- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Statin Muscle Pain: Scientists Finally Explain What That Is
Credits: iStock
Statin pain and what is it, scientists finally explain. A study by University of British Columbia finally explained what statin muscle pain is and what triggers it. Statins have long been a cornerstone of cardiovascular care. By lowering “bad” LDL cholesterol, these drugs have significantly reduced the risk of heart attacks and strokes for millions worldwide. Yet, for a notable number of users, statins come with an uncomfortable trade-off: muscle pain, weakness, and, in rare cases, severe muscle breakdown that can even lead to kidney failure.
For years, doctors have known that these side effects occur, but not why. Now, a new study offers a detailed answer.
Researchers from the University of British Columbia (UBC), in collaboration with the University of Wisconsin–Madison, have identified the molecular trigger behind statin-related muscle problems. Their findings, published in Nature Communications, could pave the way for safer cholesterol-lowering drugs in the future.
Why Do Statins Affect Muscles?
Muscle-related side effects are among the most common reasons people stop taking statins. Symptoms range from mild soreness and fatigue to rhabdomyolysis, a rare but dangerous condition where muscle tissue breaks down and releases proteins that can damage the kidneys.
Until now, the biological mechanism behind this damage remained unclear. The new research zooms in on what happens inside muscle cells when statins are present.
Statin: The Role of Calcium in Muscle Cells
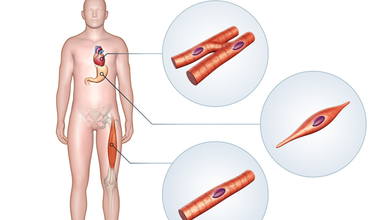
To understand the problem, researchers focused on a protein called the ryanodine receptor (RyR1), which plays a critical role in muscle contraction. RyR1 acts as a gatekeeper, controlling the release of calcium inside muscle cells. Calcium is essential for muscle movement, but only in carefully regulated amounts.
Using cryo-electron microscopy, an advanced imaging technique that allows scientists to view proteins in near-atomic detail—the team observed how statins interact with this receptor.
What they found was striking: when statins bind to RyR1, they force the channel to remain open. This leads to a constant leak of calcium into the muscle cell. Over time, this calcium overload becomes toxic, damaging muscle tissue and explaining the pain, weakness, and, in severe cases, muscle breakdown seen in some patients.
A Closer Look at How Statins Bind
The study examined atorvastatin, one of the most widely prescribed statins globally. However, researchers suggest the same mechanism may apply across the statin class.
They discovered that statins bind to RyR1 in an unusual three-part formation. One statin molecule attaches while the channel is closed, priming it to open. Two additional molecules then bind, forcing the channel fully open and keeping it that way. This sustained opening is what causes the harmful calcium leak.
This detailed binding pattern offers the clearest explanation yet for statin-induced muscle side effects.
What This Means for Future Treatments
While severe muscle injury affects only a small fraction of the more than 200 million statin users worldwide, milder symptoms are far more common and often lead patients to discontinue treatment. This is a serious concern, as stopping statins increases cardiovascular risk.
The new findings provide a potential solution. By modifying the parts of statin molecules that interact with RyR1—while preserving their cholesterol-lowering effects—scientists may be able to develop safer statins with fewer muscle-related side effects.
Why This Study Matters
Beyond statins, the research highlights how advanced imaging technologies are transforming medicine. By visualizing drug–protein interactions at near-atomic resolution, scientists can move from observing side effects to understanding their exact cause.
For patients, this could mean a future where statins remain just as effective—but far easier on the muscles, improving long-term adherence and overall quality of life.
Red Cross Faces Blood Shortage, Asks For Immediate Donations

Credits: iStock
The American Red Cross reported a severe shortage of blood that has affected Tri-City area hospitals. In the last month, there has been a 35% drop in blood supply. The 'Code Red' blood shortage in Washington created a critical situation with hospitals requesting for blood. The drop is also noted due to the winter weather that has affected donation drive.
Red Cross Faces Blood Shortage: How Does Weather Influence Blood Bank?
Reports note that during the winter season, blood supply becomes challenging, though its demand may increase due to illness and severe weather conditions. However, the same factors lead to fewer donation drives that leads to critical shortage. According to Red Cross reports, more than 550 blood drives have been canceled since January 21. This has resulted in over 15,000 uncollected blood and platelet donation.
The shortage has severely impacted the availability of blood for trauma victims, cancer patients and those who require emergency surgeries. During such situation, volunteer donors play an essential role.
Diana Heilman, supervisor at the Kennewick Red Cross Fixed Site, said, "octors may face difficult decisions during a blood shortage, such as who can safely receive the products and treatments, and they will potentially have to wait because there simply isn't enough blood available."
Red Cross Faces Blood Shortage: What Is Affected?
- The Kennewick Red Cross identified a dire need of Type O blood, both positive and negative
- A negative
- B negative
- Platelets
Type O is a universal donor, while Type O positive is the most commonly transfused blood type. A negative blood type is found in only 6% of the population, and B negative is less than 2%.
Red Cross also announced a $20 e-gift card for those who donate between January 26 to February 28, as incentive.
Read: Japan Races To Develop World’s First Artificial Blood, Trials To Begin
Red Cross Faces Blood Shortage: Who Can Donate?
Must be in good general health, weigh at least 110 pounds, and be 17 years old (or 16 with parental consent where permitted)
- Valid identification is required, along with a brief health screening before donation
- Minimum hemoglobin levels: 12.5 g/dL for women and 13.0 g/dL for men
- Most medications are allowed, but blood thinners and some antiviral drugs may disqualify donors
- The full donation visit takes about one hour; the actual blood draw lasts 8–10 minutes
- Whole blood can be donated every 56 days; Power Red donations every 112 days
- Platelets are in high demand due to their five-day shelf life and essential role in cancer, trauma, and surgical care
- Donors with O negative, O positive, A negative, and B negative blood types are encouraged to consider Power Red donations
- Officials urge eligible donors to schedule appointments promptly to help address ongoing blood shortages impacting patient care
Red Cross Faces Blood Shortage: Frequently Asked Questions
Read: Thinking of Donating Blood? A Doctor Answers All Your Doubts
Can Women Donate Blood During Their Period?
This is one of the most common concerns, especially among first-time female donors. According to Dr. Sangeeta Pathak, Director and Head of Transfusion Medicine at Max Super Speciality Hospital, Saket, who spoke to Health and Me, as per the Drugs and Cosmetics Act, women are advised not to donate during their menstruation, particularly during the 4-5 days of active bleeding. However, they are completely eligible to donate at any other time of the month if they are in good health.
Can You Donate Blood While Recovering From An Illness?
Health is key when it comes to blood donation. “A person should be completely healthy and free from fever or illness at the time of donation,” says Dr. Pathak. Moreover, certain medications can lead to deferral, and there is a comprehensive list maintained under the Drugs and Cosmetics Act. So if you’re on a prescribed course, it’s best to consult a doctor or the blood bank before donating.
Can You Donate Blood If You Have A Tattoo Or Piercing?
Yes. If you’ve recently had a tattoo or body piercing, you’ll need to wait 12 months before you can donate blood. This is a precautionary step to ensure there’s no risk of transmitting infections.
Nipah Virus Outbreak In India: Is Thailand Carrying Out COVID 19 Like Screenings At Airports?

Credits: PR Thai Government (X)
Nipah virus outbreak in India triggered airport screenings of travelers. Many reports claim that passengers are being checked in similar ways as they were during the COVID-19 virus spread.
Nipah Virus Outbreak In India: Are Travelers Passing Through A COVID-19 Like Check?
In Thailand, health officials have announced: "passenger screening points for arrival from affected areas" on its official X account, along with the information on airports to start "enhanced cleaning of shared areas to ensure the safety of both passengers and staff".
On January 27, Thailand's Tourism Ministry announced that they had "not detected any cases of Nipah virus, affirming that strict screening and preventive measures are in place at all international airports to safeguard public health and reassure tourists."
Nipah Virus Outbreak In India: What Does The COVID-Like Screening Include?
The screening includes:
- Temperature checks
- Health history
- Travel history
- Epidemiological monitoring
Anyone suspected of having Nipah will be immediately isolated and referred to public health system "in accordance with International Health Regulations".
Read: Australia Is Monitoring Nipah Virus Outbreak In India
In Thailand, the screenings are happening in these following airports:
- Phuket International Airport
- Bangkok's Suvarnabhumi Airport
- Don Mueang Airport
Nipah Virus Outbreak In India: Why Is Thailand Gearing Up For COVID-19 Like Checks?
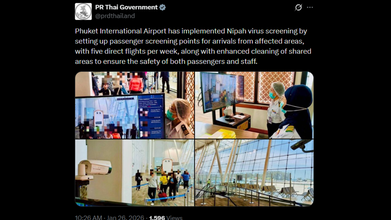
Two cases of Nipah virus were detected in India's eastern state of West Bengal, in Kolkata. While other airports have also geared up for travel checks, Thailand is taking it to a next level with COVID-19 like checks. The reason is due to a huge number of international travel form Kolkata to Bangkok and Phuket. Many reports claim that Thailand is a premier international destination for travelers from Kolkata, due to its proximity, affordability, and being a visa-free detination. There are roughly 55 weekly direct flights from Netaji Subhash Chandra Bose International Airport to Bangkok and Phuket.
Nipah Virus Outbreak In India: What Is It?
As per the World Health Organization (WHO), Nipah virus infection is a zoonotic illness that is transmitted to people from animals, and can also be transmitted through contaminated food or directly from person to person.
In infected people, it causes a range of illnesses from asymptomatic (subclinical) infection to acute respiratory illness and fatal encephalitis. The virus can also cause severe disease in animals such as pigs, resulting in significant economic losses for farmers.
Read: Nipah Virus Outbreak In India: How Did It All Begin?
Although Nipah virus has caused only a few known outbreaks in Asia, it infects a wide range of animals and causes severe disease and death in people.
Nipah virus is infectious and can spread from animals like bats and pigs to humans through bodily fluids or contaminated food. It can also pass between people through close contact, especially in caregiving settings. While it can spread via respiratory droplets in enclosed spaces, it is not considered highly airborne and usually requires close, prolonged contact for transmission. Common routes include direct exposure to infected animals or their fluids, consuming contaminated fruits or date palm sap, and contact with bodily fluids such as saliva, urine, or blood from an infected person.
Nipah Virus Symptoms
- Fever
- Headache
- Breathing difficulties
- Cough and sore throat
- Diarrhea
- Vomiting
- Muscle pain and severe weakness
Thar Desert Bacteria Is Infecting People in Himalayas, Study Finds

Credit: Canva
Bacteria from the Thar desert is being transported by wind to the Eastern Himalayas and causing respiratory and skin diseases in locals, according to a Science of the Total Environment study.
Researchers from Bose Institute found that powerful dust storms filled with disease-causing bacteria can travel hundreds of kilometers, crossing densely populated and polluted Indo-Gangetic Plain before finally settling over Himalayan hilltops, where they are affecting local populations and ecosystems.
The scientists noted: "In addition to respiratory and skin diseases due to the transported pathogens, vertical uplift injects locally sourced pathogens into high-altitude atmosphere, where they mix with long-range travellers arriving from afar. Together, they reshape the bacterial community floating above the Himalayas, contributing to gastrointestinal infections as well."
Why Is This A Concern?
The Himalayan hill-top atmosphere is widely considered beneficial for human health. However, after analyzing air samples for two years, the scientists found a clear link between desert-origin dust and bacterial shifts in the Himalayan atmosphere.These changes were driven by horizontal wind patterns that carry particles across vast distances, combined with rising air pollution from lower elevations.
Riddled with airborne bacteria, including pathogens that can affect overall physical health, this air can increase vulnerability in people living in colder regions, who are already at a high risk of developing conditions related to the weather such as hypoxia (a condition where tissues don't get enough oxygen, often causing confusion, rapid heart rate, shortness of breath and bluish skin)
“About 80 percent of the total Himalayan bacterial population is due to long-range transport via horizontal and vertical movement of atmosphere, causing about 60 percent perturbation in Himalayan bacterial diversity,” the researchers said.
Cold weather and excessive exposure to airborne bacteria also increases disease risks by weakening immune responses, causing blood vessels to constrict and promoting close indoor confinement, which accelerates the spread of bacteria and viruses.
Some common conditions include respiratory infections (pneumonia, bronchitis), cardiovascular strain (heart attacks, strokes) and bacterial infections like Strep throat.
READ MORE: AI Detects More Breast Cancer Cases in Landmark Swedish Study
Antibiotic Resistance: An Rising Threat
This comes days after experts warned that one child in India dies every nine minutes from an infection caused by antibiotic-resistant bacteria, as it becomes one of the top 10 global public health threats.Dr HB Veena Kumari of the Department of Neuromicrobiology, National Institute of Mental Health and Neurosciences, claims: "The Covid-19 pandemic has significantly contributed to rising antimicrobial resistance. The World Health Organisation projects that 10 million deaths will occur annually by 2025."
According to the National Foundation for Infectious Diseases, antibiotic resistance occurs when bacteria in the body learns to withstand and remain unaffected by the medicines (antibiotics) meant to kill them.
In such cases, doctors have to switch to different antibiotics, but these backup medicines might not work as well or might cause more side effects. Additionally, infections may also worsen over time as bacteria can become resistant to all available drugs.
Alarmingly is that these tough, drug-resistant bacteria can spread from one person to another, both in hospitals and at home.
According to Dr TS Balganesh, Gangagen Biotechnologies, nearly 36 percent of haemodialysis patients die from fatal infections, which is second only to cardiovascular diseases as a cause of death.
He tells Deccan Herald: "The risk for infective endocarditis in haemodialysis patients is approximately 18 times higher than in the general population and up to 58 percent of these episodes are caused by a bacteria named 'S aureus', with an in-hospital mortality of more than 50 percent."
© 2024 Bennett, Coleman & Company Limited

