Antibiotics are medicines specifically meant to fight bacterial infections by destroying bacteria or preventing them from spreading. This helps the body’s immune system clear the infection. However, it is important to understand that antibiotics do not work on viral infections. These include illnesses such as the common cold, flu, and COVID-19.
In a post shared on social media platform X, the UKHSA stated: “Antibiotics don’t work for colds and flu – pharmacists can advise you on how to treat your symptoms.”
Flu Influenza: Guidelines On Using Antibiotics During Super Flu
The UKHSA has urged people to follow a few “simple” rules when it comes to antibiotics:
- Don’t take them for colds or flu
- Don’t save them to use later
- Take them exactly as prescribed
This advice comes as flu cases continue to rise across the UK. Data from the UKHSA showed that in the week ending December 7, flu positivity in England increased, with the weekly average reaching 21 per cent, up from 17 per cent the week before.
Hospital admissions linked to flu also rose to 10.05 per 100,000 people, compared with 8.09 per 100,000 previously.
Flu Influenza: Antibiotic-Resistant Infections
The warning follows the publication of the UKHSA’s English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) report in November. The report revealed that around 400 people each week in England are diagnosed with antibiotic-resistant infections.
These infections are harder to treat and can result in serious health problems. Experts say that the excessive use of antibiotics over time has reduced their effectiveness, leading to the rise of so-called “superbugs.”
The NHS explains that these are types of bacteria that have developed resistance to several antibiotic treatments, including:
- MRSA (methicillin-resistant Staphylococcus aureus)
- Clostridium difficile (C. diff)
- The bacteria responsible for multi-drug-resistant tuberculosis
The NHS has warned: “These infections can be serious and difficult to treat, and are becoming an increasing cause of disability and death worldwide. The greatest concern is that new strains of bacteria could develop that cannot be treated with any existing antibiotics.”
Dr Alicia Demirjian, consultant epidemiologist and clinical lead for antimicrobial resistance and prescribing at the UKHSA, said: “Antibiotic resistance is one of the biggest threats to modern medicine, but the good news is that we can all help reduce it.”
When a GP prescribes antibiotics, it is vital to follow the instructions carefully and not miss any doses.
The NHS advises: “If you forget to take a dose of your antibiotics, check the patient information leaflet that comes with your medicine to see what to do. If you’re unsure, speak to a pharmacist or your GP.
“In most cases, you can take the missed dose as soon as you remember and then continue the course as normal. But if it’s nearly time for your next dose, skip the missed one and carry on with your regular schedule.” You should never take a double dose to make up for a missed one.
Disclaimer: This article is for informational purposes only and is not intended as medical advice. Antibiotics or any other medicines should only be taken after consulting a qualified healthcare professional. Always follow the guidance of your doctor, pharmacist, or local health authority regarding diagnosis and treatment.
© 2024 Bennett, Coleman & Company Limited

