- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Wildfire Smoke May Rewire Your Immune System, Scientists Warn: Here’s How It Impacts Your Health

Credits Canva
As wildfires become an all-too-familiar headline across the globe, their visible devastation—scorched forests, lost homes, and displaced communities—often overshadows a more insidious threat: the impact of wildfire smoke on human health. While the immediate dangers of flames and evacuations are clear, a new study published in Nature Medicine reveals that wildfire smoke does far more than irritate eyes and throats. It can fundamentally alter the immune system, potentially making people more susceptible to illness long after the smoke has cleared.
The study, led by researchers from the Harvard T.H. Chan School of Public Health, found that people exposed to wildfire smoke exhibit changes in gene expression and immune function, even if they’re otherwise healthy. This suggests that the health consequences of wildfires may extend far beyond the immediate coughing, wheezing, and watery eyes that so many experience during fire season.
How Smoke Alters Immunity?
The research, led by Dr. Kari Nadeau of the Harvard T.H. Chan School of Public Health, provides the most detailed look yet at how wildfire smoke affects the body on a cellular level. By analyzing blood samples from 31 firefighters and civilians exposed to wildfire smoke and comparing them to 29 unexposed individuals, the study uncovered a complex web of immune changes.
People exposed to wildfire smoke showed a marked increase in memory immune cells—cells that typically provide long-term immunity. At first glance, this might seem beneficial, but the study also found elevated biomarkers of inflammation and immune activity, as well as changes in dozens of genes linked to allergies and asthma. In short, the immune system was not just activated—it was thrown into overdrive, potentially increasing vulnerability to illness.
Dr. Mary Johnson, the study’s lead researcher, explains, “Our findings demonstrate that the immune system is extremely sensitive to environmental exposures like fire smoke, even in healthy individuals. Knowing exactly how may help us detect immune dysfunction from smoke exposure earlier and could pave the way for new therapeutics to mitigate, or prevent altogether, the health effects of smoke exposure and environmental contaminants.”
What’s in Wildfire Smoke?
Wildfire smoke is a toxic brew. It contains:
- Fine particulate matter (PM2.5)
- Toxic gases
- Heavy metals
- “Forever chemicals” like PFAS
- Cancer-causing compounds
The ultra-fine PM2.5 particles are particularly dangerous. At less than 2.5 micrometers in diameter, they are 28 times smaller than the width of a human hair and can be inhaled deep into the lungs, enter the bloodstream, and affect organs throughout the body.
“These findings suggest that even short-term exposure to wildfire smoke can act as a biological stressor with long-lasting effects,” said Dr. Mary Johnson, lead researcher and environmental health scientist at Harvard. “That’s especially concerning as wildfire seasons grow longer and smoke plumes travel farther.”
What are the Genetic Impacts of Wildfires?
One of the most striking findings of the study was the alteration of 133 genes related to allergies and asthma in those exposed to wildfire smoke. This genetic shift may help explain why people living in wildfire-prone areas often report more respiratory problems, even months after the fires have ended.
The study also found that smoke-exposed individuals had more immune cells affected by toxic metals, further increasing inflammation and the risk of immune dysfunction. These changes may make people more susceptible to infections, worsen existing respiratory conditions, and potentially contribute to the development of new allergies or asthma.
The United States, particularly western states like California, has witnessed a dramatic increase in wildfire frequency and severity. In 2023 alone, California experienced over 7,000 wildfires, with the California Department of Forestry and Fire Protection responding to nearly 590,000 related emergencies. The devastating January 2025 fire in Los Angeles County, which claimed 30 lives and scorched 40,000 acres, underscored the deadly toll of these disasters.
Climate change is a major driver, creating hotter, drier conditions that fuel longer and more intense fire seasons. As wildfires become more common, understanding and mitigating the health risks of smoke exposure is more urgent than ever.
What are the Immediate and Long-Term Health Effects?
Wildfire smoke can trigger a range of symptoms, from burning eyes and runny noses to persistent coughs and breathing difficulties. For people with pre-existing conditions like asthma, COPD, or eczema, exposure can lead to dangerous flare-ups.
But the risks extend beyond the lungs. Fine particulate matter (PM2.5) can enter the bloodstream, causing inflammation throughout the body. Studies have linked wildfire smoke to increased emergency room visits for heart attacks and coronary heart disease within 24 hours of exposure. There is also emerging evidence that PM2.5 can impair cognitive functions such as memory and attention, likely by inducing inflammation in the brain.
How to Protect Yourself and Your Family?
Experts emphasize the need for proactive measures as wildfire season peaks:
- Stay indoors when smoke levels are high. Keep windows closed and seal gaps in doors.
- Use HEPA-grade air purifiers to reduce indoor particle pollution.
- Wear a certified N95 mask when outdoors, especially if you’re in a smoke-affected region.
- Monitor air quality via apps or government alerts, such as AirNow.gov.
- Avoid outdoor exercise when AQI levels are poor; opt for indoor alternatives instead.
- Keep emergency medications handy, especially for people with asthma or heart conditions.
If evacuation orders are issued, follow them promptly—not just for safety from flames, but from the health threats the smoke carries.
As wildfires continue to reshape landscapes and communities, their invisible legacy—on our immune systems and overall health—demands urgent attention. The message from scientists is clear: wildfire smoke is not just an environmental nuisance, but a profound health hazard that can affect anyone, anywhere the wind blows. Proactive measures, informed guidelines, and continued research are essential to protect public health in an increasingly fiery world.
Ronald Acuña Jr. Sidelined with Achilles Tendon Tightness: What It Means and Why It Matters

It’s déjà vu Braves fans didn’t ask for. Ronald Acuña Jr., Atlanta’s powerhouse baseball outfielder and reigning National League MVP, has hit the injured list again, this time with tightness in his right Achilles tendon. Just months after returning from a torn ACL in his left knee, Acuña pulled up sore after sprinting the bases and later chasing a fly ball, exiting Tuesday’s game against the Royals mid-inning.
But what does Achilles tendon tightness actually mean, and why does it freak out athletes and sports doctors alike?
The Achilles tendon, also known as the calcaneal tendon, is the thick band of tissue that connects your calf muscles to your heel bone. It is the biggest and strongest tendon in the human body. But it can bring even the fittest athletes to their knees.
It helps you run, jump, pivot and push off the ground, basically every move an outfielder like Acuña makes in a single play. When it is tight, inflamed or partially torn, that springy propulsion becomes painful and unstable. Cue the limping, grimacing and, in some cases, weeks on the injured list.
Why Achilles Pain Is a Red Flag
Achilles tightness might sound like a minor complaint, but it is often the body’s early warning system. It could stem from overuse, fatigue, poor footwear, or biomechanical imbalances.In Acuña’s case, the discomfort reportedly began the night before while sprinting around the bases and got worse chasing fly balls. That is a classic setup: high-intensity bursts, sudden stops, and quick direction changes, all high-risk moves for the Achilles.
If ignored, tightness can escalate to tendonitis (inflammation), partial tears, or the dreaded rupture, which is basically the tendon snapping in two. That is a season-ending injury, often requiring surgery and months of rehab.
When the Body Says No
Beyond the physical pain, repeated injuries hit hard on the mental game. Acuña admitted he did not want to sit out, even though the pain intensified, because he has already missed too much time.But ignoring Achilles issues can backfire in the worst way. What starts as tightness today could be crutches tomorrow. The tendon does not heal fast, and re-injury is a very real risk if recovery is rushed.
The Game Plan for Recovery
For now, Acuña’s been placed on the 10-day injured list, but tendon issues do not always follow a schedule. He will likely undergo scans to rule out structural damage, followed by rest, anti-inflammatories, and physical therapy to stretch and strengthen the area.Recovery is not just about waiting for the pain to stop; it is about rebuilding strength, restoring flexibility, and ensuring both legs are balanced and strong.
Why This Matters for Everyone Who Plays
This is not just a pro-athlete problem. Achilles injuries are surprisingly common in runners, dancers, and gym-goers. If you feel stiffness in your heel or lower calf, especially first thing in the morning or during exercise, do not brush it off.Stretch regularly, warm up before activity, avoid sudden ramp-ups in intensity, and listen to your body. And if the pain lingers or worsens, see a specialist. Ronald Acuña Jr.’s Achilles flare-up might just be tightness, but it is the kind of tightness that turns trainers serious and fans anxious. It’s also a timely reminder that this tendon is small but mighty, and when it acts up, rest is not optional. Whether you are chasing fly balls or your morning run goal, treat your heels with the caution they deserve.
Manhattan Shooter Cited CTE in Suicide Note: Here Is What the Condition Means
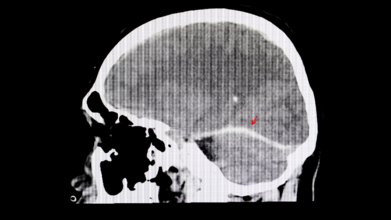
A recent tragic shooting in Midtown Manhattan has pulled an obscure but alarming brain disease back into the headlines. The shooter reportedly left behind a suicide note claiming he suffered from CTE, short for chronic traumatic encephalopathy, a condition linked to repeated head trauma. As shocking as the incident was, it has opened up a floodgate of questions: What exactly is CTE? Can it really make someone act out violently? And how can we even know if someone had it?
What Exactly Is CTE?
CTE is not your everyday concussion aftermath. It is a progressive, degenerative brain disease caused by repeated head injuries, the kind you get from rough contact sports, military service, or just too many unfortunate falls. Over time, these impacts seem to trigger the buildup of an abnormal protein in the brain called tau. This sticky substance does not just sit there quietly. It gradually spreads through the brain, messing with vital functions and causing serious, irreversible damage.The Symptoms
People with CTE do not wake up one morning knowing something is wrong. The symptoms can creep in slowly, subtle at first, then increasingly hard to ignore, leading to memory lapses, confusion, impulsive behaviour, unexplained aggression, mood swings, deepening depression and, in many tragic cases, suicidal thoughts.It is the sort of change that can feel like a personality transplant. Loved ones often report seeing someone “become a different person” over time.
Not Just a Pro Athlete Problem
For a long time, CTE seemed to be the unwanted souvenir of retired American football players. The sport's culture of full-body collisions made it the perfect storm for head trauma. But recent research is telling a more disturbing story. A 2023 study uncovered CTE in younger, amateur athletes, including teens as young as 17.Back to the Manhattan case. While the shooter’s note mentioned CTE, we still do not know whether he actually had it, let alone whether it influenced his behaviour. This brings up messy territory: should possible brain disease be considered in criminal responsibility? Can CTE be a mitigating factor in violent crime?
It is a grey zone. And until we develop reliable tools to diagnose CTE in the living, we are mostly left guessing.
What Can We Do?
CTE is a slow, silent thief, robbing people of their memory, emotions, and identity. And while scientists are racing to understand it better, prevention remains our best bet for now. That means:- Rethinking how we approach youth and professional sports
- Reducing repeated head trauma wherever possible
- Keeping an eye out for changes in behaviour following head injuries
What Is That One Thing That Makes Hepatitis So Dangerous?

Hepatitis is not nicknamed the “silent killer” for nothing. What makes it so dangerous is how symptomless it often is for years. It can quietly chip away at your liver without so much as a warning sign. By the time symptoms like fatigue, jaundice, or abdominal pain appear, significant harm may already have occurred. This eerie silence allows hepatitis to go undetected until it has done some serious damage.
Just Because You Cannot Hear It Does Not Mean It Is Not There
Dr Vikram Vora says that hepatitis is a major global health threat, killing over a million people each year. What is even more tragic? These deaths are, in his words, “largely preventable”. The villains in this tale, cirrhosis and liver cancer, often stem from untreated or undiagnosed hepatitis infections.
Prevention Helps
“The cornerstone of hepatitis control is prevention,” Dr Vora says. And the good news is that you have got some powerful tools at your disposal. “Vaccination, especially against Hepatitis B, is one of the most effective tools available,” he says, adding that infants, healthcare workers, and at-risk adults should be prioritised. Other prevention measures include safe injection practices, steering clear of needle-sharing, and ensuring blood transfusions are properly screened.
But danger often hides in plain sight. Dr Vora warns that something as seemingly harmless as getting a tattoo or piercing can carry lifelong consequences if done in an unregulated facility. His advice? “Choosing safe, licensed establishments is non-negotiable.”
Why You Should Not Wait for Symptoms
If there is one thing hepatitis is good at, it is staying undetected. That is why Dr Vora champions regular screening, especially if you have had medical procedures, blood transfusions, or close contact with someone infected. “Early diagnosis is a game-changer,” he says. Caught in time, hepatitis can be treated effectively, helping patients avoid severe liver disease or even make a full recovery.
A Diagnosis Is Not a Death Sentence
Dr Vora offers hope to those living with hepatitis. “With proper medical care and lifestyle adjustments, a healthy life is achievable,” he insists. That means ditching alcohol, sticking to a balanced diet, maintaining a healthy weight, and closely following medical advice. He also points out the mental and emotional toll a diagnosis can take. “Support from family, community, and healthcare providers can make a significant difference in outcomes.”
The Stigma That Silences
Perhaps just as damaging as the virus itself is the social stigma surrounding it. Dr Vora identifies this as a major hurdle in tackling hepatitis. “Fear of social exclusion keeps many from seeking help,” he explains. And that delay can cost lives. According to him, building a culture of empathy and understanding is critical. He encourages public health campaigns, education, and open dialogue as essential tools to dismantle this stigma.
Make Noise Against the Silence
In Dr Vora’s words, “Hepatitis may be silent, but it is not invincible.” Every little step, whether it is getting vaccinated, getting screened, or just talking about it, can chip away at the power hepatitis holds. Silence has cost too many lives already. Awareness can save them.
© 2024 Bennett, Coleman & Company Limited

