- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
What Is Swimmer's Itch? How To Get Rid Of This Common Summertime Rash

Credit: Canva
Swimmer's itch is a rash caused by an allergic reaction to the larvae of microscopic parasites that are found in both fresh and saltwater. These parasites commonly live in snails, which secrete larvae into the water, per the CDC.
Swimming in contaminated water for even a short period of time can cause swimmer’s itch, and after you come in contact with the larvae, “when the skin dries off, those parasites burrow under people's skin and cause an itchy rash,” says Dr. Christina Boull, MD, an associate professor of dermatology and pediatrics at M Health Fairview University of Minnesota Medical Center. Read on to learn what symptoms to look out for and precautions you can take to prevent this uncomfortable summertime rash.
What Is Swimmer's Itch?
You can identify swimmer’s itch, also known as cercarial dermatitis, from the little red dots that appear on your skin after you’ve been exposed to the parasites, Boull says. The rash will likely manifest on skin that was directly exposed to the water as opposed to skin protected by your bathing suit. For this reason, your arms and legs are particularly vulnerable to swimmer’s itch, she says.
These dots typically appear 12 hours after exposure, and over the next day or two, some people may experience a more severe reaction with welts and blisters. “One of the main risk factors of complications from this rash would be a secondary bacterial infection.” If you scratch the rash, there’s a possibility of staph bacteria getting under your skin, leaving your body vulnerable to developing staph infections such as impetigo or cellulitis, she says.
What Can Be Mistaken For Swimmer's Itch?
When it comes to swimming in the ocean, seabather’s eruption is a rash that presents similar symptoms to swimmer’s itch. In terms of identifying whether your rash is swimmer’s itch or sea bather’s eruption, the latter tends to develop under a swimsuit, Boull explains. Comparatively, swimmer’s itch is more likely to appear in areas that are not protected by a swimsuit, she reiterates. Additionally, because swimmer’s itch presents as small red bumps, it is also commonly mistaken as bites caused by small bugs, such as gnats or mosquitoes, Boull says.
How Do You Get Rid Of Swimmer's Itch?
"The good news is that it spontaneously resolves," Boull says. Because people are the preferred hosts of the mites, they don’t live in the skin very long. Typically, the rash and itch significantly improve over the course of a week, although it's possible for it to last as long as three weeks, she says.
To quell the itching of the rash, Boull suggests 1% hydrocortisone, an over the counter topical steroid cream. She also recommends taking an oral antihistamine. In cases of severe itch, prescription oral prednisone and oral cortisone medicines can help relieve itch and inflammation.
If your swimmer’s itch has developed into blistering, open sores, and you’re experiencing fever, it could be signs of a secondary bacterial infection. In this case, it’s essential you see a doctor who can prescribe you oral antibiotics, Boull says.
Does Showering Kill Shower's Itchh?
The parasites that cause swimmer’s itch can only burrow into your skin after you’ve dried off. “So, it's really important after getting out of a lake or areas where you're swimming that would have snails, that you take a towel and really wipe the water off your skin.” Showering after you’ve gotten out of the water can also help prevent the parasites from getting underneath your skin.Does chlorine damage hair? Here’s how to protect your hair this swim season.
Snails tend to prefer warm, shallow water, so avoiding these areas can limit the possibility of exposure to the parasites. Finally, take note of no-swim zone signs that may indicate whether there are pathogens in the water.
Colorectal Cancer: The Preventable Tragedy
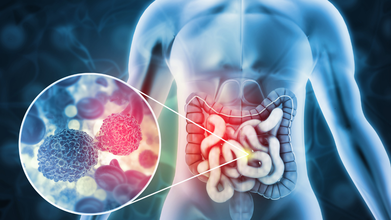
Credit: iStock
In the world of oncology, we usually speak of battling or fighting cancer. We pool in our whole life’s earnings to find a cure or solution for the advanced stages of this disease. What if cancer were not a threat?
Here is one of the most common and deadly cancers, which is also one of the most preventable ones. We are talking about Colorectal cancer, which is often described by medical professionals as a preventable tragedy. This is because, unlike many other forms of the disease, we have a clear window of opportunity to stop it before it even begins.
As we observe Colorectal Cancer Awareness Month in March, it is time to strip away the fear surrounding the tests and understand why nobody should ever have to die from a condition that gives many chances to catch it well in time.
How It All Begins
To understand why colorectal cancer is preventable, we have to look at how it develops. As with most cancers, this too doesn’t appear overnight. Almost always, these cancers start as small growths called polyps or precancerous lesions on the inner lining of the colon or rectum.
These polyps are like seeds; they are mostly benign. But there is one type of polyp that can gradually turn into cancer over a period of time. This is where the advantage lies. There is a long interval of time before polyps develop into cancer.
During this time, they can be removed if they are identified. If a doctor removes a precancerous polyp during a routine screening, they would not only have nipped the cancer in the bud, but would have also prevented it from occurring.
The statistics are encouraging when detected early, with figures showing that over 90 per cent of cases of colorectal cancer are fully curable. However, people do not seek medical attention until they experience some symptoms, at which point the seed-like polyps have already grown into a deep-rooted cancer.
Screening – The Main Defense
In Western countries, the death rate from colorectal cancer has been declining at a visible rate due to the presence of strong and well-supported screening programs from their governments.
Although some countries have not yet introduced a formal national program, the consensus among medical experts is that if you are above 45 years of age or have high-risk factors, you need to take the initiative to be screened.
There are two primary ways we do this:
1. The FIT (Fecal Immunochemical Test) – This is a simple, non-invasive stool test that has become a staple in most general health check-up packages. It works by detecting tiny amounts of human hemoglobin (blood) that aren’t visible to the naked eye.
The advantage of getting a Fecal Immunochemical Test done is that it is very easy, and it can be done at home, and requires no special preparations. It acts as an early warning system. If a FIT result comes back high, it signals that something is happening in the bowel that requires a closer look via colonoscopy. It is recommended that everyone over 45 undergoes this test annually. While not as definitive as a colonoscopy, it is a vital first line of defence.
2. The Colonoscopy – This is the gold standard. Despite all the fear and misinformation that can be spread on the Internet, a colonoscopy is a routine and safe procedure. It allows a doctor to visually inspect the inside of the colon. It is a procedure that has dual benefits – to see what is wrong, and to make things right. Should the doctor find a polyp, it can be safely removed at the time of the procedure.
Many people avoid this procedure because of embarrassment and fear of discomfort. However, with the sedation, most people find it to be completely painless.
Recognizing The Red Flags
While screening is for people with no symptoms, you must be alert to signs that require an immediate expert opinion, regardless of your age. Also, never ignore these symptoms or assume that they are due to bad food choices:
- If you feel changes in bowel habits frequently, then this is not just a one-off upset stomach. Pay attention to persistent change, such as recurrent diarrhea or a sudden onset of constipation that doesn’t resolve.
- Blood in the stool is perhaps the most critical sign. Many people write off rectal bleeding as piles (hemorrhoids). But bleeding that persists despite treatment must be checked by an expert.
- Losing weight without trying is often a sign that the body is under significant stress. Not all unexpected weight loss is a happy occurrence.
- Anemia and fatigue are visible proof. If a blood test shows low hemoglobin or iron-deficiency anemia – especially in men or in post-menopausal women – a colonoscopy is often mandatory to rule out internal bleeding from a tumor.
- Persistent abdominal pains, which are chronic, severe, or are accompanied by unexplained cramping and pain in the lower tummy area, must be evaluated by a doctor.
Breaking The Stigma
The aim of Colorectal Cancer Awareness Month is not just to create awareness about the disease; it is also about providing support as we pay tribute to cancer warriors who have completed the painful journey from surgery and chemotherapy to rehabilitation. Shared stories can help remove the fear in others’ minds.
There is no such thing as too much information in the doctor’s office. Our bowels are part of our body, and we must overcome the shame or embarrassment associated with talking about them. A simple dialogue about bathroom habits or asking for a FIT test can save a life.
By promoting early detection leading to the removal of precancerous polyps, we can build a world where no one ever has to die from colorectal cancer. If you are aged 45 years or older, make this the month you arrange for a screening. If you have symptoms, do not wait; the right time is now.
In the case of colorectal cancer, prevention is not just the best medicine, it IS the cure.
No Smoking Day: Are There Science-backed Methods To Quit Smoking?

Credits: Canva
On No Smoking Day, we drive our focus to science-backed methods that can help one leave smoking. Smoking is one of the leading causes of preventable deaths worldwide. It also contributed to severe health problems, including cancer, cardiovascular diseases, and respiratory diseases. Even though many people are aware of this harmful consequences, many struggle to quit smoking. Mostly because it is a habit often associated to enjoying a break. Even when someone does not need it, their brain tricks them into believing that smoke is important for the break they are meant to enjoy.
However, there are several studies that have explored science-backed methods that could help one to quit smoke.
A study published in the journal Addiction, emphasizes three primary methods proven effective for quitting smoking: behavioral support, prescription medications, and nicotine replacement therapy (NRT). These strategies have shown varying levels of success in aiding smokers to quit permanently. In addition, alternative methods like e-cigarettes and mindfulness-based techniques have gained traction in helping reduce smoking addiction.
Quitting smoking is more than just a decision; it’s a commitment to significantly improving your health and well-being. Smoking has been directly linked to various cancers, lung diseases, and heart conditions. In the long term, stopping smoking can lower your risk of these life-threatening conditions.
According to the study, individuals looking to quit smoking should consider using Varenicline (sold as Chantix/Champix), Cytisine (a plant-based supplement available in Europe and Canada), or nicotine e-cigarettes.
“Quitting smoking is difficult, and some people find it harder to quit than others, but tobacco is uniquely deadly among legal consumer products, so it’s important to seek help quitting,” said lead investigator Jonathan Livingstone-Banks, a lecturer and researcher in evidence-based health care with the University of Oxford in the U.K.
Read: Does Smoking Affect Women Differently Than Men?
What Happens When You Stop Smoking?
- In just 20 minutes of stopping, your blood pressure and heart rate begin to normalize.
- Within a few weeks, your lung function improves.
- Over time, the risk of heart disease and cancer also decreases dramatically.
Three Science-backed Methods That Could Help You Quit Smoking
Behavioral Support
Quitting smoking isn’t just about resisting cravings. Often, behavioral support through counseling or therapy is crucial for tackling the psychological aspects of addiction. Behavioral therapy involves working with a trained professional to identify triggers, develop coping strategies, and create a tailored quit plan. Research shows that combining counseling with other quit methods can significantly increase success rates.
Prescription Medications
Some medications, such as varenicline (Chantix) and bupropion (Zyban), have been shown to help people quit smoking by reducing cravings and withdrawal symptoms. Experts suggest that varenicline works by blocking the effects of nicotine in the brain, while bupropion is an antidepressant that helps manage withdrawal symptoms. Both medications are generally more effective when combined with behavioral therapy.
Nicotine Replacement Therapy (NRT)
Nicotine replacement products, such as nicotine patches, gums, lozenges, and nasal sprays, deliver controlled amounts of nicotine to ease withdrawal symptoms. According to experts at Harvard Health, NRT can double the chances of quitting by alleviating physical cravings while the person works on overcoming the psychological addiction.
The Silent Rise of Fatty Liver Disease: How India-Specific Guidelines Can Help

Metabolic dysfunction-associated steatotic liver disease (MASLD), previously called fatty liver disease, is becoming extremely common in people with type 2 diabetes in India.
Studies suggest that 50–70 percent of Indians with type 2 diabetes may have fatty liver, and a significant proportion can progress to inflammation, liver fibrosis, cirrhosis, or even liver cancer if the condition is not detected early. Because India already has one of the world’s largest populations with diabetes, MASLD is emerging as a major but under-recognized public health problem.
The recently published consensus guidelines developed by Indian experts aim to provide practical, India-specific recommendations for diagnosing and managing MASLD in people with type 2 diabetes.
In fact, these are the first global guidelines for MASLD and type 2 diabetes, albeit restricted to India. This matters because most existing international guidance—including from organizations such as the American Diabetes Association—is largely based on evidence and healthcare systems in high-income Western countries. These recommendations often assume easy access to expensive diagnostic tests and medications, which may not always be feasible in India.
In India, healthcare costs are frequently paid out-of-pocket by patients. Advanced imaging tests or newer medications can therefore be unaffordable for many people.
The Indian consensus addresses this reality by recommending step-wise and cost-effective screening strategies, beginning with simple clinical risk assessment and basic laboratory tests, followed by non-invasive fibrosis scoring tools and ultrasound when appropriate. This approach helps identify high-risk individuals without overburdening patients or the healthcare system.
Another important reason these guidelines matter is that Asian Indians have a unique metabolic profile. Compared with Western populations, Indians often develop diabetes and fatty liver at younger ages and lower body weight, partly because of higher abdominal fat and insulin resistance. Therefore, early screening for liver disease in people with diabetes becomes particularly important in India.
Dietary recommendations are also adapted to local eating patterns. Instead of focusing on Western dietary models, the guidelines emphasize reducing refined carbohydrates, excess sugars, and unhealthy fats common in Indian diets while promoting traditional, healthier foods, whole grains, legumes, and increased physical activity.
In simple terms, these India-specific guidelines aim to ensure that more patients with diabetes are screened early, treated appropriately, and protected from severe liver complications, using strategies that are practical, affordable, and suited to the realities of the Indian healthcare system.
How These Guidelines Differ From Those In The West
Guidelines for MASLD developed in Western countries provide important scientific guidance, but they are often designed for healthcare systems with greater resources and different patient characteristics. The Indian consensus recommendations differ in several key ways to make them more suitable for local populations and healthcare settings.
First, screening strategies are more pragmatic and cost-conscious. Western guidelines often recommend advanced imaging tests or specialized biomarkers to assess liver fat and fibrosis. However, these tests can be expensive and not widely available in many parts of India.
The Indian recommendations emphasize simple, widely available tools—such as routine blood tests and non-invasive fibrosis scoring systems—before considering more advanced imaging. This stepwise approach ensures that patients who are most at risk are identified while keeping costs manageable.
Second, the guidelines recognize the unique metabolic risk profile of Asian Indians. Compared with Western populations, Indians tend to develop metabolic diseases such as type 2 diabetes and fatty liver at younger ages and lower body mass index (BMI). Abdominal obesity and insulin resistance are particularly common.
Therefore, the Indian recommendations stress earlier and more vigilant screening for MASLD in people with diabetes, even if they are not severely obese.
Third, treatment priorities differ because of affordability and access to medications. Western guidelines may emphasize newer and often expensive drugs that show benefits for fatty liver disease. While these therapies can be effective, they may not be accessible to many patients in low- and middle-income countries.
The Indian consensus places stronger emphasis on lifestyle interventions, weight reduction, improved diet, and physical activity as the foundation of treatment, while suggesting pharmacotherapy selectively based on evidence, availability, and cost.
Fourth, perhaps the most important difference, dietary advice is culturally tailored. Western guidelines typically discuss Mediterranean-style diets.
In contrast, the Indian recommendations translate healthy eating principles into Indian dietary patterns, focusing on reducing refined carbohydrates, sugar-sweetened foods, and excess saturated fats while promoting whole grains, pulses, vegetables, and traditional balanced meals.
Finally, the Indian document highlights the need for public health awareness and primary care involvement, since a large proportion of patients with diabetes are managed outside specialized centers.
Overall, the key difference is that while Western guidelines provide strong scientific foundations, the Indian recommendations adapt those principles to local realities.
© 2024 Bennett, Coleman & Company Limited

