- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
10 Signs You May Have A Parasite
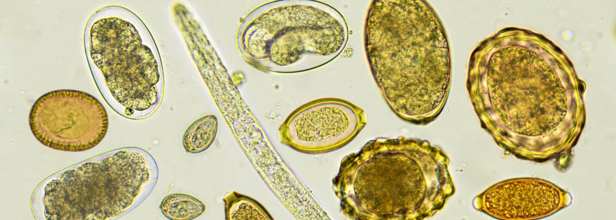
Credits: Canva
A parasite is an organism that lives on or in the host organism. It also gets its food from or at the expense of its host. Parasitic infections can be unpleasant as they sound. They are much more common than we think. In fact, in most cases, these infections are the reason behind a lot of health issues that people suffer from. It could be a parasitic infection for all you know that affects your physical, mental, and digestive health.
Types of Parasites
- Roundworms
- Tapeworms
- Pinworms
- Whipworms
- Hookworms
- Lice
- Giardia
- Mosquitos
- Bedbugs
- Scabies
Parasites can come in many shape and sizes. Once inside your body it can make you feel hungry, because it feeds on the nourishment from your body. Whereas there are some that feeds off your red blood cells, and cause you anemia. Since it is all the things we feel from within, many times, people do not even realise that they are suffering from a parasitic infection and that it could lad to chronic health problems. It is also important to look out for causes, signs, and symptoms that indicate a parasitic infection to start treatment as soon as possible.
How Can You Get Intestinal Parasites?
- If you live in or visit an area which is known to have parasites
- During an international travel
- If you consume contaminated or unclean food or water
- If you eat uncooked meats
- If you maintain a poor hygiene
- If you have a weakened immune system or HIV or AIDS
- If you work closely with animals, or handle soil or other waste material
Once you are infected with a parasite, it is easy to pass it along to others. If you have a parasite and you do not wash your hands after using the restroom, you can easily pass microscopic parasite eggs onto anything that you touch. It could also come from the common places like the bathroom door handle, a salt shaker, your phone, or just anything that you touch.
How Would You Know If You Have A Parasite?
Here are 10 signs that will help you identify if you have a parasitic infection in your body.
1. Digestive Issues
Unexplained constipation, diarrhea, gas, bloating, heartburn, or nausea could signal a parasitic infection. Intestinal parasites settle in the gastrointestinal (GI) tract, triggering immune responses that cause a range of symptoms. Many of these are often mistaken for Irritable Bowel Syndrome (IBS). Unfortunately, routine lab tests may not always detect parasites, and more sensitive diagnostics like the GI-MAP test are needed for accurate identification.
2. Chronic Fatigue & Exhaustion
Parasites can drain your body's nutrients, leading to persistent fatigue, mood changes, headaches, and even memory issues. Some, like Giardia, can cause chronic fatigue syndrome, making it difficult for your body to absorb essential nutrients like iron and B12. This deficiency results in unexplained lethargy, which can disrupt daily life.
3. Skin Problems
Mysterious rashes, hives, eczema, or rosacea may be linked to parasites. When parasites trigger an immune response, your body produces more Immunoglobulin E (IgE) antibodies, leading to allergic reactions that manifest as stubborn skin issues. If over-the-counter treatments aren’t helping, a parasitic infection might be the hidden cause.
4. Muscle & Joint Pain
Some parasites release inflammatory toxins that can settle in muscles and joints, causing pain and stiffness. A specific parasite, Trichinella, found in undercooked meat, can migrate to muscles, leading to persistent aches that don’t respond to usual treatments.
5. Anemia
Certain parasites consume red blood cells or cause internal bleeding, resulting in iron deficiency anemia. This leads to fatigue, weakness, and pale skin, as your body struggles to function with reduced oxygen levels.
6. Constant Hunger or Loss of Appetite
Feeling hungry all the time, despite eating regularly, could indicate a tapeworm or other parasite feeding off your nutrients. On the other hand, nausea and gas can suppress appetite, causing unintentional weight loss.
7. Itching
Some parasites burrow under the skin or lay eggs, leading to intense itching. Pinworms, for example, cause persistent itching around the anus, especially at night. The immune system's response to parasites can also trigger allergic reactions, worsening the irritation.
8. Teeth Grinding (Bruxism)
Grinding your teeth at night could be linked to toxins released by parasites. These toxins interfere with neurotransmitters, triggering anxiety, nervousness, and involuntary teeth grinding while sleeping.
9. Insomnia & Sleep Disturbances
Parasites are often more active at night, causing physical discomfort and disrupting sleep. If you're experiencing frequent wake-ups or unexplained restlessness, an underlying parasitic infection might be the reason.
10. Bloating & Gas
Parasites like Giardia can lead to excessive gas and bloating, making your stomach feel constantly distended. The severity of symptoms varies, and while some people experience major discomfort, others may have a parasitic infection without any noticeable symptoms.
Heart Attack: How Symptoms Differ In Men And Women

Credit: American Heart Association
Heart attack is the world's number one killer, yet its symptoms differ for both men and women, leading to varied outcomes.
A heart attack typically occurs when cholesterol plaque builds inside the walls of arteries and causes damage to the major blood vessels.
While men typically develop plaque in the largest arteries that supply blood to the heart, in women, it accumulates in the heart’s smallest blood vessels, known as the microvasculature.
A study published today in Circulation: Cardiovascular Imaging, an American Heart Association journal, showed that women report less artery-clogging plaque. Yet, it did not protect them from heart disease compared to men.
The study showed that women faced increased heart risk at lower levels of plaque compared to men. For total plaque burden, women’s risk began to rise at 20 percent plaque burden, while men’s risk started at 28 percent.
The increasing plaque levels led to a sharper risk for women than for men.
How Heart Attack Symptoms Differ Between Men And Women
According to global studies, women are more likely than men to die from a heart attack. The major reason is the late onset of symptoms of a heart attack in women.
During a heart attack, men are likely to experience sweating, pain in the chest, arms, and legs, and shortness of breath.
While the experiences are common among women, they also tend to suffer a combination of less-recognized symptoms such as nausea, indigestion, fatigue, dizziness, and pain in the neck, jaw, throat, abdomen, or back.
The obvious chest discomfort is also sometimes absent during heart attacks in women.
Other common reasons for heart attacks in women include:
- High testosterone levels before menopause
- Hypertension during menopause
- Autoimmune diseases such as rheumatoid arthritis
- Stress and depression
Can Heart Attacks Be Prevented?
Cardiovascular diseases are mostly preventable by targeting traditional risk factors common to both women and men, which include obesity, smoking, diabetes, high blood pressure, family history and metabolic syndrome -- the co-existence of high blood pressure, obesity, and high glucose and triglyceride levels.
The American Heart Association also advises at least 150 minutes a week of moderate-intensity aerobic activity (such as brisk walking) or 75 minutes of vigorous activity (such as jogging), or a combination of both.
Include fruits, vegetables, lean proteins, whole grains, low-fat or fat-free dairy, nuts, and seeds in your diet.
Limit processed foods, added sugars, sodium, and alcohol.
Sleep Terrors In Children: Warning Signs And What Parents Should Do

Credit: Canva
Seeing your child suddenly screaming at night, with wide eyes and thrashing limbs, can be deeply unsettling. However, remaining calm and focusing on safety is crucial for parents during the sleep terror episodes, said health experts.
Sleep terrors, also known as night terrors, are episodes of sudden fear, screaming, or intense distress that occur during sleep.
The condition is more common in children, especially between the ages of 3 and 8 years, as their sleep patterns are still maturing.
Unlike nightmares, which usually happen during dreaming (REM sleep) and are often remembered, sleep terrors occur during deep non-REM sleep.
Dr Preeti Singh, Senior Consultant, Clinical Psychology, Max Super Speciality Hospital, Dwarka told HealthandMe, that while it may be frightening to witness, especially for parents, sleep terrors themselves are usually not harmful.
Although most kids outgrow this naturally, if the episodes are violent or very frequent, consult a specialist, added Dr Sudhir Kumar, a neurologist at Apollo Hospitals, Hyderabad.
What Are Sleep Terrors
During sleep terror, the child may sit up abruptly, shout, appear frightened, sweat, breathe rapidly, and be difficult to console. In most cases, they do not recall the episode the next morning.
Sleep terrors typically occur in the first third of the night, during deep sleep (slow-wave sleep). They are considered a type of parasomnia, meaning an unusual behavior during sleep.
Dr Kumar, in a post on social media platform X, explained that unlike a bad dream, a sleep terror happens in deep sleep (Stage N3).
It is characterized by abrupt sitting up/screaming, with physical signs that include a fast heart rate, sweating, and dilated pupils.
"It is 11 PM. Your child suddenly sits up, screams at the top of their lungs, and looks terrified. They are not responding to you, and they seem to be looking right through you. This is likely a sleep terror (night terror), a common NREM sleep parasomnia in children aged 3-12,” said Dr Kumar, popularly known as the Hyderabad doctor, on X.
The expert noted that the children are unlikely to recognize the parents and be "consoled" during the episodes.
What Factors Trigger Sleep Terrors
- Sleep deprivation or irregular sleep schedules
- Fever or illness
- Emotional stress or anxiety
- Major life changes or trauma
- Family history of parasomnias
- Certain medications
For children, sleep terrors are often developmental and tend to reduce as the nervous system matures, Dr Singh told HealthanMe.
How Can Parents Respond?
Parents often feel alarmed during a sleep terror episode, but the key is to remain calm, the experts said. They said during an episode:
- Do not try to fully wake the child, as this may increase confusion and agitation.
- Gently ensure the child is safe and cannot injure themselves.
- Speak softly and reassuringly, even if they do not respond.
- Wait for the episode to pass, which usually happens within a few minutes.
Other preventive measures include:
- Maintaining a consistent bedtime routine
- Ensuring the child gets adequate sleep
- Reducing screen time before bed
- Managing stress during the day
- Creating a calm and secure sleep environment
How To Manage
Most children do not require medical treatment, as sleep terrors usually resolve on their own with age. Treatment is considered when episodes are frequent, severe, cause injury, or significantly disrupt family life.
However, addressing sleep deprivation, treating any underlying medical conditions (e.g., sleep apnea), counseling or stress management strategies can help.
Why Hypertension Is Soaring Stroke Risk, Death In Young Indians

Credit: Canva
Hypertension or high blood pressure, a major risk for stroke, is preventable and treatable. Yet it accounts for about 14 per cent of cases of stroke among young adults aged below 45 years.
High blood pressure can be defined as the increasing pressure in blood vessels marked as 140/90 mmHg or higher.
Uncontrolled hypertension can burst or block arteries that supply blood and oxygen to the brain, causing a stroke.
A recent study by the Indian Council of Medical Research (ICMR) found that hypertension (74.5 percent) was the most common risk factor for stroke and related deaths (27.8 percent) and significant disability (about 30 per cent) across India.
“Blood vessel walls can be damaged through uncontrolled high blood pressure, making them prone to blockage or rupture. The good news is that hypertension is preventable through regular monitoring, reduced intake of salt, exercise stress control, and medication when required,” Dr. Rajul Aggarwal, Director - Neurology, Sri Balaji Action Medical Institute, Delhi, told HealthandMe.
How Does Hypertension Increase The Risk Of Stroke?
Chronic high pressure forces the brain to compensate, leading to vessel remodeling, narrowing, and eventually rupture or clotting.
The ICMR study reported that ischemic stroke accounted for 60 percent of cases.
The experts explained that in the case of ischemic stroke, high blood pressure damages artery walls, fostering plaque buildup (atherosclerosis) or allowing clots to form and block blood flow to the brain.
On the other hand, with hemorrhagic Stroke, constant strain caused by high blood pressure weakens artery walls, causing them to burst or leak blood into the brain. This can result in severe damage or life-threatening emergencies.
“When blood pressure stays high for years, it slowly strains the blood vessels -- nothing dramatic at first, which is why people ignore it. The arteries become stiff and fragile, sometimes narrowing, sometimes tearing,” Dr. Gunjan Shah, Interventional Cardiologist, Narayana Hospital, Ahmedabad, told HealthandMe.
"This makes clots or bleeding in the brain more likely, leading to ischemic or hemorrhagic stroke, even in people who otherwise feel perfectly fit and busy with daily life," Dr. Shah added.
Importance of the ‘Golden Hour’ In Stroke Care
In stroke-related cases, the golden hour -- referred to as the critical first 60 minutes after symptom onset -- is very much critical. Early medical treatment during the window can prevent death risk as well as boost health outcomes.
However, the ICMR study, published in the International Journal of Stroke, showed that just 20 percent of patients arrived in the hospital after 24 hours of the onset of symptoms.
Dr. Aggarwal said treatment within the first 60 minutes can significantly reduce the brain damage and improve survival as well.
“In a stroke, time moves very differently. Brain cells begin getting damaged within minutes when blood flow stops. If someone reaches the hospital quickly -- within the golden hour -- we have a real chance to restore circulation and limit disability. Recognising symptoms early and not waiting at home can truly change how well a person recovers,” added Dr Shah.
How Can Hypertension And Stroke Be Prevented?
Hypertension is a modifiable disease, and the risks can be reduced by:
- Cutting down and managing stress
- Checking blood pressure regularly
- Treating high blood pressure
- Eating less salt
- Staying active
- Managing stress
- Sleeping properly
- Avoiding tobacco
Dr Shah said that many young patients delay care because they feel fine, but taking medicines on time and correcting lifestyle early can prevent serious problems later.
© 2024 Bennett, Coleman & Company Limited

