- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Can You Kill E. Coli By Cooking Your Food?
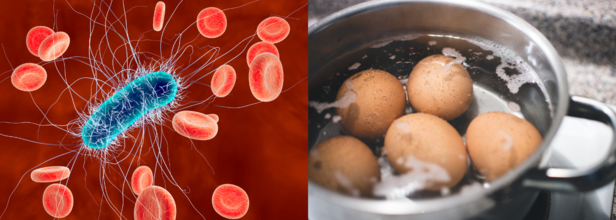
There have been many recent news of E.coli. Whether it is the McDonald's Quarter Producer incident or the E. Coli outbreak in the baby carrots and organic carrots. These recent E. Coli outbreaks have garnered media attention, raising concerns about the safety of food. Since outbreaks continue to cause deaths and illnesses, it is critical to understand ways to prevent infection.
The organic carrot recall was initiated by Grimmway Farms following the reporting of almost 40 instances across 18 states. One verified death and at least 15 hospitalized individuals were involved. Similarly, there was one fatality in Colorado and over 100 cases in 14 states from the McDonald's Quarter Pounder outbreak.
Heating and Cooking food can kill E.coli?
Food must be cooked to an internal temperature of at least 165°F, according to experts, in order to destroy E. coli. All food items, including meat and vegetables, fall under this category. To make sure the meal has reached the proper temperature and eradicate the bacteria, it's also critical to use a food thermometer.
Exact cooking instructions are necessary since certain strains of E. coli are heat-resistant and may withstand temperatures as high as 160°F.
Carrots that have been recalled should be thrown away or returned to the retailer, according to the Centers for Disease Control and Prevention. Additionally, the CDC advises using hot, soapy water or a dishwasher to clean any contaminated surfaces or objects.
E.coli and contamination
E. coli contamination in vegetables can occur in many different ways. It is also often linked to the bacteria residing in the intestines of animals.
During food processing, contamination happens if facilities lack proper hygiene or if workers fail to wash their hands thoroughly. Additionally, E. coli can spread through contaminated water, food, contact with animals, or infected individuals.
Experts emphasize the importance of clean hands, safe food preparation practices, and consuming only safe water to reduce the risk of infection.
Does Washing or Freezing Kill E. coli?
Washing vegetables can remove dirt and reduce some surface bacteria. However, washing vegetables cannot eliminate E. coli entirely.
Experts stress that no matter how thoroughly vegetables are washed, E. coli cannot be completely removed.
Can freezing food also freeze the bacteria and eventually kill them? Freezing foods does not kill E. coli bacteria, suggest experts. So what does freezing do? While freezing may slow bacterial growth, once the food thaws, the bacteria can resume multiplying. This highlights the need for proper cooking rather than relying on washing or freezing to ensure safety.
Why Are E. coli Outbreaks So Common?
The growing number of outbreaks reflects issues within an industrialized and processed food supply chain. Experts point out that as food passes through multiple processing stages, the chances of contamination increase. Each step in the production and distribution process presents an opportunity for harmful bacteria like E. coli or listeria to infiltrate.
In addition, growing antimicrobial resistance is making bacteria more resilient. The scale of modern food production and distribution also amplifies the impact of outbreaks, allowing contamination to spread far beyond localized areas. This has made it crucial to implement stricter testing and monitoring protocols in food facilities.
How Can You Stay Safe?
The recent outbreaks underscore the importance of vigilance in food safety practices. Consumers should dispose of any recalled items, thoroughly cook food to recommended temperatures, and maintain strict hygiene standards in food preparation. While industrial-scale food production offers convenience, it also necessitates greater attention to preventing contamination to protect public health.
'Eat Your Skin Care' What This Online Trend Really Mean

Credits: Canva
It started with a simple TikTok video, four large carrots shaved into ribbons, mixed with garlic, sesame oil, lime juice, coconut aminos, rice vinegar, and green onions. The resulting “crunchy and addictive” salad quickly racked up millions of views under the viral trend #EatYourRetinol. But is it just social media hype, or can what’s on your plate really show up on your face?
The trend encourages eating vitamin A-rich foods, like carrots, to support skin health from the inside out. “Skincare always starts within,” says Johanna Salazar, registered dietitian nutritionist and founder of Healing Nutrition, as noted by Martha Stewart. But experts urge a balanced view: while diet can support your skin, it’s not a magic replacement for topical care.
What’s in the Carrot Salad That’s Good for Your Skin?
The base of the salad, carrots, are packed with beta-carotene, a precursor to vitamin A, known for boosting skin cell turnover and promoting a radiant complexion. Pairing it with a fat, like sesame oil, helps your body absorb the fat-soluble vitamin. Lime juice adds vitamin C, key for collagen production, while garlic and green onion offer prebiotics that support gut health, which in turn impacts skin health.
Sesame seeds sprinkled on top bring in vitamin E and fiber, which contribute to skin hydration and a healthy glow.
“It’s a nice mix of ingredients that all play small but beneficial roles in skin support,” says Salazar.
Dermatologists Weigh In: Not a Cure-All
Lauren Kole, M.D., associate professor of dermatology at the University of Alabama at Birmingham, appreciates the effort to eat for skin health—but with a word of caution.
“Deficiencies in certain vitamins and minerals can negatively affect the hair, skin, and nails,” she says. “But eating an excess doesn’t necessarily make your skin better.”
Kole points out that while beta-carotene from carrots is helpful, it's not strong enough to replace prescription retinol or other topical treatments for conditions like acne or hyperpigmentation. “Diet is not a substitute for proper skin care,” she emphasizes.
Beyond Carrots: Other Skin-Loving Foods
Experts agree that eating for your skin isn’t just about one salad. A variety of fruits, vegetables, and healthy fats are essential. Salazar and Kole both recommend incorporating:
Dark-colored fruits like berries and red grapes, which are high in antioxidants that fight oxidative skin damage.
Leafy greens such as spinach, kale, and chard, which are rich in vitamin C and help with collagen production.
Vegetables like broccoli, mushrooms, and cauliflower, which support healthy pigmentation and skin repair.
Healthy fats including avocados, walnuts, flaxseeds, and omega-3-rich foods to reduce inflammation and maintain skin moisture.
According to Kole, diets like the Mediterranean diet—rich in plant-based foods and good fats, have shown potential skin benefits in clinical settings.
Don’t Ditch Your Skincare Just Yet
While the “Eat Your Retinol” movement has its heart in the right place, Salazar and Kole stress that no food trend should replace professional skincare or personalized advice.
Lizzy Davis, Ph.D., a dietitian and assistant professor at UAB, advises people to approach such trends with balance.
“Cooking carrots, for example, doesn’t reduce their skin-friendly fiber,” she notes. “It can actually make them easier to digest and still beneficial.”
Davis also warns against over-relying on TikTok or Instagram for skincare advice. “Talk to your doctor or a registered dietitian,” she says. “Social media is convenient, but it can’t give you a plan tailored to your needs.”
Not Just Cigarettes, But Your Food Too Could Increase Your Chance Of Lung Cancer

Credits: Canva
We already know that ultraprocessed foods are linked to obesity, heart disease, and diabetes. But now, a new study published in the medical journal Thorax suggests a concerning addition to that list, lung cancer.
According to researchers, people who consume the highest amounts of ultraprocessed foods may face a 41% higher risk of being diagnosed with lung cancer, compared to those who eat the least, even when accounting for smoking and other known risk factors.
What Are Ultraprocessed Foods?
Ultraprocessed foods are industrial formulations made largely or entirely from substances not typically used in home cooking.
According to the Food and Agriculture Organization of the United Nations, these include artificial colorings, preservatives, emulsifiers, and chemically altered fats, sugars, or salts.
Common examples? Think sodas, chips, packaged soups, processed meats like chicken nuggets and cold cuts, instant noodles, diet soft drinks, and even some ice creams.
These additives enhance taste, shelf-life, and appearance, but at what cost?
What Does The Study Reveal About Food Choices and Lung Cancer Risk
Researchers behind the Thorax study analyzed data from over 100,000 adults who participated in the U.S. National Health and Nutrition Examination Survey. Each person filled out a detailed dietary questionnaire, which researchers then compared with medical records to track lung cancer diagnoses over time.
On average, people reported eating nearly three servings of ultraprocessed food a day, most commonly lunch meats and soft drinks.
Despite adjusting for smoking habits, age, sex, and other lifestyle factors, the study found a clear association between higher ultraprocessed food intake and increased lung cancer risk, particularly among people who had never smoked.
“This strongly suggests that these foods may contribute to lung cancer risk in ways beyond just smoking,” said Dr. David Katz, a specialist in preventive and lifestyle medicine and founder of the nonprofit True Health Initiative, as reported by CNN. Though not involved in the study, Katz called the findings “concerning and credible.”
Why Would Food Be Linked to Lung Cancer?
Experts believe multiple mechanisms could be behind the link.
“Industrial processing alters the food matrix,” the study authors explained, “which affects how nutrients are absorbed and may produce harmful contaminants.”
One such contaminant is acrolein. It is a toxic compound found not only in cigarette smoke, but also produced when cooking oils or fats are heated to high temperatures.
The U.S. Centers for Disease Control and Prevention (CDC) lists acrolein as a substance that can inflame and damage lung tissue.
Packaging may also be a problem. Plastics and synthetic materials used in food storage can leach chemicals, some of which are known or suspected carcinogens.
Add to that the fact that ultraprocessed foods are often low in omega-3 fatty acids, said Dr. Tom Brenna, professor of nutrition and chemistry at the University of Texas at Austin, as reported by CNN.
“Omega-3s spoil easily, so manufacturers tend to remove them to increase shelf life,” he explained. That’s unfortunate, because omega-3s help reduce inflammation, a key process in cancer development.
Smoking Isn’t the Only Risk Factor
Lung cancer remains one of the most commonly diagnosed cancers globally, with 2.4 million new cases in 2022, according to the World Health Organization. While smoking remains the leading risk factor, experts now believe diet and environmental exposures also play a role.
Dr. Fang Fang Zhang, a professor at Tufts University’s Friedman School of Nutrition Science and Policy, as reported by CNN, noted that while the study adjusted for smoking, the adjustment may not have been thorough enough. “Smoking needs to be measured more precisely, by cigarettes per day or years of exposure,” she said. Still, she found the link stronger in non-smokers, which makes the data all the more compelling.
What You Can Do: Eat More Whole Foods
The takeaway? While more research is needed to understand the exact biological mechanisms at play, the connection between ultraprocessed foods and cancer risk can no longer be ignored.
According to Dr. Katz, the solution lies in going back to basics. “Health and diet quality improve when people eat mostly whole, unprocessed foods,” he said, including vegetables, fruits, beans, whole grains, nuts, seeds, and other plant-based ingredients.
Dr. Zhang agrees. “Avoid foods with long ingredient lists full of unfamiliar chemicals,” she advised. “Focus on meals made from whole or minimally processed ingredients whenever possible.”
From PMS to Postpartum, Heart to Hormones: Why Fish Oil is the Ultimate Health Elixir for Every Woman at Every Stage

Fish oil is a star supplement loaded with omega-3 fatty acids like EPA and DHA. It offers a spectrum of vital benefits for women’s health. These extend beyond general well-being to support heart, brain and joint function, especially in areas of concern specific to women.
Fish oil, rich in omega-3s, addresses unique needs across all stages of a woman’s life. From adolescence through motherhood to menopause, fish oil supports cardiovascular, hormonal, mental and reproductive health.
A Boost for the Heart
Fish oil plays a major role in promoting heart health. According to Dr Mohit Bhatia, it helps lower triglyceride levels, a risk factor for cardiovascular disease, and improves blood flow, making it essential for proper cardiovascular function. He adds that it also slows the progression of cardiovascular disease.
Karan Khurana, a health expert at WishNew Wellness, concurs, saying that omega-3s in fish oil reduce triglycerides, lower blood pressure, and decrease arterial inflammation. This is particularly vital for post-menopausal women, who face a greater risk of heart disease. Regular consumption of fish oil, he says, can even lower the risk of heart attacks and strokes.
Hormones, Menstrual Cycles and PMS
Women facing bloating, mood swings or cramps may find some relief with fish oil. Dr Bhatia says that some evidence-based research suggests fish oil can help alleviate PMS and menstrual pain, thanks to its anti-inflammatory properties.
Khurana elaborates that omega-3s may regulate menstrual cycles and reduce cramps by lowering prostaglandin levels, which contribute to pain and inflammation. He adds that fish oil can ease common PMS symptoms such as bloating and breast tenderness.
Pregnancy, Postpartum and a Baby’s Brain
The benefits of fish oil carry into pregnancy too. Dr Bhatia points out the importance of DHA during this stage, saying it is vital for healthy foetal brain and eye development. It may also reduce the risk of preterm birth and help alleviate postpartum depression.
Khurana backs this up, pointing out that fish oil supplementation not only supports cognitive function in babies but also helps mothers manage postpartum depression. It plays a role in maintaining the mother’s brain health during and after pregnancy.
Bones, Joints and the Menopause Years
Post-menopause, bone health becomes a serious concern for many women. Dr Bhatia says that the anti-inflammatory properties of fish oil can contribute to bone health, potentially reducing the risk of osteoporosis.
Khurana adds that omega-3s enhance calcium absorption and support bone density. Fish oil, he explains, helps reduce inflammation linked to joint pain, promoting stronger bones and better mobility for older women.
Better Moods and Sharper Minds
Women are more likely than men to experience anxiety and depression, and fish oil might just help. Dr Bhatia explains that these fatty acids play a role in elevating mood and supporting brain function, potentially mitigating cognitive decline.
Khurana agrees, saying omega-3s support cognitive health and reduce the risk of dementia later in life. Fish oil, he says, may alleviate symptoms of depression and anxiety, contributing to overall mental well-being.
Your Skin Will Thank You Too
Dr Bhatia does not touch on it, but Khurana dives into skin benefits. He says that fish oil improves hydration, reduces wrinkles, and protects against UV damage. Its anti-inflammatory effects can ease conditions like eczema, making skin look and feel healthier.
Final Thoughts Before You Pop That Capsule
Dr Bhatia emphasises that while fish oil is a powerful supplement, it should complement a balanced diet and healthy lifestyle. He strongly recommends consulting a healthcare professional before starting, especially for those on medication or with existing conditions.
Khurana suggests aiming for 250–500 mg of combined EPA and DHA daily, either through fatty fish like salmon or through supplements. Fish oil, he concludes, is a holistic powerhouse that can help women thrive at every stage of life.
© 2024 Bennett, Coleman & Company Limited

