- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Why Allergies Are Almost Nonexistent In Children From THIS Community

(Credit-Canva)
One of the many beliefs that people hold, especially the older generation, is that the new way of living, which is highly protected and sanitized, has made kids weaker. While there are certain evolutionary changes we have developed over the past few centuries, it is arguable whether we are . However, their theory may not be far from the truth, but how do we know that? To this day, there are certain communities who enjoy a quiet living, void of modern possessions like the Amish community.
Surveys have noted that Amish children tend to have lesser allergies or asthma cases, but how?
Why Do Amish Children Have Less Allergies?
Scientists have long known that kids who grow up on traditional farms are less likely to have asthma and allergies. This is called the "farm effect," and it seems to be caused by being around farm animals, especially cows, and the microbes (tiny living things) that are found there.
In a 2018 study, researchers from The University of Manchester and Northern Care Alliance NHS Foundation Trust studied two unique farming communities in the U.S.: the Amish and the Hutterites. Both groups have similar genes and lifestyles, but they farm in very different ways, and this seems to be the reason for their different health outcomes.
Another 2020 study done by the American College of Allergy Asthma & Immunology compared the living of Amish and Old Order Mennonite, who also have a similar style of living, with a few comparable changes.
What Is The Difference Between Amish And Hutterite Living?
The Amish and Hutterites both came from the same group in Europe and have similar lifestyles. They eat similar foods, have large families, and avoid many modern habits like having indoor pets or using the internet. However, their farming practices are completely different.
Amish Farms
The Amish use old-fashioned, family-run farms with horses for work. Their barns are close to their homes, so children are around the animals and barn dust from a young age.
Hutterite Farms
The Hutterites live on large, modern, industrial farms. Their barns are big and located far from their homes, so children have little contact with the animals or barn environment.
This difference in lifestyle led to a major difference in health. The study found that Amish children have a very low rate of asthma (just 5.2%), while Hutterite children have a much higher rate (21.3%). This shows that the environment, not their genes, is the most important factor in preventing asthma.

How Was Amish Health Different From Mennonite Health?
The 2020 study researchers created a survey to compare the health of these two groups. They asked families about different types of allergies they had, as well as their lifestyle and farming practices.
They found that families in both groups lived on farms and drank raw, unprocessed milk. However, the Amish families had more children on average and lived on smaller farms with fewer animals compared to the Mennonite families. The survey results showed a significant difference in health between the two groups:
The Amish families reported having a much lower rate of allergies overall. Only about 26% of Amish households had a family member with an allergy.
The Mennonite families had a much higher rate of allergies, with nearly 47% of households reporting an allergy.
Why Were The Amish Less Likely To Get Allergies?
One key difference is that while both the Amish and Mennonites have large families, Mennonite communities sometimes use modern technology like tractors and electricity. In contrast, the Amish stick to traditional, old-fashioned farming.
This difference in farming methods could change the types of microbes (tiny living things) found in the farm environment. Since other research has shown that these specific microbes are important for preventing allergies, the different farming practices might explain why the Amish have a much lower allergy rate.

How the Environment Protects Against Asthma
The scientists found a key difference in the homes of the two groups: Amish homes had much more endotoxin, a type of dust from bacteria. When this dust was tested on mice, the dust from Amish homes protected the mice from developing asthma. However, dust from Hutterite homes actually made the mice's asthma worse.
This suggests that the kind of dust and microbes you are exposed to matters. The dust in Amish homes is full of "good" microbes that help a child’s immune system grow and develop correctly, preventing it from overreacting and causing asthma.
How Does Immunity Affect Allergies And Asthma?
The study also looked at the children's blood and immune systems. They found that the Amish children’s immune systems were very different from the Hutterite children's. The Amish kids had a stronger innate immune system, which is the body's first defense against germs. Their immune cells were "calm" and seemed to be trained to not overreact to things that can trigger asthma.
This research strongly suggests that the farm effect works by "training" the immune system. Early exposure to a wide variety of microbes helps the body learn how to respond correctly, which in turn protects against asthma.
While these studies give us a lot of great information, there are still many questions to answer. Scientists still need to figure out exactly which microbes or substances in the farm environment are the most protective. They also need to study children at a younger age to see how their immune systems change over time.
But for now, the findings from this research confirm that growing up on a traditional farm and being exposed to its rich environment is a powerful way to protect against asthma and allergies.
Men Lose Their Y Chromosomes As They Age, Here's Why It Matters
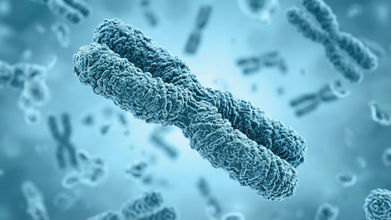
Credits: Canva
For decades, scientists believed the gradual loss of the Y chromosome in ageing men did not matter much. But a growing body of research now suggests otherwise. Studies show that losing the Y chromosome in blood and other tissues is linked to heart disease, cancer, Alzheimer’s disease and even shorter lifespan. The crux is simple but striking. As men age, many of their cells quietly lose the Y chromosome, and this loss may be shaping men’s health in ways we are only beginning to understand.
Aging And The Disappearing Y Chromosome
Men are born with one X and one Y chromosome. While the X carries hundreds of important genes, the Y is much smaller and contains just 51 protein coding genes. Because of this, scientists long assumed that losing the Y in some cells would not have serious consequences beyond reproduction.
However, newer genetic detection techniques tell a different story. Research shows that about 40 percent of men aged 60 have some cells that have lost the Y chromosome. By age 90, that number rises to 57 percent. Smoking and exposure to carcinogens appear to increase the likelihood of this loss.
This phenomenon, known as mosaic loss of Y, does not occur in every cell. Instead, it creates a patchwork in the body where some cells carry the Y chromosome and others do not. Once a cell loses the Y, its daughter cells also lack it. Interestingly, Y deficient cells seem to grow faster in laboratory settings, which may give them a competitive edge in tissues and even in tumors.
Why Would Losing The Y Matter?
The Y chromosome has long been viewed as mainly responsible for male sex determination and sperm production. It is also uniquely vulnerable during cell division and can be accidentally left behind and lost. Since cells can survive without it, researchers assumed it had little impact on overall health.
Yet mounting evidence challenges that assumption. Several large studies have found strong associations between loss of the Y chromosome and serious health conditions in older men. A major German study reported that men over 60 with higher levels of Y loss had an increased risk of heart attacks. Other research links Y loss to kidney disease, certain cancers and poorer cancer outcomes.
There is also evidence connecting Y loss with neurodegenerative conditions. Studies have observed a much higher frequency of Y chromosome loss in men with Alzheimer’s disease. During the COVID pandemic, researchers noted that men with Y loss appeared to have worse outcomes, raising questions about its role in immune function.
Is Y Loss Causing Disease?
Association does not automatically mean causation. It is possible that chronic illness or rapid cell turnover contributes to Y loss rather than the other way around. Some genetic studies suggest that susceptibility to losing the Y chromosome is partly inherited and tied to genes involved in cell cycle regulation and cancer risk.
However, animal research offers stronger clues. In one mouse study, scientists transplanted Y deficient blood cells into mice. The animals later developed age related problems, including weakened heart function and heart failure. This suggests the loss itself may directly contribute to disease.
A New Chapter In Men’s Health
So how can such a small chromosome have such wide ranging effects? While the Y carries relatively few genes, several of them are active in many tissues and help regulate gene activity. Some act as tumor suppressors. The Y also contains non coding genetic material that appears to influence how other genes function, including those involved in immune responses and blood cell development.
The full DNA sequence of the human Y chromosome was only completed recently. As researchers continue to decode its functions, the message for men’s health is becoming clearer. Ageing is not just about wrinkles or grey hair. At a microscopic level, the gradual disappearance of the Y chromosome may be quietly influencing heart health, brain health and cancer risk.
Understanding this process could open new doors for early detection, personalized risk assessment and targeted therapies that help men live longer and healthier lives.
Udit Narayan’s First Wife Alleges She Was Forced to Undergo Hysterectomy, Files Police Complaint
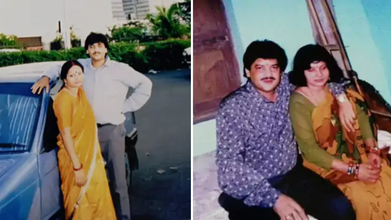
Credits: Facebook
First wife of singer Udit Narayan, Ranjana Narayan Jha made serious allegations against him, claiming that he forced her to get hysterectomy. She filed a police complaint earlier this week at the Women's Police Station in Supaul district, Bihar.
She accused Udit Narayan and his two brothers Sanjay Kumar Jha and Lalit Narayan Jha and his second wife Deepa Narayan of a criminal conspiracy that lead to hysterectomy - the surgical removal of uterus, without her knowledge. As per an NDTV report, "She claimed she became aware of this only years later during medical treatment."
Udit Narayan's First Wife's Allegations
As per the complaint, Udit and Ranjana were married on December 7, 1984, in a traditional Hindu ceremony. Udit then moved to Mumbai in 1985 to pursue his music career. She later learned through media that he had married another woman Deepa. As per the complaint, he continued to mislead her whenever she confronted him.
As per the complaint, in 1996, she was taken to a hospital in Delhi under the pretext of medical treatment, where, she claims that her uterus was removed without her knowledge. She said that she was compelled to file a complaint years after being ignored. "You all know that Udit Narayan ji repeatedly makes promises but does not fulfill them. He has not done anything till now, which is why I have come to the Women's Police Station. I deserve justice," she said.
"Nowadays, I am constantly unwell and need his support. But Udit Narayan is neither saying anything nor doing anything. He came to the village recently and left after making promises once again," she said, as per a Hindustan Times report.
What Is Hysterectomy?
It is the surgical removal of one's uterus and cervix. There are different kinds of hysterectomy available, which depends on the condition of the patients.
Total Hysterectomy
This removes uterus and cervix, but leaves ovaries. This means the person does not enter menopause after the surgery.
Supracervical Hysterectomy
Removing just the upper part of the uterus and leaving the cervix. This could also be when your fallopian tubes and ovaries are removed at the same time. Since, you have a cervix, you will still need Pap smears.
Total Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes and ovaries. This will start menopause immediately after the surgery.
Radical Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes, ovaries, the upper portion of your vagina, and some surrounding tissue and lymph nodes. This is done to people with cancer. Patients who get this enter menopause right after the surgery.
Lorna Luxe's Husband John Dies After Three Year Long Cancer Battle

Credits: Instagram
Lorna Luxe's Husband, 64, John Andrews passed away after a three-year-long cancer battle. On February 11, the British influencer shared a post on her Instagram. The 43-year-old wrote: "My beautiful, brave John died yesterday. I am heartbroken. We were together to the every end, at home, in our own bed and holding hands which is exactly what he wanted."
Lorna Luxe's Husband John Dies: What Happened To Him?
John, a former banker, was diagnosed with stage three cancer in 2023. He had been receiving treatment over the last three years. John's cancer also entered remission and it returned in 2024 and spread to his brain.
He underwent a surgery in 2025, however, he was back in hospital in December after a complication with his chemotherapy treatments. This led to organ failure.
In January this year, Lorna told her followers that she was "looking for a miracle" and shared that his cancer had "progressed to his other organs" and treatment was "no longer an option".
“I think he's possibly the bravest person. And I suppose at this point we're looking for a bit of a miracle and we're going to take each day as it comes,” she wrote on her post.
In her post that announced John's death, she wrote when she asked him how he was feeling, her husband responded, "Rough, but in love".
Read: Catherine O'Hara Cause Of Death Is Pulmonary Embolism; She Also Had Rectal Cancer
Lorna Luxe's Husband John Dies: Can Cancer Spread To Other Organs?
While John's cancer has not been specified, but the reports reveal that his cancer spread to other organs. According to National Institution of Health (NIH), US, the spreading of cancer to other parts of the body is called metastasis.
This happens when cancer cells break away from where they first formed, and travel through the blood or lymph system. This could lead to formation of new tumors in other parts of the body. Cancer can spread to anywhere in the body, however, it is common for cancer to move into your bones, liver, or lungs.
When these new tumors are found, they are made of the same cells from the original tumor. Which means, if someone has lung cancer and it spread to brain, the cells do not look like brain cancer. This means that the cancer cells in the brain is metastatic lung cancer.
Cancer cells could also be sent to lab to know the origin of the cell. Knowing the type of cancer helps in better treatment plan.
Lorna Luxe's Husband John Dies: Could Chemotherapy Lead To Organ Damage?
As per the University of Rochester Medical Center, in some cases, chemotherapy could cause permanent changes or damage to the heart, lungs, nerves, kidneys, and reproductive organs or other organs.
For instance, some anti-cancer drugs cause bladder irritation, it could result in temporary or permanent damage to kidneys or bladder. In other cases, chemotherapy could also have potential effects on nerves and muscles. Chemotherapy could also damage the chromosomes in the sperm, which could also lead to birth defects. In females, it could damage the ovaries and could result in short-term or long-term fertility issues.
Chemotherapy could also induce menopause before the correct age and could cause symptoms like hot flashes, dry vaginal tissues, sweating, and more.
For some, it could also cause a 'chemo-brain', which is a mental fog that many chemotherapy patients face, that could affect memory or concentration.
© 2024 Bennett, Coleman & Company Limited

