- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
With The FDA Banning Food Dyes, Here's A Natural Alternative To Use

Credits: Canva
As the U.S. Food and Drug Administration (FDA) moves to ban certain synthetic food dyes, consumers are turning their attention to natural options. One vibrant contender is blue spirulina, an eye-catching, plant-based pigment that has found its way into smoothies, candies, beverages, and even gourmet salad dressings.
The History and Science Of The Color
Blue spirulina is an extract of green spirulina, a type of blue-green algae classified as cyanobacteria. Its intense color comes from phycocyanin, a potent antioxidant not found in land plants. While spirulina itself has been consumed in various cultures for centuries, the blue variety gained FDA approval as a food color additive in 2013 for use in candy and gum.
Approval has since expanded to include non-alcoholic drinks, condiments, dairy alternatives, seasoning mixes, salad dressings, and certain low-alcohol beverages.
NASA once studied spirulina as a space food supplement, thanks to its nutrient density and antioxidant properties. However, dietitians caution against assuming blue spirulina is a nutritional powerhouse in large doses. “There are some benefits, but the hype is largely due to its Instagram-worthy color,” says Caroline Thomason, a Washington, D.C.-based dietitian, as reported by USA Today.
Safety and Regulation
Any color additive sold in the U.S. must undergo FDA evaluation before hitting the market. The agency’s approval indicates that the benefits outweigh potential drawbacks, but does not guarantee absolute safety. Blue spirulina is classified as a color additive exempt from certification, meaning each batch does not require individual testing before sale.
This exemption raises quality concerns. Harvard Health notes that products can vary in purity, and some may not contain the promised levels of spirulina. Contamination is another risk. Between 2018 and 2020, three blue-green algae products—two supplements and one beverage—were recalled for containing unsafe levels of microcystins, natural toxins that can damage the liver and kidneys.
“It’s generally safe in small amounts, though the quality can vary between brands,” says Thomason. “Choose a reputable source to avoid contamination with heavy metals or toxins, which can happen in poorly regulated algae products.”
Nutritional Value and Limits
While whole spirulina offers a rich profile of protein, vitamins, and minerals, the blue extract contains fewer nutrients. Still, it delivers antioxidants that may help reduce inflammation, similar to those in blueberries or red cabbage.
Adding blue spirulina to foods and drinks can be a fun way to experiment with color and flavor. However, Thomason warns that treating it like a miracle superfood can backfire. “As with any trendy health ingredient, going overboard might lead to nutrient gaps or an unhealthy fixation,” she says.
With the FDA’s crackdown on synthetic dyes, blue spirulina stands out as a visually stunning, naturally derived option for coloring foods.
If you plan to incorporate it into your meals, do so occasionally, and after consulting an expert and source it from trusted brands.
This Naturally Occurring Molecule May Have Ozempic-like Benefits Without The Side Effects

Credits: Canva
What if we tell you that a naturally occurring molecule can do wonders like Ozempic, but without the side effects. Hard to believe, isn't it? However, Stanford Medicine researchers have found a molecule that acts similar to semaglutide, by suppressing appetite and reducing body weight. The trials on animals have also shown that it worked without some of the drug's side effects, including nausea, constipation and significant loss of muscle mass.
The paper was published on March 5 in Nature, and led by Laetitia Coassolo, PhD, Kartin Svensson, assistant professor of pathology.
What Is This Naturally Occurring Molecule?
This newly discovered molecule is BRP. This acts, though, in a separate pathway, but has similar metabolic effects. It can activate different neurons in the brain and offer a more targeted approach to body weight reduction.
Stanford Medicine's release quoted Svensson, PhD, who explained, "the receptors targeted by semaglutide are found in the brain but also in the gut, pancreas and other tissues. That’s why Ozempic has widespread effects including slowing the movement of food through the digestive tract and lowering blood sugar levels. In contrast, BRP appears to act specifically in the hypothalamus, which controls appetite and metabolism.”
Svensson has also co-founded a company to launch clinical trials of the molecule in humans in the near future.
How Was The Study Conducted?
This study would not have been possible without the help of AI, notes the release. Researchers used AI to sift through dozens of proteins in a group called prohormones.
Prohormones are molecules that do not do anything on their own at first. They become active only after being cut into smaller pieces, called peptides, by other proteins. Some of these peptides then act as hormones, controlling important functions in the body, such as energy use in the brain and other organs.
Each prohormone can be cut in different ways, producing many possible peptides. Among these, only a few actually work as hormones, while most are just byproducts of protein breakdown. Traditional lab methods make it hard to find the useful peptides in this mix.
The researchers focused on an enzyme called prohormone convertase 1/3, which cuts prohormones at specific points in the amino acid chain. This enzyme has been linked to obesity in humans. One of the peptides it produces is GLP-1, which helps control appetite and blood sugar levels.
The drug semaglutide works by mimicking GLP-1. The team wanted to see if there were other peptides from this enzyme that also play a role in energy metabolism.
To do this, they created a computer program called Peptide Predictor. Instead of manually sorting through proteins, the program scanned all 20,000 human protein-coding genes to find likely cutting sites for prohormone convertase 1/3. They focused only on proteins that are secreted outside the cell, a key feature of hormones, and that had at least four cutting sites. This narrowed the list to 373 prohormones.
The program predicted that these could produce 2,683 unique peptides. The team then looked at those most likely to act in the brain and tested 100 of them, including GLP-1, on lab-grown nerve cells.
GLP-1 increased cell activity about three times compared to normal cells, as expected. But one small peptide, just 12 amino acids long, increased activity tenfold. They named it BRP, based on the name of its parent protein BRINP2.
What Did The Result Reveal?
Tests on lean mice and minipigs showed promising results. An injection of BRP before feeding reduced food intake by up to 50% over the next hour. In obese mice, daily injections for two weeks led to an average weight loss of 3 grams, mostly fat, while untreated mice gained about 3 grams. The treated mice also had better blood sugar control.
Importantly, BRP did not change the animals’ movement, water intake, anxiety levels, or digestion. It also works through different brain and body pathways than GLP-1 or semaglutide, which could make it useful for people who do not respond well to those drugs.
What's Next?
Researchers now want to find the exact cell receptors BRP binds to and figure out how to make its effects last longer in the body. If it proves safe and effective in humans, BRP could offer a new option for treating obesity.
The study was a collaboration between scientists at the University of California, Berkeley, the University of Minnesota, and the University of British Columbia.
What A Single High-Fat Meal Can Do To Your Brain In Just Hours

Credits: Freepik
We already know a greasy meal isn’t great for the heart. But science is now showing that it can impact your brain far faster than you might expect — in as little as four hours. A new study from the University of South Wales reveals that just one high-fat meal can temporarily reduce your brain’s ability to regulate blood flow, a crucial function that protects against strokes and cognitive decline. And the effects aren’t subtle. Even in healthy men, researchers detected measurable changes in both blood vessel flexibility and brain circulation changes that could spell trouble over time.
Researchers recruited 41 healthy men- 20 in their twenties and 21 in their sixties. None smoked, had heart disease, or took medications that could skew the results. The team gave them a calorie-dense, high-fat drink made from heavy cream, chocolate syrup, sugar, and powdered milk. Nicknamed the “brain bomb,” the shake contained 1,362 calories and 130 grams of fat, a fat load similar to a fast-food burger, fries, and milkshake combo.
To trigger post-prandial hyperlipidaemia, a temporary spike in blood fats that happens after a fatty meal. Four hours later, scientists tested the men’s artery health and brain blood flow control using ultrasound and other measures.
Blood Fats Skyrocket, Arteries Struggle
In just four hours, triglyceride levels surged: from 0.88 to 2.26 mmol/L in younger men, and from 1.39 to 2.92 mmol/L in older men. Artery flexibility — measured by flow-mediated dilation (FMD) — dropped as well. Younger men saw a 0.7 percentage point decrease, while older men’s FMD dropped by 1.2 points.
Though these numbers may sound small, they represent real changes in how blood vessels respond to increased flow — a key marker of vascular health. Less flexible arteries mean blood pressure fluctuations become harder to manage, and circulation to sensitive organs like the brain can falter.
The Brain’s Shock Absorbers Go Offline
Your brain relies on a mechanism called dynamic cerebral autoregulation — think of it as built-in shock absorbers that keep blood flow steady despite everyday changes in blood pressure, like when you stand up quickly.
In this study, that system faltered just hours after the high-fat meal. The pulsatility index — a measure of stiffness in brain vessels — increased, signaling that blood vessels were less able to cushion those changes. Older men showed the most pronounced effects: stiffer brain vessels, lower baseline blood flow, and a weaker ability to adapt when pressure shifted.
These changes don’t mean a stroke is imminent after one meal, but they suggest that even short-lived dips in brain blood flow regulation can stress an already vulnerable vascular system — particularly with age.
Why This Is Important For Overall Wellness?
The men in the study were healthy and relatively fit, meaning the negative effects could be even stronger in people with high blood pressure, diabetes, or sedentary lifestyles. For stroke survivors, the implications are especially important. The brain’s blood flow regulation is often already compromised after a stroke, and even small disruptions could hinder recovery.
The researchers didn’t follow participants to see how long the effects lasted, but the takeaway is clear: your brain reacts quickly to what you eat, and those reactions aren’t always benign.
Why The Type of Fat and Fat Distribution is Critical?
Dietary fat isn’t inherently bad. It’s an essential nutrient, providing energy, helping absorb fat-soluble vitamins, and supporting cell structure. The problem lies in saturated fat — the kind found in butter, fatty cuts of meat, and many processed foods.
Saturated fats are linked to stiffer arteries and reduced nitric oxide production — a molecule that helps blood vessels relax and widen. When you load your system with a sudden burst of saturated fat, blood vessels constrict, and the brain’s ability to keep a steady flow of oxygen and nutrients takes a hit.
In contrast, unsaturated fats from foods like oily fish, nuts, seeds, and olive oil are associated with better heart and brain health over time. What’s still unknown is whether a single meal high in these healthier fats affects brain blood flow in the same way as saturated fat.
Why Older, Ageing Brains Are More Vulnerable?
Aging naturally brings stiffer blood vessels and slower circulatory responses. This means older adults have less “reserve” when sudden stressors — like a high-fat meal — challenge the system. In the study, older men experienced about 10% greater impairment in brain blood flow regulation compared to younger men.
For older adults, especially those with cardiovascular risk factors, even temporary dips in brain blood flow could contribute to cumulative damage over years, raising the risk of dementia and stroke.
How Much Saturated Fat Is Too Much?
In the US and UK, dietary guidelines suggest limiting saturated fat to less than 10% of daily calories — roughly 20 grams for women and 30 grams for men. The “brain bomb” used in the study had more than four times that limit in one sitting.
It’s worth remembering that many people exceed these limits regularly, especially with weekend takeout, pub lunches, or fast-food splurges. And because blood fat levels can remain elevated for hours, we may spend much of the day in a post-meal state that quietly strains our vascular systems.
How To Protect Your Brain?
The lesson isn’t to fear every indulgence, but to recognize that the brain responds to dietary choices in real time. Here are practical ways to reduce risk:
- Limit high-saturated-fat meals, especially if you’re older or have cardiovascular risk factors.
- Swap in unsaturated fats — choose olive oil over butter, fish over fatty cuts of red meat.
- Balance the meal — pairing fats with fiber-rich vegetables and whole grains can slow the absorption of fats into the bloodstream.
- Stay active — exercise improves blood vessel function and brain circulation, helping buffer the effects of occasional indulgences.
A single high-fat meal may not seem like much, but it can make your blood vessels including those in your brain less responsive within hours. The effect is stronger with age and may be amplified by existing health conditions.
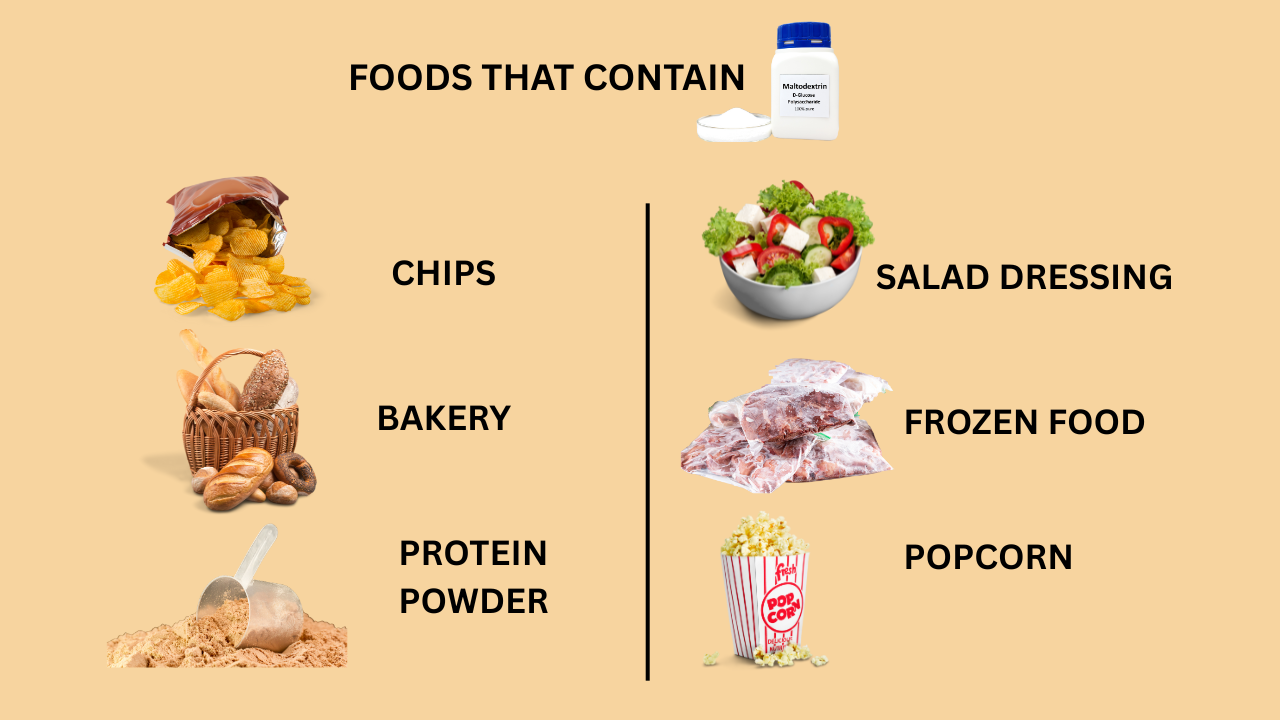
THIS Ingredient Is Even Worse Than Sugar, And You Are Consuming It Everyday

Credits: Canva
"Sugar has a bittersweet reputation when it comes to health," notes Harvard Health Publishing's piece on how too much sugar can lead to the greatest threats to cardiovascular disease. However, there exists something else that could be worse than sugar. Maltodextrin.
While part of a balanced diet, and it can provide carbohydrates and energy, especially those who need an instant increase in blood sugar levels, however, its consumption must be regulated and balanced with fiber and protein.
What Exactly Is Maltodextrin?
It is a white powder, which is made from corn, rice, potato starch, or wheat. While it is plant based, it is highly processed.
How is it extracted? The starch is first cooked and then is added with acids or enzymes like heat-stable bacterial alpha-amylase, which breaks it down further. As a result, a white powder, which is also water soluble, has a neutral taste, is created. If one has to draw a close parallel, it could be corn syrup solids. However, what makes it different from corn syrup solids is the sugar content.
Both of them undergo hydrolysis, which is a chemical process that involves addition of water to further help with the breakdown. As per the Handbook of Food Preservation, after hydrolysis, corn syrup solids are at least 20% sugar, while maltodextrin is less than 20% sugar.
What Makes It So Dangerous Then?
Dietician Lavleen Kaur, in her Instagram reel mentioned that maltodextrin is found in most processed foods. This means, if we are consuming processed food, we are continuously consuming maltodextrin, even if it has a low sugar percentage as compared to corn syrup, the frequency of the consumption could result in high blood sugar.
"This silent culprit, often found in processed foods, can spike your blood sugar levels even higher than table sugar. Prioritize your health by cutting down on ultra-processed foods and make informed choices," said Kaur.
Is It Safe To Consume?
As per the Food and Drug Administration (FDA), maltodextrin has been approved as a safe food additive. It is also included in the nutritional value of food as part of the total carbohydrate count.
The Dietary Guidelines for Americans suggest that carbohydrates must make up 45% to 65% of one's overall calories. Most of these must be complex carbohydrates, which are rich in fiber, rather than simple carbohydrates, which can raise blood sugar in a go.
Maltodextrin has a high glycemic index (GI) value, which means it can cause a spike in your blood sugar. However, only if consumed in small amounts, it is safe to use. If someone has diabetes, one should be mindful of how much they consume, and also speak to the doctor before making any change with their diets.
Why Is Maltodextrin Added In Foods?
The main purpose of this ingredient is to increase the volume and the solubility of the product. It also helps extend its shelf life. Furthermore, it increases sweetness, prevents melting and reduces nutrient losses.
Health Issues And Maltodextrin
Maltodextrin due to its high GI value, could be unsafe for those struggling with diabetes. Issues like inflammatory bowel diseases and ulcerative colitis, Crohn's disease, and an increased risk to infections like E.coli and Salmonella could be also linked to maltodextrin. The US FDA researchers found that it is because maltodextrin can alter gut bacteria, impair mucus release, and suppress the growth of good bacteria in gut.
© 2024 Bennett, Coleman & Company Limited

