- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
World Lung Cancer Day 2025: Why You Should NOT Ignore A Recurring Cough? Danger Of Overlooking Early Symptoms

Credits: Health and me
Lung cancer remains one of the deadliest forms of cancer worldwide, accounting for nearly one in five cancer-related deaths each year. What makes this cancer especially dangerous is how silently it advances. Many people miss the early signs or ignore them, believing they’re just symptoms of a lingering cold, allergies, or an old infection but on World Lung Cancer Day—observed every year on August 1—the message is clear, early detection can mean the difference between life and death.
First observed in 2012, World Lung Cancer Day was launched by the Forum of International Respiratory Societies (FIRS) in partnership with patient advocacy groups. The aim? To break the silence surrounding lung cancer, correct widespread misconceptions, and push for better early detection and prevention.
Despite advances in medicine, lung cancer continues to slip under the radar. Many associate it solely with smoking, overlooking other contributors like air pollution, genetic factors, or secondhand smoke. Moreover, stigma often deters patients from seeking help early especially non-smokers who don’t consider themselves at risk.
While a chronic cough might seem harmless, dismissing it as seasonal or due to pollution, the reality is that it could be your body’s early warning system. Lung cancer rarely causes symptoms in its earliest stages, which is why seemingly minor signs like a persistent cough or subtle breathlessness deserve closer attention. By the time more severe symptoms—like coughing up blood, wheezing, or unexplained weight loss—appear, the disease may already be in an advanced stage.
What makes lung cancer particularly dangerous is its ability to remain silent until it’s too late. This is why awareness and early screening, especially in high-risk groups, are crucial. Smokers and former smokers, people exposed to secondhand smoke or environmental toxins, and those with a family history should be especially vigilant. Even if you don’t fall into these categories, don’t ignore your instincts. If something feels off—get it checked.
When a Cough Isn't 'Just a Cough'
Dr. Rakesh Pandit, Senior Consultant & Head of Internal Medicine at Aakash Healthcare, emphasizes that we often brush off coughs that last beyond a week or two, that’s a mistake. “A recurring cough is not always just a leftover from the flu or a seasonal allergy,” he says. “It could point to asthma, acid reflux, lung infections, tuberculosis—or even early-stage lung cancer.”
Dr. Pandit adds that if a cough persists for over eight weeks in adults (or four weeks in children), it needs medical attention. And it’s not just about coughs—symptoms like breathlessness, chest pain, coughing up blood, wheezing, or unexplained weight loss should be immediate red flags.
In fact, lung cancer is often detected late because the symptoms can be vague or mimic other conditions, a long-standing cough, shortness of breath, and fatigue—these aren’t always alarming on their own, but together, they can signal something serious.
Technological advances in low-dose CT scans now allow for earlier detection, improving survival rates significantly. The five-year survival rate for early-stage lung cancer can be as high as 60%, compared to just 6% in advanced stages. That’s a major difference—and it all starts with paying attention to symptoms that seem small.
Also, it’s not just about cancer. Chronic coughing and breathlessness can be early signs of other serious conditions like COPD, pulmonary fibrosis, or even heart failure. So addressing them isn’t just about cancer prevention—it’s about taking charge of your overall respiratory health.
What Missed Symptoms Can Lead To?
Dr. Sachin Kumar, Director of Pulmonology & Critical Care Medicine at Sakra World Hospital in Bengaluru, recalls a case that perfectly illustrates the cost of late detection. A 48-year-old man visited a doctor for back pain. Painkillers didn’t work. An MRI revealed cancer in the spine—further tests showed the primary cancer was in the lungs. It had already spread.
“This is how deceptive lung cancer can be,” Dr. Kumar explains. “Often, the first symptoms don’t even involve the lungs. That’s why awareness is key.”
Why Lung Cancer Is Not Just a Smoker’s Disease?
One of the most dangerous myths about lung cancer is that only smokers are at risk. While smoking remains the number one cause, non-smokers aren’t safe either. Dr. Debanti Banerjee, Consultant at HCG Cancer Center, Kolkata, warns that more young adults, women, and non-smokers are being diagnosed than ever before.
“Increasingly, we’re seeing lung cancer in non-smokers—possibly due to genetic predispositions, air pollution, and environmental toxins,” she explains. “People must understand that anyone can get lung cancer, and everyone needs to be vigilant about symptoms.”
She adds, “Lung cancer doesn’t always shout—it often whispers. Catching it in stage 1 or 2 can mean curative treatment. Catching it at stage 3 or 4? That’s a different story.”
What Are The Environmental Triggers and Everyday Risks?
In addition to smoking and secondhand smoke, prolonged exposure to pollution, dust, biomass fuel (like wood or coal used for cooking), and occupational hazards (like asbestos) significantly increase lung cancer risk. People living or working in such conditions often develop chronic coughs from continuous lung irritation. Unfortunately, this persistent irritation can mask the early signs of something more dangerous.
“Especially in urban environments, we’re breathing in harmful particles every day,” Dr. Pandit says. “If you’re in a high-risk environment, you can’t afford to ignore a chronic cough or delay a check-up.”
What You Can Do To Prevent And Early Diagnosis?
Here’s the thing—lung cancer caught early is often treatable but because early symptoms are vague, diagnosis is frequently delayed. The solution lies in being proactive.
- Don’t dismiss persistent symptoms, especially coughs, breathlessness, fatigue, or weight loss.
- Get screened if you’re high-risk, this includes smokers, ex-smokers, people over 50, or those with a family history.
- Avoid triggers, stay away from secondhand smoke, reduce exposure to pollution, and use protective gear if working in hazardous conditions.
- Vaccinate for infections like tuberculosis and influenza can damage lungs and increase vulnerability.
- Annual health checks should be part of your routine, not just something you do when you’re sick.
“Most causes of a recurring cough are treatable if caught early,” Dr. Pandit says. “That’s why a cough that won’t quit needs more than just home remedies or over-the-counter syrup. It needs medical evaluation.”
When detected in its early stages, non-small cell lung cancer (NSCLC)—the more common and slower-growing form—can often be removed surgically or treated with radiation and targeted therapies. But in later stages, treatment gets more complicated and outcomes become uncertain.
Dr. Banerjee sums it up best, “We need to move beyond fear and stigma. Early diagnosis isn’t about being alarmist—it’s about giving people a fighting chance.”
The theme of World Lung Cancer Day isn’t just about awareness. It’s a call to action- to listen to your body, to challenge the assumptions around who gets lung cancer and to make preventive health a priority. So, if you or someone you know has a cough that keeps coming back, don’t wait.
This Is Endometriosis, A Short Film On Debilitating Health Condition Wins BAFTA Award 2026, Know More

Credits: Instagram/ IMDb
This Is Endometriosis, a 2024 intimate, expressive film by Georgie Wileman and Matt Houghton won a BAFTA Award 2026 for Best British Short Film. This 19.27 minute long film shows how Georgie was robbed of her time due to endometriosis. The film sets in present-day narrative with memories from her past.
Endometriosis is a condition, that Georgie notes is often dismissed by many doctors as just "painful periods". However, her film portrays how truly disabling this medical condition. It is a condition in which cell similar to the lining of the uterus or the endometrium, grow outside the uterus. It affects 1 in 10 born with a uterus and could cause pain, often "worse than the last stages of child labour", notes thisiseno.com, the official website of the short film. Around 190 million people worldwide are impacted by the condition, however, what the film points out is how "dangerously underfunded, under researched and misinformed" doctors continue to remain despite the condition being so widespread.
Read: A Woman Lost Her Ovary To Endometriosis Surgery After Receiving An Ultimatum From Gynecologist
A Film That Documents Personal Struggle

Georgie, while accepting the award wore a symbolic blood-red gown. She said, "It was surreal and beautiful. Knowing how much this win would mean to the [endometriosis] community made it an emotional moment."
She points out that it is more than just a "painful period" and that "It is a full body disease. It important for people to understand the severity of the pain – it’s widely considered to be worse than childbirth." What is shocking is that it takes an average of eight to 10 years to be diagnosed.
She shares being "bed-bound for three months" when she was only 13. She said it first got "really bad" and she was not believed for long time. "It took me a long time to even believe myself. I was just so angry at my body for not working."
While she had been in and out of wheelchair, she was not formally diagnosed with endometriosis until she was 26, and then at 29, she was diagnosed with its 'sister disease' adenomyosis. She has undergone seven surgeries for her endometriosis and a hysterectomy for adenomyosis.
Read: Keltie Knight Was Gaslit By Doctors For Years Before Getting A Hysterectomy
In 2020, after years of feeling dismissed by doctors and watching her condition be misunderstood in the media, she decided she had had enough. That frustration pushed her to tell the story herself.
“It began as a photography project,” Wileman says. “And it meant a lot to people because, for the first time, they felt their experiences were being shown truthfully.”
But she soon realized that still images could only go so far. “There’s only so much a photograph can capture,” she adds.
Why Does It Take So Long For An Endometriosis Diagnosis?
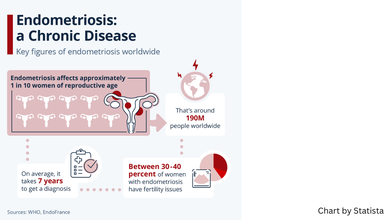
A study published in Obstetrics and Gynecology journal looks at the factors of what leads to such a delay in endometriosis diagnosis. Researchers identified that factors include normalization of menstrual pain, the diversity of symptoms, and a lack of training and prompt referrals among healthcare professionals lead to this delay.
At an individual level, the researchers found that many women struggled to tell the difference between “normal” period pain and something more serious. A common belief was that painful periods were simply part of being a woman and had to be endured. As a result, many relied on self-care measures and delayed seeking medical help, which likely pushed back the timeline for an endometriosis diagnosis.
On an interpersonal level, stigma played a powerful role. Menstrual problems were often seen as too private or embarrassing to talk about. At the same time, society’s tendency to normalize period pain meant that symptoms were minimized, both by those experiencing them and by people around them. This silence and normalization further contributed to delayed diagnoses.
Barriers also existed within the healthcare system itself. Some participants said their general practitioners dismissed their concerns or appeared unfamiliar with endometriosis. Healthcare professionals involved in the study acknowledged gaps in their own training and pointed out the lack of clear clinical guidelines for diagnosing the condition.
Doctors also noted that endometriosis symptoms can overlap with other disorders, making it harder to identify. Diagnosis is particularly challenging because there is no simple, noninvasive test that can confirm the condition with certainty. Delays in referrals were common. One contributing factor was the widespread belief that laparoscopic surgery is the only definitive way to diagnose endometriosis. Some healthcare providers also questioned how useful a formal diagnosis would be, which further slowed the process.
Dr Sophie Davenport, a doctor in England who conducted the research as part of her Master of Public Health dissertation, emphasized that the problem is layered and requires solutions at multiple levels.
“The key highlights of the data are that delays to diagnosis exist throughout the journey,” she explained. “We need to address these at different levels — from society understanding what ‘normal’ menstruation looks like and being open about menstrual problems, to clinicians being well educated, up to date on how endometriosis presents and diagnosed, and truly listening when patients say their periods aren’t normal.”
German Study Shows Squirrels May Be Harboring Mpox Virus
Credit: Canva
Squirrels could be natural hosts of the mpox virus (MPXV) -- that causes monkeypox disease -- according to a recent study by German researchers.
The team from the Helmholtz Institute for One Health (HIOH) identified the fire-footed rope squirrel (Funisciurus pyrropus) as a likely natural reservoir of the MPXV.
The study published in the journal Nature revealed that sooty mangabeys – a primate found in West Africa -- can contract mpox by eating infected squirrels. The disease may present mild lesions, but it can also cause more severe skin lesions or even be fatal.
"Identifying the animal sources of the virus and the exposure routes that lead to inter-species transmission are key steps towards understanding spillover mechanisms and developing effective prevention measures to mitigate the risk of transmission to humans," said Livia V. Patrono, one of the senior authors at HIOH.
Squirrels Suspected MPXV Hosts
While squirrels have long been suspected as potential reservoirs for MPXV, their role was confirmed after an investigation of an mpox outbreak among wild sooty mangabeys (Cercocebus atys) in Côte d'Ivoire.
During the outbreak, reported in early 2023, nearly one-third of the primates showed clinical signs of disease, and four infants died.
The team conducted viral genome sequencing and found that the infected monkeys carried a virus that was nearly identical to an MPXV strain identified in a fire-footed rope squirrel found dead 12 weeks earlier nearby.
Further, the team analyzed fecal samples from the mangabeys. A sample collected eight weeks before the outbreak's onset contained DNA from both the virus and the rope squirrel. This provided strong evidence of interspecies transmission at that moment.
Sooty mangabeys have been previously observed catching and eating fire-footed rope squirrels, which provide a direct route for the transmission of viruses.
Mpox Continues To Spread Globally
Although mpox is no longer a public health emergency, outbreaks of clade I and clade II strains of the mpox virus are continuing in many countries around the world, especially in Africa.
Last week, Madagascar announced the country's first death from mpox, a 3-year-old girl from the island nation’s eastern city of Toamasina.
The WHO has also confirmed that two cases of the recombinant strain – combining genomic elements of clades Ib and IIb of the monkeypox virus (MPXV) – have been identified to date: one in the United Kingdom and one in India.
Mpox is an infectious disease caused by the monkeypox virus (MPXV), part of the Orthopoxvirus genus, which also includes the virus that causes smallpox.
It spreads through close physical contact, including sexual contact, and in some cases through contaminated materials or respiratory droplets.
Symptoms typically include fever, swollen lymph nodes, rash, and/or lesions.
The global health body has also urged all countries to “remain alert to the possibility of MPXV genetic recombination.” It has also urged for continued epidemiological surveillance, sequencing, vaccination of at-risk groups, and infection prevention and control measures.
This AI Tool Predicts Women’s Breast Cancer Risk Up to Four Years
Credit: Canva
An international group of scientists has created an artificial intelligence tool that can estimate a woman’s likelihood of developing breast cancer within the next four years.
The AI tool, known as the BRAIx risk score, analyzes mammogram images to generate an individualized risk assessment and flag women who may face a higher chance of developing the disease.
It may not only show the current risk but also predict the future risk, enabling early detection and treatments for a better outcome.
According to the findings published in The Lancet Digital Health journal, nearly one in 10 women ranked in the top 2 percent of risk by the AI tool were diagnosed with breast cancer within four years. This was despite previously receiving a clear screening result.
“These risk scores enable future development of personalized screening pathways to transform population breast cancer screening and save lives,” said corresponding author Helen M. L. Frazer of the University of Melbourne.
Frazer noted that identifying women who appear cancer-free but carry very high risk -- comparable to those with inherited BRCA1 or BRCA2 mutations -- will unravel both hereditary and non-hereditary causes of breast cancer.
From one-size-fits-all screening to personalization
Breast cancer screening programs have significantly lowered mortality rates -- by roughly 40-50 percent among women aged 50 to 74. However, most screening systems still apply the same approach to all women, regardless of individual risk.
Traditional screening tools use genetics, breast density, and questionnaires to estimate breast cancer risk. On the other hand, new AI-based screening tools, such as BRAIx personalizes screening by gathering information already present in breast scan images to better identify who is at higher risk.
“Our results show that conventional mammographic density is a far weaker predictor of breast cancer risk than the BRAIx risk score, even for interval cancers,” the researchers said in the paper. Interval cancers are aggressive tumors diagnosed after a negative mammogram.
The BRAIx Tool
The BRAIx risk score was developed using mammograms from nearly 400,000 women. To prove its efficacy, the AI tool was tested on data from almost 96,000 women from Australia and then confirmed in an independent Swedish population of over 4,500 women.
The findings showed that:
- The BRAIx risk score estimated breast cancer risk more accurately than the traditional risk factors, such as breast density, country of birth, and even family history.
- For the top 2 percent of women with the highest BRAIx risk score, the probability of a cancer diagnosis within 4 years was 9.7 percent -- a risk level exceeding that typically seen in women with inherited BRCA1 or BRCA2 mutations.
The BRAIx risk score can:
- Make breast screening more personalised,
- Improve early cancer detection,
- Reduce false alarms,
- Save lives without increasing costs
Global Breast Cancer Burden
Breast cancer continues to be the most common cancer among women worldwide.
A recent study published in The Lancet Oncology journal predicted that the number of new cases of the deadly disease will reach more than 3.5 million globally in 2050 -- rising by a third from 2.3 million in 2023.
Annual deaths from the disease will also rise by 44 percent -- from around 764,000 to 1.4 million.
However, not smoking, getting sufficient physical activity, lowering red meat consumption, and having a healthy weight can help prevent over a quarter of healthy years lost to illness and premature death from breast cancer.
© 2024 Bennett, Coleman & Company Limited

