- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
5 Reasons To Get Regular STI Testing If You’re 'Sexually Active'

Sexual health remains one of the most vital yet overlooked aspects of public health across the world. Despite increasing awareness, sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) continue to be surrounded by stigma, misinformation, and delayed intervention.
The terms STI and STD are often used interchangeably, but the medical nuances between them are critical. STIs (sexually transmitted infections) refer to the presence of an infection—caused by bacteria, viruses, or parasites—that is transmitted through sexual contact. This stage may not always result in symptoms.
According to Dr. Shelly (Mittal) Mahajan, Lab Director & Clinical Lead at Mahajan Imaging Labs in India, “There’s a fundamental need to educate individuals on the difference between STIs and STDs—not just for medical accuracy, but also for proactive health behavior.”
“An infection occurs when a pathogen enters the body and begins to multiply,” explains Dr. Mahajan. “But not all infections cause symptoms or result in disease immediately. This is the stage when someone is most likely to be unaware they’re even infected.”
In contrast, STDs (sexually transmitted diseases) represent the point where the infection leads to recognizable symptoms or causes damage to the body. Think of STIs as the initial silent stage and STDs as the symptomatic or advanced phase.
Take chlamydia, for example. “Initially, it can be entirely asymptomatic and go unnoticed,” Dr. Mahajan notes. “But left untreated, it can progress to pelvic inflammatory disease (PID), which is an STD. PID can lead to complications like chronic pelvic pain, infertility, and ectopic pregnancy.”
This difference between infection and disease progression is crucial because it highlights the role of early testing and intervention. Many individuals may carry and transmit infections unknowingly, which reinforces the need for routine screening—even in the absence of symptoms.
Why Routine Testing Is Important When You Are Sexually Active?
One of the most concerning aspects of STIs is how quietly they can progress. Asymptomatic carriers often delay testing, inadvertently spreading infections and risking long-term health effects. The Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) both emphasize regular STI screening for anyone who is sexually active, especially individuals with multiple partners or those engaging in unprotected sex.
“Many people wait until symptoms appear, but by then, damage could already be done,” says Dr. Mahajan. “Regular testing is a form of self-care and a responsibility to your partners.”
If left untreated, STIs can result in:
- Chronic pelvic pain
- Infertility in both men and women
- Ectopic pregnancies
- Increased vulnerability to HIV and other infections
- Neurological and organ damage in severe cases like late-stage syphilis
Common STIs
Chlamydia
A bacterial infection that is often symptom-free, especially in women. When symptoms appear, they may include unusual discharge, painful urination, or pain during intercourse. If not treated promptly, it can cause PID in women and epididymitis in men—both affecting fertility.
Gonorrhea
Also known as “the clap,” gonorrhea can cause genital pain, discharge, and inflammation. If untreated, it may lead to systemic infection known as Disseminated Gonococcal Infection (DGI), which includes joint pain, fever, and skin sores.
Syphilis
An infection that evolves in stages. “The early stages involve painless sores, which are often ignored,” Dr. Mahajan warns. As it advances, it causes rashes, flu-like symptoms, and eventually can lead to brain and organ damage. Syphilis remains curable with early antibiotic treatment.
HIV (Human Immunodeficiency Virus)
HIV weakens the immune system and can remain asymptomatic for years before progressing to AIDS. “Early detection and treatment with antiretroviral therapy (ART) can dramatically change the trajectory of the condition,” says Dr. Mahajan. “It transforms HIV into a manageable chronic condition.”
Ways To Prevent Sexually Transmitted Diseases
When it comes to preventing STIs, knowledge and consistency are key.
1. Use Protection Consistently
“Condoms are still one of the most effective barriers against many STIs,” affirms Dr. Mahajan. Used correctly, they can significantly reduce transmission risks.
2. Get Tested Regularly
Even if you're in a monogamous relationship or show no symptoms, routine testing should be a part of your health checklist. Testing intervals may vary depending on your risk profile, but annual screenings are a good starting point.
3. Have Open Conversations with Partners
Sexual health should never be a taboo topic in relationships. “Discussing STI history and protection methods isn’t just responsible—it builds trust,” says Dr. Mahajan.
4. Vaccination Matters
Vaccines are available for some STIs like HPV and Hepatitis B. Check with your healthcare provider about vaccination schedules and eligibility.
STIs are not a moral failing. They are medical conditions that require attention, not judgment. Unfortunately, stigma remains a barrier, often preventing individuals from seeking timely care.
“People are often embarrassed or fearful to even talk about STIs,” says Dr. Mahajan. “This silence is dangerous. We need to normalize these conversations to promote better health outcomes.”
From cultural taboos to misinformation, stigma around STIs can perpetuate cycles of neglect and misinformation. Public health campaigns, inclusive sexual education, and non-judgmental medical care are essential steps in changing this narrative.
Understanding the distinction between STIs and STDs is more than academic—it’s empowering. As Dr. Mahajan emphasizes, “With awareness, testing, treatment, and open dialogue, most STIs are manageable, many are curable, and all are preventable.”
What Are The Physical Symptoms Of Stress?
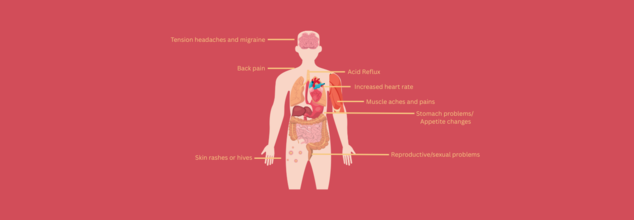
Credits: Canva
Stress is your body’s natural response to challenges or demands. It’s a physical and mental reaction triggered by anything from daily responsibilities—like work, school, or family—to major life changes, such as illness, loss of a loved one, or a traumatic event. In small doses, stress can be beneficial. It helps you stay alert and focused and can even improve performance in some situations. This is because your body releases hormones like adrenaline and cortisol, which increase your heart rate, speed up your breathing, and prepare your muscles to respond quickly.
But when the stress response continues for too long or happens too often, it can become harmful. Chronic stress—when your body stays in a prolonged state of alert—can lead to long-term health problems.
How Stress Affects the Body
Central Nervous and Endocrine Systems
Your brain’s hypothalamus triggers the “fight or flight” response, telling your adrenal glands to release stress hormones. These hormones prepare your body to deal with threats. Ideally, once the threat is gone, hormone levels drop, and your body returns to normal. But if stress persists, this system stays activated. Over time, this can lead to anxiety, depression, irritability, headaches, and sleep disturbances. Chronic stress can also push people toward unhealthy habits like overeating, skipping meals, smoking, or using alcohol or drugs.
Respiratory and Cardiovascular Systems
Stress causes your breathing to speed up in order to quickly move oxygen throughout your body. If you have a breathing condition like asthma, this can worsen symptoms. Your heart also pumps faster, and your blood pressure rises. Over time, this extra workload increases your risk of high blood pressure, stroke, and heart disease.
Digestive System
Under stress, your liver produces extra glucose for energy. But if your body can’t regulate this surge, it can raise your risk of developing type 2 diabetes. Stress may also lead to stomach discomfort, nausea, acid reflux, or bowel issues such as diarrhea or constipation. While stress doesn’t directly cause ulcers, it can aggravate them.
Muscular System
Muscles tense up during stress to protect you from injury. Normally, they relax when the stress passes. But with ongoing stress, they stay tight. This can lead to headaches, back pain, and general body aches. Chronic muscle tension can also make you less likely to stay active, which can contribute to more discomfort and reliance on painkillers.
Sexual and Reproductive Systems
Stress can reduce sex drive in both men and women. In men, long-term stress can lower testosterone, affect sperm production, and cause erectile dysfunction. In women, it may lead to irregular, painful, or heavier periods and intensify menopause symptoms.
Immune System
Initially, stress boosts your immune system. But over time, it weakens your body’s defenses, making you more susceptible to colds, flu, and other infections. It can also slow down your recovery from illness or injury.
Which COVID-19 Variants Are Going Around The World In 2025?

Credits: Canva
When the COVID-19 pandemic hit the world, many studies and experts predicted that COVID-19 is here to stay. While the extent to with it would affect an individual's health may have gone down, the virus, in fact, has continued to stay, and mutated. Almost like a viral fever, every year, there is a new variant and the virus seems to make head lines all over again.
This year, COVID-10 made a come back when Singapore and Hong Kong reported a spike in its cases. As per the Ministry of Health, the spike in the cases is attributed to the new variant, which is said to be on the loose - LF.7 and NB.1.8.1. These two are descendants of the JN.1 variant.
COVID-19 Variants In 2025
As per the World Health Organization, as of May 23, 2025, the following COVID-19 variants are currently circulating and are under monitoring:
KP.3 - This is a sub lineage of the JN.1, which comes from the Omicron variant. It evolved from the JN.1 and has a very similar structure too, with only two changes in spike as compared to JN.1. It also causes gastrointestinal symptoms like nausea, vomiting, etc. apart from the other common COVID-19 symptoms.
KP.3.1.1 - As per the Centers for Disease Control and Prevention (CDC), KP.3.1.1, of the Omicron family, is the predominant SARS-CoV-2 variant, which is an offshoot from within the KP.3 family.
LB.1 - It is said to be a spinoff of JN.1 with additional mutation, which sets it apart from the other strains.
XEC - As per the CDC and WHO, it is a highly transmissible coronavirus subvariant that comes from the SARS-CoV-2 Omicron strain. What makes it different is its hybrid result from a merger and rearrangement of two pre-existing COVID subvariants: Omicron sub-lineages KP.3.3, and KS.1.1.
LP.8.1 - This is also a variant of SARS-CoV-2, a descendant of the JN.1 lineage, with notable mutation in the spike protein. However, its ability to spread is not fully understood. Although, the resistance of LP.8.1 is similar to that of XEC and KP.3.1.1 across all serum groups tested. These results suggest that while LP.8.1 has lower pseudovirus infectivity than JN.1, its immune resistance is comparable to XEC and KP.3.1.1.
NB.1.8.1 - This is the new mutation causing a spike in cases in China and is part of the Omicron family. However, this means that the current vaccines and immunity from the recent infections should provide some protection against it. This is a highly contagious mutated variant, which has been detected in several US states and have prompted concerns among medical and health professionals.
As per Nebraska Medicine, this variant makes up for the 73% of cases in the US.
ALSO READ: Covid Cases Surge In Singapore: What Do We Know About The New Variant On The Loose?
Which Variant Is Active In India?
Like most of the active variants from the WHO list of variants under monitoring (VUM) comes from JN.1, the case of India is no different.
The current active variant in India is JN.1, which is a subvariant of the Omicron, which has evolved from the BA.2.86 variant, also known as Pirola. This was first identified in Luxembourg in 2023. Since then, it has spread to other parts of the world, including India.
It is more transmissible than the previous variants, the reason being, its specific mutations in its spike protein. These mutations help the variant to bind to humans easily.
As per the Indian SARS-CoV-2 Genomics Consortium (NSACOG) data, India has reported cases of LF.7 and NB.1.8.1 cases, both of which are descendants of JN.1.
The other common variants in India, apart from the JN.1, which comprises of the 53% of samples which have been tested as of now, are BA.2 with 26% cases, and other Omicron sub lineages at 20% of cases.
IVF: What Is The Right Age To Start, How Many Times You Can Try And What To Expect
Credits: Health and me
Starting a family is a very personal experience—one that comes with optimism, questions, and sometimes, unforeseen setbacks. If you've been the one asking, "Is it too early or too late for IVF?" or "How many attempts can we make before we give up?"—you're not the only one. In Vitro Fertilization (IVF) has brought new possibilities to couples fighting infertility, but timing, expectations, and psychological preparation are vital. From biological clocks to financial realities, understanding when and how to begin IVF can make all the difference.
An IVF expert helps break down all the elements involved in conceiving via In Vitro Fertilization (IVF). As assisted reproduction becomes more prominent and mainstream, it's important to consider IVF from a broader picture than the mere clinical procedure. Whether one is successful or not with IVF depends on an intricate mix of biology, preparedness, and timing—factors that are very personal and specific to each and every individual and couple.
Why Timing in IVF Matters?
Timing in IVF is not so much a matter of calendar or age—it is a question of coordinating physical health, emotional readiness, and financial capability.
Biologically, age plays a pivotal role, particularly for women. A woman is born with all the eggs she will ever possess, and as she gets older, both the number and quality of these eggs decrease. This natural decline generally becomes appreciable after age 30 and more sharply after 35. In Dr. Pavithra M, Fertility Consultant at Garbhagudi IVF Centre's opinion, "The best time for a woman to opt for IVF is between her early to mid-30s. Fertility starts decreasing gradually from age 30, and after 35, the possibilities fall sharply." Conversely, men have a more insidious decline in fertility, with sperm quality usually decreasing after 40–45 years of age. Reduced motility, sperm density, and elevated DNA fragmentation can impact IVF success when paternal age is increased. While men can theoretically sire children at older ages, older paternal age has been linked to greater conception and pregnancy complications.
IVF initiated at an earlier reproductive age offers higher chances of success per cycle, requires fewer attempts, and can be more cost-effective. “Success rates are significantly higher in younger women,” says Dr. Pavithra. “That’s why early intervention is key.”
How Many Times Can Couples Try IVF?
IVF is not a single-process affair, and the number of attempts necessary can range widely. Although there is no theoretical limit to the number of cycles an individual or couple may attempt, professionals insist on a realistic strategy.
"Usually, if the patient has failed to conceive after three to four IVF cycles, it might not be worth continuing," says Dr. Pavithra. She adds that repeated failure of cycles deserve a more in-depth examination of protocols, lifestyle influences, and possible underlying pathology.
For others, it is in the first or second try. For others, it may be six or more. But the process is physically and psychologically draining. Many insurance policies don't entirely cover fertility treatment, so couples are left with significant out-of-pocket costs. Aside from cost, the bodily and psychological price of hormone shots, egg retrieval, and successive failures is significant.
Clinically, once three to six cycles have failed, physicians usually re-evaluate everything right from the embryo quality to uterine status and even immunological variables. "Every failed cycle is also a diagnostic," Dr. Pavithra says. "We know more about the reproductive health of the couple after each attempt."
Waiting Between IVF Cycles: How Long Should You Pause?
The mind and body require time to recuperate between IVF cycles. Experts normally advise a break of one to three months between tries, depending on how the person has coped physically and emotionally.
"The waiting time between cycles is very important for emotional recuperation," says Dr. Pavithra. "It also provides time to analyze embryo growth from the previous cycle, make necessary changes to protocols, and mentally prepare for the next step."
In some situations—particularly with diminished ovarian reserve or age-related drop)—physicians might start another cycle in as brief a time as a month. This accelerated timing is often selected if waiting would result in a subsequent diminishment of egg quantity and quality. It is not typically recommended, though, to hurry into back-to-back cycles, because physical stress can compromise oocyte (egg) quality and affect results.
What if IVF Fails?
When IVF fails the first time, there is usually an emotional rollercoaster for couples. Understand that a failed cycle does not necessarily mean something is "wrong" with you—but it may indicate that further investigation is needed.
About 50–70% of implantation failure is due to chromosomal defects in the embryo. Other problems are due to poor development or inadequate lab conditions on the embryo side. On the maternal side, some causes of failure include uterine abnormalities such as fibroids or polyps, thin endometrium, or even immunological disorders.
"Sometimes" and even with" all" being "good quality eggs," "embryos," and "a healthy uterus," implantation just doesn't happen," explains Dr. Pavithra. "Those are termed idiopathic or unexplained cases." In these cases, additional testing would usually be carried out to detect any immunological reasons why" the body is rejecting the embryo, and treatment would be designed to curb overactive immune reactions.
Hormonal instability, endometriosis, blood clot disorders, and lifestyle factors such as smoking, alcohol drinking, or major weight concerns also contribute to outcomes. IVF involves considering the whole person, usually with lifestyle changes alongside medical treatments.
What Couples Should Expect?
IVF is not just a fertility treatment, it is a journey that is as much diagnostic as it is therapeutic. For several couples, IVF is the start of an understanding of their reproductive well-being. Even though pregnancy may not be achieved in the first try, the process provides insight into egg quality, sperm condition, and the body's reaction to assisted reproduction.
Couples have to enter this process educated and emotionally equipped. They need to be patient, resilient, and realistic. While science and medicine can lay out the route, the choice of when to begin, how many times to attempt, and when to stop or take a break is a highly personal decision.
Statistics reveal that the majority of successful IVF pregnancies happen during the first three to six cycles, but there can be variations depending on age, reason for infertility, and other medical factors. The process tends to be non-linear, and support in any form—whether from medical providers, therapists, or loved ones—can be the turning point.
Is There A "Perfect Timing"?
In the end, the optimal time to start IVF is not a number, but rather defined by personal health, relationship maturity, and life situation. For certain individuals, beginning in one's early 30s can be the highest likelihood of success. For others, IVF at an older age is still a viable and worthwhile option—particularly with newer developments such as egg freezing and donor assistance.
As Dr. Pavithra notes, "IVF is a journey of hope, science, and strength. It's crucial that couples don't lose hope with one or even more failed attempts. Every step brings us closer to knowing what the body needs to nourish new life."
© 2024 Bennett, Coleman & Company Limited

